Paraneoplastic syndromes are fascinating yet complex phenomena that occur in some cancer patients. They reflect the body’s response to cancer rather than the direct effects of a tumor. This means that even when there is no visible evidence of disease progression, individuals can experience various symptoms related to these syndromes. Understanding paraneoplastic syndrome is crucial for early diagnosis and effective management.
As we delve into this topic, you’ll discover how these syndromes manifest across different systems in the body, from neurological issues to endocrine disturbances. With emerging research and treatment options on the horizon, being informed can empower both patients and caregivers alike. Join us as we explore what you need to know about paraneoplastic syndromes!
Understanding Paraneoplastic Syndromes: An Overview
Paraneoplastic syndromes are rare disorders triggered by cancer’s presence in the body. These syndromes occur when the immune system reacts to a tumor, leading to symptoms that can affect various organ systems. Interestingly, these manifestations can arise even before a cancer diagnosis is made.
The term “paraneoplastic” refers to effects that are not directly caused by tumor invasion or metastasis but rather result from biological processes initiated by tumors. This makes understanding paraneoplastic syndrome essential for early detection and intervention.
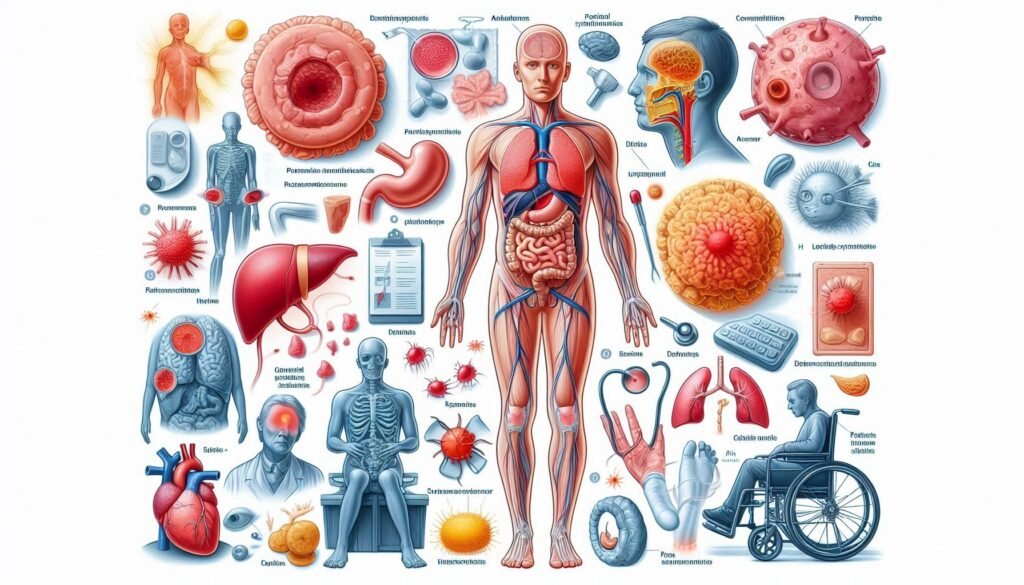
Symptoms may vary widely, impacting neurological function, hormonal balance, and skin health. Awareness of these syndromes can significantly improve patient outcomes through timely diagnosis and treatment options.
Types of Paraneoplastic Syndromes: Neurological, Endocrine, and Others
Paraneoplastic syndromes manifest in various forms, primarily categorized into neurological and endocrine types. Neurological paraneoplastic syndromes often present with symptoms like muscle weakness, seizures, or cognitive changes. These occur when the immune system reacts to cancer cells affecting nervous tissue.
“What Is Abruzzo-Erickson Syndrome? Understanding This Rare Genetic Condition”
Endocrine paraneoplastic syndromes involve hormone imbalances due to tumor secretions. For instance, some tumors can produce hormones that lead to conditions like Cushing’s syndrome or hypercalcemia.
Beyond these categories, other manifestations include dermatological issues and hematological disorders. Each type presents unique challenges for diagnosis and treatment but is crucial in understanding the broader effects of malignancies on overall health.
Pathophysiology: Immune-Mediated Mechanisms
Paraneoplastic syndromes often arise due to immune-mediated mechanisms triggered by malignancies. The immune system can mistakenly attack normal tissues after recognizing tumor-associated antigens. This response leads to a variety of neurological, endocrine, and other dysfunctions.
