Sleep is meant to be a time for rest and rejuvenation, but for many, it can be anything but peaceful. Obstructive Sleep Apnea Syndrome (OSAS) disrupts sleep patterns and compromises overall health in ways that extend far beyond the bedroom. This common yet often overlooked condition leads to serious consequences that affect daily life, mood, and even long-term health outcomes.
Understanding OSAS is crucial for anyone who snores or experiences excessive daytime sleepiness. Did you know that untreated sleep apnea can increase your risk of cardiovascular disease or diabetes? As we delve into this complex topic, you’ll discover how obstructive sleep apnea may impact your quality of life and what steps you can take toward better health. Whether you suspect you might have OSAS or are simply interested in learning more, this guide aims to shed light on the broader implications of disrupted breathing during sleep.
Obstructive Sleep Apnea Syndrome: Understanding Sleep-Disordered Breathing
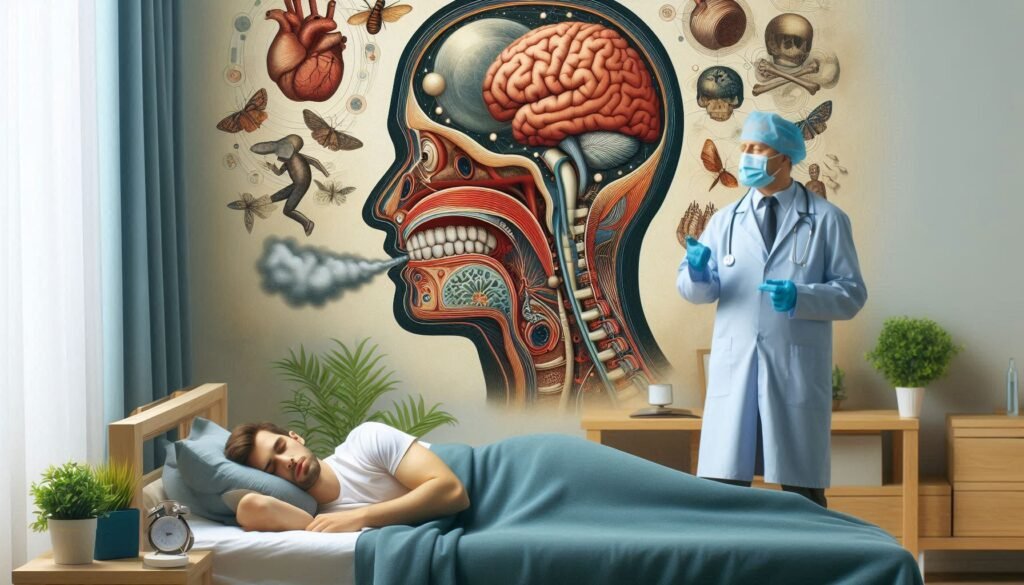
Obstructive Sleep Apnea Syndrome (OSAS) is a prevalent disorder characterized by repeated episodes of upper airway obstruction during sleep. These interruptions can last from a few seconds to minutes, resulting in fragmented sleep and decreased oxygen levels in the blood.
People with OSAS often experience loud snoring, choking, or gasping sounds as they wake briefly throughout the night. This leads not only to poor rest but also excessive daytime drowsiness and fatigue.
“Why Does Van der Woude Syndrome Cause Cleft Lip?”
The condition affects individuals across various age groups and demographics. However, it remains underdiagnosed due to misconceptions about its seriousness. Awareness of OSAS and its symptoms is vital for timely intervention and management to improve overall health outcomes.
Pathophysiology: Upper Airway Collapse and Its Consequences
Obstructive Sleep Apnea Syndrome (OSA) primarily stems from the collapse of the upper airway during sleep. This occurs when throat muscles relax excessively, obstructing airflow. The result is interrupted breathing patterns that can last for seconds to minutes.
“How Does Variably Protean Syndrome Present?”
As oxygen levels drop, the body reacts by briefly waking up to restore breathing. These frequent awakenings disrupt sleep cycles, leading to fragmented and non-restorative sleep. Consequently, individuals may experience daytime fatigue and decreased cognitive performance.
