X-linked Hypophosphatemia (XLH) may not be a household name, yet it profoundly impacts the lives of those affected. This rare genetic disorder disrupts phosphate metabolism, leading to various health challenges. Understanding XLH is crucial for patients, families, and healthcare professionals alike. With insights into its causes, symptoms, and treatment options, we can shed light on this often-misunderstood condition.
Living with X-linked Hypophosphatemia means navigating a complex landscape of skeletal abnormalities and dental complications that can emerge from early childhood through adulthood. As research continues to evolve in this field, staying informed about the latest advances in diagnosis and management strategies becomes increasingly important.
Join us as we explore the intricacies of X-linked Hypophosphatemia—its genetic basis and clinical manifestations—and discover how individuals cope with this condition while seeking ways to improve their quality of life. Let’s dive into understanding XLH together!
Understanding X-linked Hypophosphatemia Syndrome: An Overview
X-linked Hypophosphatemia is a genetic disorder primarily affecting phosphate metabolism. This condition arises due to mutations in the PHEX gene, which plays a crucial role in regulating phosphate levels in the body.
Phosphate is vital for bone health and energy production. In XLH, inadequate phosphate leads to weakened bones and skeletal deformities. Children with this syndrome often face challenges as they grow, including delayed growth and dental issues.
“Ablepharon Macrostomia Syndrome: What Causes These Facial Features?”
The inheritance pattern of XLH is X-linked dominant, meaning that it predominantly affects males while females can be carriers. Symptoms usually manifest in early childhood but may go undiagnosed for years if not recognized by healthcare professionals.
Understanding this syndrome’s complexities helps families seek appropriate care and support from specialists familiar with its unique challenges. As awareness increases, so does hope for improved management strategies for those living with X-linked Hypophosphatemia.
Genetic Basis of X-linked Hypophosphatemia Syndrome
X-linked Hypophosphatemia (XLH) is primarily linked to mutations in the PHEX gene. This gene plays a crucial role in phosphate metabolism and bone mineralization.
Located on the X chromosome, the PHEX gene’s dysfunction leads to impaired regulation of phosphate levels in the body. As a result, individuals with XLH experience low serum phosphate concentrations.
“How Does Alström Syndrome Affect Multiple Organs? Complete Guide”
The inheritance pattern of XLH is X-linked dominant. This means that both males and females can be affected, but males often exhibit more severe symptoms due to having only one X chromosome.
Understanding these genetic underpinnings helps inform diagnosis and treatment options for those impacted by this condition. Genetic counseling can provide valuable insights for families with a history of XLH, guiding them through potential risks and implications for future generations.
The Role of PHEX Gene Mutations in XLH
PHEX gene mutations are central to understanding X-linked Hypophosphatemia (XLH). The PHEX gene, located on the X chromosome, is crucial for phosphate regulation in the body. When this gene is mutated, it leads to a disruption in phosphate metabolism.
“What Causes Angelman Syndrome? Understanding ‘Happy Puppet’ Disorder”
This impairment results in decreased reabsorption of phosphate in the kidneys. Consequently, individuals with XLH experience hypophosphatemia—abnormally low levels of phosphate in the blood. Low phosphate can significantly impact bone mineralization and growth.
The severity of symptoms often correlates with specific mutations within the PHEX gene. Some mutations may cause milder forms of XLH while others lead to more pronounced clinical manifestations. Understanding these genetic variations aids healthcare providers in tailoring effective treatment plans for each patient.
Phosphate Metabolism and Its Disruption in XLH
Phosphate metabolism plays a crucial role in maintaining bone health and overall cellular function. In a healthy body, phosphate is absorbed through the intestines and regulated by hormones to ensure proper levels in the bloodstream.
“What Is Antiphospholipid Syndrome & Why Does It Cause Blood Clots?”
In individuals with X-linked Hypophosphatemia (XLH), this delicate balance is disrupted due to impaired renal phosphate reabsorption. The kidneys fail to retain adequate amounts of phosphate, leading to hypophosphatemia—an abnormally low level of phosphate in the blood.