Autoantibodies play a crucial role in these processes. They target specific proteins within healthy cells, disrupting normal cellular functions. As a result, patients may experience symptoms that seem unrelated to their underlying cancer.
“Achard-Thiers Syndrome: Why Does It Cause Diabetes & Hirsutism in Women?”
Additionally, cytokines released from tumors can further exacerbate these responses. These signaling molecules impact various body systems and contribute to the diverse manifestations of paraneoplastic syndromes observed in affected individuals.
Common Cancers Associated with Paraneoplastic Syndromes
Paraneoplastic syndromes often accompany various malignancies, affecting many organ systems. Lung cancer is one of the most commonly associated cancers, frequently linked to neurological and endocrine manifestations. Small cell lung carcinoma, in particular, can lead to severe paraneoplastic complications.
Breast cancer also presents several paraneoplastic syndromes. These may include autoimmune phenomena that result in neurological symptoms or skin changes.
“What Causes ARDS (Acute Respiratory Distress Syndrome)? Complete Guide”
Hematological cancers like lymphoma and leukemia are significant contributors as well. They can provoke a range of immune-mediated responses leading to disorders such as hypercoagulability and anemia, which complicate patient management further.
Neurological Paraneoplastic Syndromes: Symptoms and Diagnosis
Neurological paraneoplastic syndromes occur when cancer triggers immune responses that affect the nervous system. Patients may experience a range of symptoms, including muscle weakness, seizures, memory loss, and coordination difficulties. These manifestations can vary significantly based on the specific syndrome.
Diagnosis involves a thorough clinical evaluation and neurological examination. Physicians often rely on patient history and symptom presentation to guide their assessments. Additional tests like MRI scans or lumbar punctures can help identify inflammation or other abnormalities in the central nervous system.
“How Does Adams-Oliver Syndrome Affect Development? Expert Explained”
Autoantibodies are frequently detected in these patients, providing crucial diagnostic clues. Identifying these antibodies can link neurological symptoms to an underlying malignancy effectively.
Endocrine Paraneoplastic Syndromes: Clinical Presentations
Endocrine paraneoplastic syndromes occur when tumors produce hormones or hormone-like substances, leading to significant clinical manifestations. One common example is the ectopic production of adrenocorticotropic hormone (ACTH), which can cause Cushing’s syndrome. Patients may experience weight gain, hypertension, and glucose intolerance.
Another notable condition is hypercalcemia due to parathyroid hormone-related peptide (PTHrP) secretion from malignancies such as lung cancer. This results in elevated calcium levels, causing symptoms like fatigue, nausea, and confusion.
“What Is Adie Syndrome & Why Does It Affect Your Pupils? Complete Guide”
Moreover, insulinomas can lead to episodes of hypoglycemia from excess insulin release. Symptoms may include sweating, tremors, and altered consciousness. Early recognition of these syndromes is crucial for effective management.
Dermatological Manifestations of Paraneoplastic Syndromes
Dermatological manifestations of paraneoplastic syndromes can vary significantly among patients. These skin-related symptoms often indicate an underlying malignancy and may precede the diagnosis of cancer. Common conditions include dermatomyositis, characterized by a distinctive rash and muscle weakness.
Other skin changes may present as pruritic papules or erythematous plaques, which signal immune system involvement. The relationship between these dermatological signs and specific cancers is vital for early detection.
“Why Does Alice in Wonderland Syndrome Make Things Look Different? Guide”
Recognizing these cutaneous clues can prompt further investigation into possible malignancies. Dermatologists play a crucial role in identifying these manifestations, helping to facilitate timely medical intervention before more serious complications arise.
Hematological Paraneoplastic Disorders
Hematological paraneoplastic disorders are blood-related conditions triggered by underlying malignancies. These syndromes can affect red and white blood cells, platelets, and coagulation factors. They often manifest as anemia, thrombocytopenia, or hypercoagulability.
Patients may experience symptoms like fatigue, easy bruising, or excessive bleeding. The connection between cancer and these hematological issues can complicate diagnosis since the signs might be mistaken for treatment side effects or other medical conditions.