Moreover, repeated episodes of hypoxia can trigger a cascade of physiological responses. Increased heart rate and elevated blood pressure are common consequences, which can contribute to long-term cardiovascular issues if left unaddressed. Understanding this pathophysiology is crucial for recognizing OSA’s far-reaching health impacts.
Risk Factors: Obesity, Anatomy, and Other Predisposing Conditions
Obstructive Sleep Apnea Syndrome often intertwines with various risk factors, making it crucial to understand these connections. Obesity stands out as a significant contributor. Excess weight can lead to fat deposits around the neck and throat, increasing airway obstruction during sleep.
Anatomical features also play a vital role in OSA development. A thick neck, enlarged tonsils, or a recessed jaw can alter airflow dynamics, exacerbating the condition. Individuals with such anatomical predispositions are at increased risk.
“What Causes Valentine Syndrome? Heart Condition Guide”
Other conditions like age and gender further contribute to susceptibility. Men are generally more affected than women until menopause alters this trend. Additionally, certain medical conditions—such as diabetes and hypertension—can elevate the likelihood of developing obstructive sleep apnea syndrome.
Clinical Presentation: Snoring, Daytime Sleepiness, and Associated Symptoms
Individuals with obstructive sleep apnea syndrome often present with loud snoring, a hallmark symptom. This snoring is typically punctuated by periods of silence when breathing stops due to airway obstruction. These interruptions can be alarming for bed partners and lead to disrupted sleep cycles.
“Why Does Vanishing White Matter Syndrome Progress?”
Daytime sleepiness is another common complaint among those affected. The fragmented sleeping pattern results in insufficient restorative sleep, leaving individuals feeling fatigued throughout the day. This excessive daytime drowsiness can impair daily functioning.
Associated symptoms may include morning headaches, irritability, and difficulty concentrating. Patients might also experience dry mouth or sore throat upon waking due to breathing difficulties at night. Recognizing these signs early on is crucial for effective intervention and management of this condition.
Diagnostic Criteria: Polysomnography and Home Sleep Testing
Polysomnography is the gold standard for diagnosing obstructive sleep apnea syndrome. This comprehensive overnight test records brain activity, oxygen levels, heart rate, and breathing patterns. Conducted in a sleep lab, it provides detailed insights into your sleep stages and any disruptions.
“How Does VATER Syndrome Affect Multiple Systems?”
Home sleep testing offers a convenient alternative for some patients. This simpler approach uses portable devices to monitor sleep-related metrics like airflow and respiratory effort. While it’s less thorough than polysomnography, it can still effectively identify moderate to severe cases of OSA.
Both methods require careful interpretation by trained specialists. Accurate diagnosis ensures tailored treatment plans that address individual needs and improve overall health outcomes related to obstructive sleep apnea syndrome.
Cardiovascular Complications: Hypertension, Arrhythmias, and Heart Disease
Obstructive Sleep Apnea Syndrome significantly impacts cardiovascular health. Individuals suffering from this condition often experience hypertension, as the repeated interruptions in breathing cause fluctuations in oxygen levels. These variations trigger stress responses that can elevate blood pressure over time.
“What Are The Signs of Waardenburg Syndrome?”
Arrhythmias are another serious concern. The irregular breathing patterns associated with sleep apnea may lead to disturbances in heart rhythm, increasing the risk of atrial fibrillation and other types of arrhythmias. This can contribute to a heightened chance of stroke or other complications.
Heart disease is also linked to untreated obstructive sleep apnea syndrome. Chronic low oxygen levels strain the heart muscle, leading to conditions such as left ventricular hypertrophy and heart failure if not addressed promptly. Understanding these risks is crucial for effective management and treatment.
Metabolic Impact: Insulin Resistance and Type 2 Diabetes
Obstructive Sleep Apnea Syndrome significantly impacts metabolic health, particularly through insulin resistance. Inadequate sleep disrupts the body’s ability to regulate glucose levels, leading to higher blood sugar concentrations.
Research indicates that individuals with OSA are more likely to develop type 2 diabetes due to these metabolic changes. The repeated nighttime awakenings cause hormonal imbalances that affect how the body responds to insulin.
Furthermore, chronic inflammation linked with OSA may exacerbate insulin sensitivity issues. As a result, managing sleep apnea is crucial for preventing or controlling diabetes and improving overall health outcomes in affected individuals. Addressing this condition can lead to substantial benefits beyond just better sleep quality.