This deficiency has significant repercussions on bone mineralization, as sufficient phosphate is essential for forming strong bones. As a result, patients often experience weakened skeletal structures and an increased risk of deformities and fractures over time.
Moreover, this metabolic imbalance impacts various physiological processes beyond bone health. The consequences extend into muscle function, energy production, and even tooth development as phosphorus plays vital roles across multiple systems within the body.
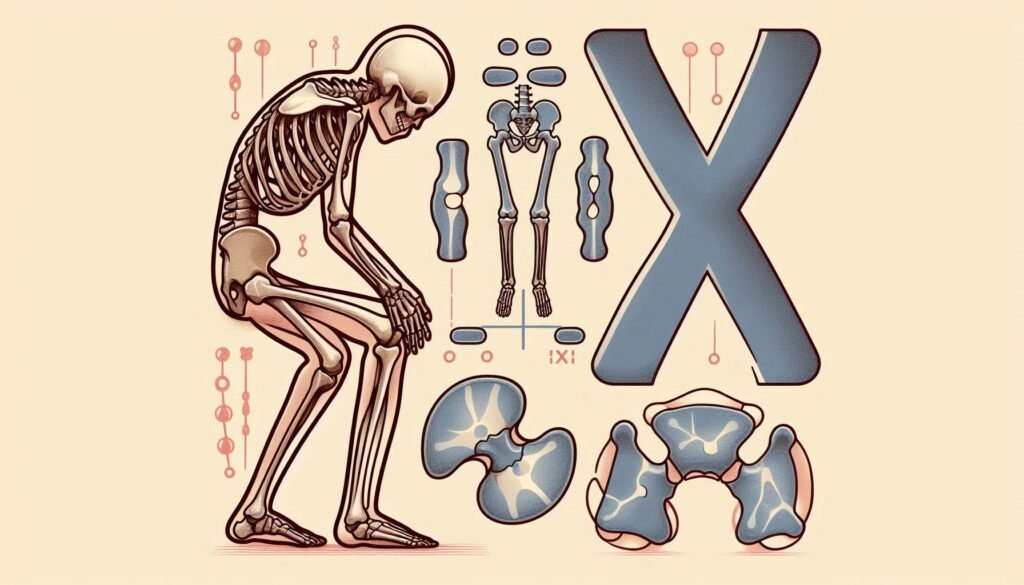
Clinical Manifestations of X-linked Hypophosphatemia Syndrome
X-linked Hypophosphatemia (XLH) presents a range of clinical manifestations primarily affecting the skeletal system. Patients often experience rickets, characterized by bone pain and deformities such as bowing of the legs. This condition typically emerges during early childhood.
“How Does Apert Syndrome Affect Skull Development? Complete Guide”
Growth deficiencies are common in XLH, leading to shorter stature compared to peers. The impact on physical development can be both emotional and psychological for affected children.
Dental issues frequently arise as well. Many individuals with XLH develop enamel defects, which increase vulnerability to cavities and other dental problems.
Joint pain is another significant concern, particularly in adulthood. As patients age, osteoarthritis may develop due to chronic stress on malformed bones and joints.
Understanding these clinical signs is crucial for timely intervention and management strategies that aim to improve quality of life for those living with XLH.
Skeletal Abnormalities Associated with XLH
X-linked Hypophosphatemia (XLH) is primarily characterized by skeletal abnormalities that can significantly affect an individual’s quality of life. One of the most common manifestations is rickets, a condition where bones become soft and weakened due to inadequate mineralization.
“What Causes Alport Syndrome? Understanding Hereditary Kidney Disease”
Patients may experience bowing of the legs, particularly during childhood as they grow. This deformity arises from the lack of phosphate needed for healthy bone development. In some cases, spinal curvature issues like scoliosis can also occur, leading to further complications in mobility.