Understanding the link between these disorders and specific cancers is essential for effective management. Timely identification of hematological disturbances allows healthcare providers to tailor treatments that address both the cancer and its associated complications more effectively.
Rheumatological Paraneoplastic Syndromes
Rheumatological paraneoplastic syndromes are immune-mediated conditions that arise due to malignancies. These syndromes often present as joint pain, muscle weakness, or systemic autoimmune features. Patients may experience symptoms like myositis, polyarthritis, and even vasculitis.
Common cancers associated with rheumatological manifestations include lung cancer and lymphomas. The connection between these malignancies and rheumatological symptoms highlights the complexity of cancer’s impact on the body’s immune response.
Diagnosing these syndromes requires a detailed clinical evaluation. Medical history, physical examinations, and laboratory tests help identify underlying malignancies while differentiating them from primary autoimmune disorders. Timely recognition is crucial in managing both the cancer and its related complications effectively.
Diagnostic Approach: Identifying Underlying Malignancies
A comprehensive diagnostic approach is crucial for identifying underlying malignancies in patients with paraneoplastic syndrome. Initial evaluations often include a detailed medical history and thorough physical examination. Physicians pay close attention to any unusual symptoms or signs that may suggest cancer.
Laboratory tests are typically performed, including complete blood counts and metabolic panels. Imaging studies such as CT scans, MRIs, or PET scans can help visualize potential tumors throughout the body.
Endoscopic procedures may also be utilized to obtain tissue samples for biopsy. Identifying the primary cancer is essential for effective treatment planning and addressing both the malignancy and its associated paraneoplastic effects.
Role of Autoantibodies in Paraneoplastic Syndromes
Autoantibodies play a crucial role in paraneoplastic syndromes. These antibodies are produced by the immune system in response to cancer cells, mistakenly targeting normal tissues instead. This aberrant immune response can lead to various neurological and systemic symptoms.
The presence of specific autoantibodies often helps identify underlying malignancies. Tests for these markers can be pivotal for early diagnosis. For instance, anti-CRMP-1 is associated with lung cancer-related neurological manifestations.
Understanding the relationship between autoantibodies and paraneoplastic syndromes enhances our grasp of disease mechanisms. It opens pathways for tailored therapeutic approaches and better patient outcomes, emphasizing the connection between the immune system and cancer progression.
Imaging Techniques in Paraneoplastic Syndrome Evaluation
Imaging techniques play a crucial role in the evaluation of paraneoplastic syndrome. These methods help identify underlying malignancies that may be causing the unusual symptoms. Common imaging modalities include CT scans, MRI, and PET scans.
CT scans provide detailed cross-sectional images of the body, allowing for effective tumor localization. MRI is particularly useful for assessing neurological manifestations associated with these syndromes. It offers high-resolution images of brain structures.
PET scans are valuable in detecting metabolic activity within tissues, helping to pinpoint cancerous growths. Each technique contributes uniquely to a comprehensive assessment, guiding clinicians toward appropriate diagnosis and management options tailored to individual patients’ needs.
Treatment Strategies: Addressing the Underlying Cancer
Effective treatment of paraneoplastic syndrome hinges on addressing the underlying cancer. Identifying and controlling the primary malignancy often alleviates associated symptoms. Treatment options may include surgical intervention, chemotherapy, or radiation therapy.
Targeted therapies are also gaining traction in managing specific cancers linked to paraneoplastic syndromes. These precision approaches aim to interrupt the disease process more effectively than traditional treatments.
In some cases, immunotherapy shows promise by harnessing the body’s immune system against cancer cells while potentially mitigating paraneoplastic effects. Collaborating with an oncologist ensures a personalized treatment plan tailored to both the cancer type and patient needs.
Immunotherapy in Paraneoplastic Syndromes
Immunotherapy has emerged as a promising treatment for paraneoplastic syndromes. This approach harnesses the body’s immune system to target cancer cells, potentially reducing tumor burden and alleviating associated symptoms.
Different immunotherapeutic strategies include checkpoint inhibitors, monoclonal antibodies, and CAR T-cell therapy. These treatments aim to enhance the immune response against malignancies linked with paraneoplastic syndromes.