Neurocognitive Effects: Memory, Concentration, and Mood Disorders
Obstructive Sleep Apnea Syndrome (OSA) significantly impacts neurocognitive functions. Individuals often experience memory issues due to disrupted sleep patterns. The brain requires restorative sleep to process and consolidate information, which OSA can hinder.
Concentration is also affected. Many people with OSA report difficulties focusing during the day, leading to decreased productivity at work or school. This impairment can be frustrating and may exacerbate feelings of inadequacy.
Mood disorders are another consequence worth noting. Chronic fatigue and irritability commonly accompany sleep apnea, increasing the risk of anxiety and depression. These emotional challenges can create a vicious cycle, further complicating both mental health and overall wellbeing in those affected by this condition.
Pediatric Sleep Apnea: Unique Features and Management
Pediatric sleep apnea presents unique challenges distinct from adult cases. The condition often stems from enlarged tonsils or adenoids, which can obstruct airflow during sleep. Children may exhibit symptoms such as restless sleep, bedwetting, and difficulty waking up.
Diagnosis typically involves a thorough evaluation by a pediatrician or sleep specialist. Polysomnography is the gold standard for confirming obstructive sleep apnea syndrome in children. It helps assess the severity of the condition and guides treatment options.
Management strategies often include lifestyle modifications like weight loss and avoiding allergens that could exacerbate symptoms. In many cases, surgical intervention to remove enlarged tonsils or adenoids proves effective in restoring normal breathing patterns during sleep.
Treatment Options: CPAP, Oral Appliances, and Lifestyle Modifications
Continuous Positive Airway Pressure (CPAP) therapy is the gold standard for treating Obstructive Sleep Apnea Syndrome. This device delivers a steady stream of air, keeping the airway open during sleep. While effective, some users find it uncomfortable or struggle with compliance.
Oral appliances are another option for mild to moderate cases. These custom-fitted devices reposition the jaw and tongue to maintain an open airway. They can be a more comfortable alternative for those who cannot tolerate CPAP.
Lifestyle modifications play a crucial role as well. Weight loss can significantly reduce OSA severity, while avoiding alcohol and sedatives helps prevent airway collapse during sleep. Incorporating regular exercise also contributes positively to overall health and well-being.
Surgical Interventions: Types and Indications for OSA
Surgical interventions for Obstructive Sleep Apnea Syndrome (OSA) are considered when non-invasive treatments fail or in specific anatomical cases. Common procedures include uvulopalatopharyngoplasty (UPPP), which removes excess tissue from the throat, and genioglossus advancement, aimed at repositioning the tongue muscle to prevent airway collapse.
Another option is maxillomandibular advancement, where both upper and lower jaw are repositioned forward to enlarge the airway. This technique often benefits those with structural abnormalities contributing to OSA.
In some instances, a hypoglossal nerve stimulator may be implanted. It stimulates the tongue muscles during sleep to keep the airway open. Each surgical choice hinges on patient-specific anatomy and severity of symptoms, requiring thorough evaluation by a sleep specialist.
Weight Management: Role of Diet and Exercise in OSA
Weight management plays a crucial role in managing obstructive sleep apnea syndrome (OSA). Excess weight, particularly around the neck, can increase airway obstruction during sleep. Losing even a small percentage of body weight can significantly improve airflow and reduce symptoms.
Dietary choices also impact sleep quality. A balanced diet rich in fruits, vegetables, lean proteins, and whole grains supports overall health and aids in weight loss. Avoiding heavy meals before bedtime helps prevent disruptions during sleep.
Regular exercise is essential for maintaining a healthy weight and enhancing respiratory function. Activities like walking, swimming, or cycling not only promote fat loss but also strengthen muscles involved in breathing. This holistic approach fosters better sleep hygiene and overall well-being for those with OSA.
Positional Therapy: Techniques to Reduce Supine Sleep
Positional therapy is a non-invasive approach to managing obstructive sleep apnea syndrome (OSA), particularly for those who experience more severe symptoms when sleeping on their backs. This method encourages patients to adopt side-sleeping positions, which can help keep the airway open during rest.