Additionally, adults with XLH may suffer from osteomalacia—a softening of bones that increases fracture risk. These skeletal changes not only lead to physical challenges but can also impact self-esteem and emotional well-being as individuals navigate their daily lives with these conditions. Addressing these abnormalities early on through effective treatment options is crucial for improving outcomes in affected patients.
Dental Complications in Patients with XLH
Dental complications are common among individuals with X-linked Hypophosphatemia (XLH). These issues primarily arise due to the disorder’s impact on phosphate metabolism, which is crucial for maintaining healthy bones and teeth.
Patients often experience dental enamel hypoplasia. This condition results in thin or missing enamel, making teeth more susceptible to decay. As a result, dental caries can develop at an accelerated rate compared to those without XLH.
Additionally, patients may face delayed eruption of their permanent teeth. The timing and sequence of tooth emergence can be significantly altered. This situation leads to potential misalignment and other orthodontic concerns later on.
Periodontal disease also poses a risk for individuals with XLH. Poor bone health can contribute to gum problems, further complicating oral hygiene efforts. Regular dental check-ups are essential for early detection and management of these complications.
Diagnosis of X-linked Hypophosphatemia Syndrome
Diagnosing X-linked Hypophosphatemia (XLH) requires a thorough evaluation of clinical symptoms and biochemical tests. Healthcare providers often start with a detailed medical history, focusing on any musculoskeletal issues or dental problems.
Blood tests are crucial in identifying low phosphate levels and elevated alkaline phosphatase activity, which are common indicators of XLH. Additionally, urine tests can reveal excessive phosphate loss.
Genetic testing plays a significant role in confirming the diagnosis. This process identifies mutations in the PHEX gene responsible for this condition.
Differential diagnosis is important to rule out other disorders that cause similar symptoms, such as renal tubular acidosis or vitamin D deficiency rickets. A multidisciplinary approach may be beneficial, involving specialists like endocrinologists and genetic counselors for comprehensive care.
Genetic Testing and Counseling for XLH
Genetic testing plays a crucial role in diagnosing X-linked Hypophosphatemia (XLH). By examining the PHEX gene, healthcare providers can confirm the presence of mutations associated with this condition. This step is vital for establishing an accurate diagnosis and guiding treatment decisions.
Counseling is equally important for families affected by XLH. A genetic counselor can explain the implications of test results, including inheritance patterns and risks to future offspring. They help parents understand how XLH may impact their family’s health.
Furthermore, support from counselors assists families in coping with emotional challenges linked to a chronic condition. Knowledge gained through genetic counseling empowers patients and families to make informed choices regarding management options and family planning strategies tailored to their needs.
Differential Diagnosis: Distinguishing XLH from Other Phosphate Wasting Disorders
Differentiating X-linked Hypophosphatemia (XLH) from other phosphate wasting disorders requires careful evaluation. Several conditions can present with similar symptoms, making accurate diagnosis crucial.
One primary disorder to consider is Autosomal Dominant Hypophosphatemic Rickets (ADHR). Unlike XLH, ADHR is inherited in an autosomal dominant manner and often has a different biochemical profile.
Another condition to differentiate is Fanconi Syndrome, which involves generalized renal tubular dysfunction. While it also leads to phosphate loss, patients typically show additional electrolyte imbalances that are not characteristic of XLH.
Additionally, hypophosphatemic osteomalacia due to Vitamin D deficiency must be ruled out. This condition does not stem from genetic mutations but rather nutritional factors or malabsorption issues.
Clinicians may rely on genetic testing and biochemical markers like serum phosphorus levels for precise identification. Understanding these nuances helps ensure patients receive appropriate treatment tailored to their specific needs.
Treatment Approaches for X-linked Hypophosphatemia Syndrome
Treatment for X-linked Hypophosphatemia focuses on managing symptoms and improving quality of life. A multidisciplinary approach is essential, tailored to each patient’s needs.
Pharmacological management often includes phosphate supplements and active vitamin D analogs. These medications help regulate phosphate levels in the body, promoting better bone mineralization.