Clinical trials are investigating how effective these therapies can be in managing both the underlying cancers and their neurological or endocrine manifestations. Early results indicate that immunotherapy might not only help treat cancer but also improve patient quality of life by addressing related symptoms more effectively.
Symptomatic Management of Paraneoplastic Manifestations
Symptomatic management of paraneoplastic manifestations focuses on alleviating discomfort and improving quality of life. Patients may experience a range of symptoms, including pain, neurological issues, or hormonal imbalances. Each symptom requires tailored strategies to ensure effective relief.
Pain management is often prioritized, utilizing non-opioid analgesics or opioids when necessary. Neurological symptoms might be addressed with medications that target specific disorders like seizures or movement abnormalities.
Hormonal therapies can help regulate endocrine-related symptoms resulting from tumors influencing hormone levels. Integrating multidisciplinary care ensures comprehensive support for patients suffering from these complex conditions while addressing both physical and emotional needs.
Prognosis and Long-term Outcomes
The prognosis for patients with paraneoplastic syndrome often depends on the underlying malignancy. Early detection and treatment of the associated cancer can significantly improve outcomes. When cancers are diagnosed at an advanced stage, the prognosis may be less favorable.
Long-term outcomes vary widely among individuals. Some patients experience remission of both their cancer and paraneoplastic symptoms after appropriate treatment, while others may face persistent challenges related to neurological or endocrine dysfunctions.
Ongoing monitoring is crucial for managing potential relapses or new complications arising from either the malignancy or its sequelae. Supportive care plays a vital role in enhancing quality of life during this journey.
Challenges in Diagnosis and Treatment
Diagnosing paraneoplastic syndrome can be challenging due to its diverse presentation. Symptoms often mimic other conditions, leading to misdiagnosis. Many healthcare providers may overlook the possibility of an underlying malignancy.
The indirect nature of these syndromes complicates treatment strategies. Physicians must not only manage symptoms but also address the primary cancer effectively. This dual focus requires a multidisciplinary approach.
Additionally, limited awareness among practitioners regarding paraneoplastic syndromes contributes to delayed diagnoses and treatments. As a result, patients may experience prolonged suffering before receiving appropriate care tailored to their unique needs.
Emerging Therapies and Clinical Trials
Emerging therapies for paraneoplastic syndromes are gaining attention in the medical community. Researchers are exploring novel immunotherapies that target specific autoantibodies associated with these conditions. By modulating the immune response, there is potential to alleviate symptoms while addressing underlying malignancies.
Clinical trials are crucial for evaluating the effectiveness of new treatments. These studies often focus on personalized medicine approaches, tailoring therapies based on individual tumor characteristics and patient profiles. Participation in such trials may offer patients access to cutting-edge interventions.
Furthermore, advancements in biomarker research provide insights into disease mechanisms. Understanding these pathways allows for more targeted treatment strategies, paving the way for improved outcomes in those affected by paraneoplastic syndromes.
Patient Education and Support
Patient education is crucial for those diagnosed with paraneoplastic syndromes. Understanding the syndrome helps patients recognize symptoms that may indicate an underlying malignancy. This knowledge empowers them to seek timely medical attention.
Support systems play a significant role in patient care. Connecting with healthcare professionals, support groups, and counseling services can alleviate anxiety and provide valuable resources for coping with the emotional burden of these conditions.
Resources such as educational materials, online forums, and workshops are beneficial. These platforms offer insights into managing symptoms and navigating treatment options while fostering a sense of community among individuals facing similar challenges.
Future Directions in Paraneoplastic Syndrome Research
Future research in paraneoplastic syndrome is focused on several key areas. Understanding the underlying mechanisms will enhance our knowledge of these complex syndromes. Researchers are exploring genetic factors that may predispose individuals to develop paraneoplastic manifestations.
Additionally, studies aim to identify specific autoantibodies associated with different malignancies and their respective syndromes. This could lead to more precise diagnostic tools and early detection strategies.
As treatments evolve, there’s a growing interest in personalized therapies targeting individual immune responses. Ongoing clinical trials are investigating new immunotherapeutic options that can provide better outcomes for patients.
Collaboration among oncologists, neurologists, and researchers is essential for advancing this field. As awareness increases, so does the potential for improved patient care through targeted interventions and support systems tailored specifically for those affected by paraneoplastic syndromes.