Various techniques are available to facilitate this change in sleeping posture. For instance, specialized pillows or cushions can be used to promote comfortable side-sleeping. Additionally, some individuals find success with wearable devices that vibrate or alarm them when they roll onto their back.
This simple adjustment may significantly reduce snoring and apnea events for many patients. By focusing on positional changes during sleep, individuals can improve their overall health and well-being while minimizing OSA complications.
Comorbid Conditions: Managing OSA with Other Sleep Disorders
Obstructive Sleep Apnea Syndrome often coexists with other sleep disorders, complicating diagnosis and treatment. Conditions like insomnia or restless leg syndrome can exacerbate the symptoms of OSA, leading to a cycle of poor sleep quality. This dual impact makes it crucial for healthcare providers to consider all aspects of a patient’s sleep health.
Managing these comorbid conditions involves a comprehensive approach. Cognitive-behavioral therapy (CBT) may help address underlying anxiety that contributes to insomnia while improving overall sleep hygiene practices.
Additionally, treating OSA effectively through CPAP or oral appliances can alleviate some symptoms associated with other disorders, creating a more manageable nighttime experience for patients facing multiple challenges in their quest for restorative sleep.
Quality of Life: Impact on Daily Functioning and Relationships
Obstructive Sleep Apnea Syndrome significantly impacts quality of life. Individuals often experience excessive daytime sleepiness, affecting their ability to focus and perform daily tasks. This can lead to decreased productivity at work or school.
Relationships may also suffer due to irritability and mood swings associated with poor sleep quality. Partners may find themselves dealing with loud snoring or frequent awakenings during the night, causing strain in the relationship.
Social activities might take a backseat as fatigue makes it challenging to maintain an active lifestyle. People affected by OSA may withdraw from friends and family, further enhancing feelings of isolation and frustration over time. Understanding these effects is crucial for effective management strategies that support both health and interpersonal connections.
Occupational Considerations: OSA in Commercial Drivers and Shift Workers
Obstructive Sleep Apnea Syndrome (OSA) poses significant risks for commercial drivers and shift workers. These individuals often face irregular sleep patterns, making them more susceptible to excessive daytime sleepiness. This can lead to impaired alertness, increasing the risk of accidents on the road or in demanding work environments.
For commercial drivers, OSA is not just a health concern; it’s a safety issue. Regulatory bodies require testing for sleep apnea among operators who exhibit symptoms like loud snoring or persistent fatigue. Failure to address OSA can result in license suspension and legal liabilities.
Shift workers also struggle with maintaining consistent sleep schedules due to their unique hours. This disruption can exacerbate OSA symptoms, leading to decreased productivity and increased errors at work.
Latest Research: Emerging Therapies and Personalized Medicine
Recent research in obstructive sleep apnea syndrome (OSA) is uncovering innovative therapies aimed at improving patient outcomes. Advances in personalized medicine allow for tailored treatment plans that consider individual anatomy and comorbidities. This shift enhances the effectiveness of interventions.
New pharmacological options are under investigation, focusing on stimulating upper airway muscles during sleep to prevent collapse. These emerging drugs offer hope for patients who struggle with traditional methods like CPAP.
Additionally, ongoing studies explore genetic factors influencing OSA severity and response to treatment. Understanding these aspects could lead to customized approaches that significantly improve compliance and overall quality of life for those affected by this complex condition.
Patient Education: Improving CPAP Compliance and Long-term Management
Patient education is essential for improving compliance with CPAP therapy and ensuring effective long-term management of Obstructive Sleep Apnea Syndrome. Understanding the condition can empower patients to engage actively in their treatment journey.
Patients should receive comprehensive information about how CPAP works, its benefits, and potential side effects. Highlighting the importance of regular use can help demystify any initial discomfort associated with wearing a CPAP mask during sleep.
Support groups or educational sessions may further enhance understanding and provide motivation. Encouraging open communication between healthcare providers and patients fosters trust and addresses concerns promptly.
Moreover, continuous follow-up appointments are critical to monitor progress and make necessary adjustments to therapy settings. By equipping patients with knowledge and resources, we pave the way for better adherence to treatment plans, ultimately enhancing quality of life for those affected by obstructive sleep apnea syndrome.