Surgical interventions may be necessary for patients with significant skeletal deformities. Procedures such as osteotomies can correct malformations and improve mobility.
Nutritional considerations also play a crucial role. Patients are advised to maintain a balanced diet rich in calcium and phosphorus while avoiding excessive intake of high-phosphate foods that could exacerbate complications.
Special attention is needed when treating children. Their growth patterns require careful monitoring to ensure optimal development alongside effective management strategies for XLH-related challenges. Regular follow-ups with healthcare providers enhance treatment efficacy and support patient well-being over time.
Pharmacological Management of XLH
Pharmacological management of X-linked hypophosphatemia (XLH) primarily focuses on increasing phosphate levels and improving bone health. The cornerstone treatment often involves oral phosphate supplements, which aim to elevate serum phosphate concentrations.
Additionally, active vitamin D analogs like calcitriol are frequently prescribed. These help enhance intestinal absorption of calcium and phosphorus. By doing so, they support better mineralization of bones in patients with XLH.
Recent advancements have introduced burosumab, a monoclonal antibody that inhibits fibroblast growth factor 23 (FGF23). This drug directly addresses the underlying cause by reducing FGF23 levels in the body, leading to improved phosphate metabolism.
Regular monitoring is crucial for all medications used in XLH management. Adjustments may be necessary based on patient response and potential side effects such as hypercalcemia or renal complications.
Surgical Interventions for XLH-related Skeletal Deformities
Surgical interventions can be crucial for addressing skeletal deformities associated with X-linked Hypophosphatemia (XLH). Patients often experience bowing of the legs, which can lead to pain and difficulty walking. Surgical correction aims to realign bones and improve function.
One common procedure is osteotomy. This involves cutting and reshaping the bone to restore normal alignment. Surgeons may use rods or plates for stabilization during recovery.
In more severe cases, limb lengthening techniques might be appropriate. These procedures gradually stretch the bone while allowing new bone tissue to form in the gap created.
Post-operative care is essential for optimal outcomes. Rehabilitation programs focus on restoring mobility and strength through targeted exercises. Multidisciplinary teams involving orthopedic surgeons, physical therapists, and nutritionists play a vital role in enhancing recovery after surgical intervention in XLH patients.
Nutritional Considerations for Patients with XLH
Nutritional considerations play a vital role in managing X-linked Hypophosphatemia (XLH). Patients often require a careful balance of nutrients to support bone health and overall well-being.
A diet rich in calcium is essential, as it helps improve bone density. Foods such as dairy products, leafy greens, and fortified alternatives are beneficial options.
Phosphate intake must be monitored closely. While some phosphate-rich foods can help maintain levels, excessive consumption may exacerbate symptoms. Consulting with a healthcare professional for personalized dietary guidance is crucial.
Vitamin D supplementation is also important for enhancing calcium absorption and promoting skeletal health. This nutrient aids in the regulation of phosphorus metabolism within the body.
Hydration should not be overlooked either; adequate fluid intake supports kidney function and overall metabolic processes that are critical for XLH management.
Managing XLH in Children: Special Considerations
Managing X-linked Hypophosphatemia (XLH) in children requires a tailored approach that addresses their unique developmental needs. Early diagnosis is crucial, enabling timely interventions to mitigate skeletal deformities.
Regular monitoring of phosphate levels and renal function helps guide treatment strategies. This often involves specific supplementation regimens aimed at improving bone health. Pediatric patients may need adjustments as they grow, making ongoing assessments essential.
Physical therapy plays a significant role in enhancing mobility and strength. Activities should be age-appropriate, focusing on safe engagement to encourage participation without risking injury.
Parents should also consider nutritional support. A well-balanced diet rich in phosphorus can aid overall management but must align with medical guidance to avoid excessive intake.
Emotional support is vital too; peer interactions help foster resilience in dealing with XLH challenges. Creating an open dialogue about the condition empowers children to understand their health better while promoting self-advocacy skills.
Long-term Prognosis and Quality of Life with XLH
The long-term prognosis for individuals with X-linked Hypophosphatemia (XLH) can vary widely. Many patients experience a spectrum of symptoms that can affect their quality of life significantly. Ongoing management is crucial to alleviate these challenges.
With appropriate treatment, including phosphate supplementation and active monitoring, many people lead fulfilling lives. However, skeletal deformities may persist into adulthood, necessitating surgical interventions.
Patients often face chronic pain and fatigue due to the condition’s impact on bone health. This can hinder physical activity and overall well-being. Mental health support becomes essential as well since living with XLH might lead to feelings of isolation or frustration.
Regular follow-ups with healthcare professionals are vital for managing complications effectively. With advances in research and therapy options, there is hope for improved outcomes and better quality of life for those affected by XLH moving forward.
Emerging Therapies and Research in X-linked Hypophosphatemia Syndrome
Recent advancements in the treatment of X-linked Hypophosphatemia (XLH) are promising. Researchers are exploring innovative therapies aimed at addressing the underlying genetic causes and improving patient outcomes.
One exciting development is the use of monoclonal antibodies targeting fibroblast growth factor 23 (FGF23). These agents can help restore normal phosphate levels, potentially alleviating some symptoms associated with XLH. Early clinical trials show favorable results, sparking interest in their long-term efficacy.
Gene therapy is another area gaining traction. Investigators are evaluating methods to correct PHEX gene mutations responsible for XLH. This approach could offer a more permanent solution rather than just managing symptoms.
Ongoing studies also focus on optimizing dietary interventions and supplements that enhance phosphate absorption. The integration of these modalities may provide comprehensive management strategies for patients living with XLH.
Living with XLH: Patient Experiences and Coping Strategies
Living with X-linked Hypophosphatemia (XLH) presents unique challenges for patients and their families. Many individuals share experiences of navigating frequent medical appointments, managing symptoms, and adjusting to the emotional toll on daily life.
Support networks often play a crucial role. Connecting with others who have XLH can provide valuable insights and encouragement. Online forums and local support groups offer a safe space for sharing stories and coping strategies.
Patients frequently emphasize the importance of education. Understanding their condition empowers them to make informed decisions about treatment options, lifestyle changes, and self-care routines.
Engaging in physical therapy is another common strategy. Tailored exercises help improve mobility while reducing pain associated with skeletal abnormalities.
Additionally, maintaining open communication with healthcare providers fosters trust. This collaboration ensures that individual needs are addressed effectively as they evolve through different life stages.
Future Directions in XLH Research and Treatment
Research on X-linked Hypophosphatemia (XLH) is advancing rapidly, and the future holds promise for improved outcomes for those affected by this condition. Ongoing studies are focusing on understanding the intricate mechanisms behind PHEX gene mutations and their impact on phosphate metabolism. This knowledge can lead to targeted therapies that could enhance treatment efficacy.
Emerging treatments, such as monoclonal antibodies aimed at regulating phosphate homeostasis, show potential in clinical trials. These innovative approaches may offer new hope for patients who currently rely heavily on traditional management strategies.
Additionally, advancements in genetic testing will allow for earlier diagnosis and personalized care plans tailored to individual patient needs. Genetic counseling services are also expanding, providing families with crucial information about inheritance patterns and implications.
Longitudinal studies tracking XLH patients over time will help researchers gather valuable data regarding long-term health outcomes and quality of life measures. By analyzing these insights, better supportive care practices can be developed.
As awareness increases within both medical communities and among the public, advocacy efforts are promoting funding for research initiatives focused on XLH. Collaboration between researchers, healthcare providers, and patient advocacy groups will drive innovation forward.
The horizon looks bright for individuals living with X-linked Hypophosphatemia as we embrace a future filled with possibilities in research breakthroughs and enhanced therapeutic options designed specifically to improve lives impacted by this rare disease.


