Neurocutaneous Melanosis Syndrome is a rare congenital disorder that combines skin and neurological complications, often leaving families searching for answers. This condition can be perplexing due to its unique combination of symptoms and the challenges it presents. With large congenital melanocytic nevi appearing on the skin, individuals may also face serious neurological issues such as seizures or developmental delays. Navigating this complex syndrome requires understanding both medical aspects and emotional support systems.
In this comprehensive guide, we aim to shed light on Neurocutaneous Melanosis Syndrome—its causes, features, diagnostic methods, management strategies, and more. Whether you are a patient or a family member affected by this condition, our goal is to provide valuable insights that empower you with knowledge about living with Neurocutaneous Melanosis Syndrome.
Neurocutaneous Melanosis Syndrome: A Rare Congenital Disorder
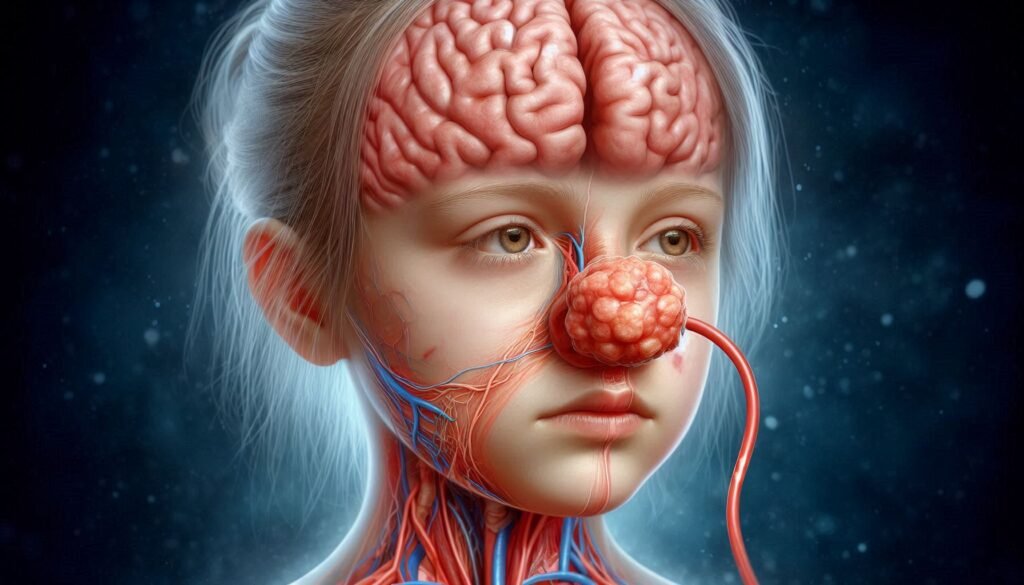
Neurocutaneous Melanosis Syndrome is an uncommon congenital disorder characterized by the presence of large pigmented skin lesions and central nervous system involvement. It typically arises from abnormalities during neural crest cell development, leading to abnormal melanocyte migration.
“Why Does Ullrich Congenital Muscular Dystrophy Affect Muscles?”
This syndrome manifests primarily in infants and young children, with cutaneous melanocytic nevi being a hallmark feature. These nevi can vary in size, shape, and color, often appearing at birth or shortly thereafter.
Beyond its visible signs on the skin, Neurocutaneous Melanosis Syndrome poses significant neurological risks. Affected individuals may experience complications that impact their cognitive development and overall quality of life. Understanding this condition is crucial for providing appropriate care and support for those affected.
Pathogenesis: Neural Crest Cell Abnormalities and Melanocyte Migration
Neurocutaneous Melanosis Syndrome arises from abnormalities in neural crest cells, which play a crucial role during embryonic development. These cells give rise to various structures, including melanocytes responsible for skin pigmentation. When migration of these cells is disrupted, it can lead to the formation of abnormal lesions.
“How Does Ulrich-Noonan Syndrome Impact Development?”
Melanocyte migration typically occurs along specific pathways in the developing embryo. If this process is impaired, melanocytes may accumulate abnormally in both the skin and central nervous system. This results in characteristic cutaneous nevi and potential CNS involvement.
Understanding this pathogenesis helps researchers identify how these disruptions occur early in development. Further exploration into neural crest cell behavior could illuminate new avenues for treatment or prevention strategies for affected individuals and families.
Clinical Features: Cutaneous Melanocytic Nevi and CNS Involvement
Neurocutaneous Melanosis Syndrome is characterized by the presence of cutaneous melanocytic nevi, which are pigmented lesions often found at birth. These nevi can vary in size and number, typically appearing large and dark. They serve as key indicators for diagnosing the condition.
“What Triggers Ulcerative Colitis Syndrome? Treatment Guide”
Central nervous system (CNS) involvement is a critical aspect of this syndrome. Patients may exhibit neurological symptoms due to abnormal neural development associated with melanocyte migration. This can lead to complications that significantly impact their quality of life.
Recognizing these clinical features early on is vital for timely intervention and management strategies. Families should be aware of both skin manifestations and potential CNS issues when navigating care options for affected individuals.
Diagnostic Criteria: Cutaneous and Neurological Manifestations
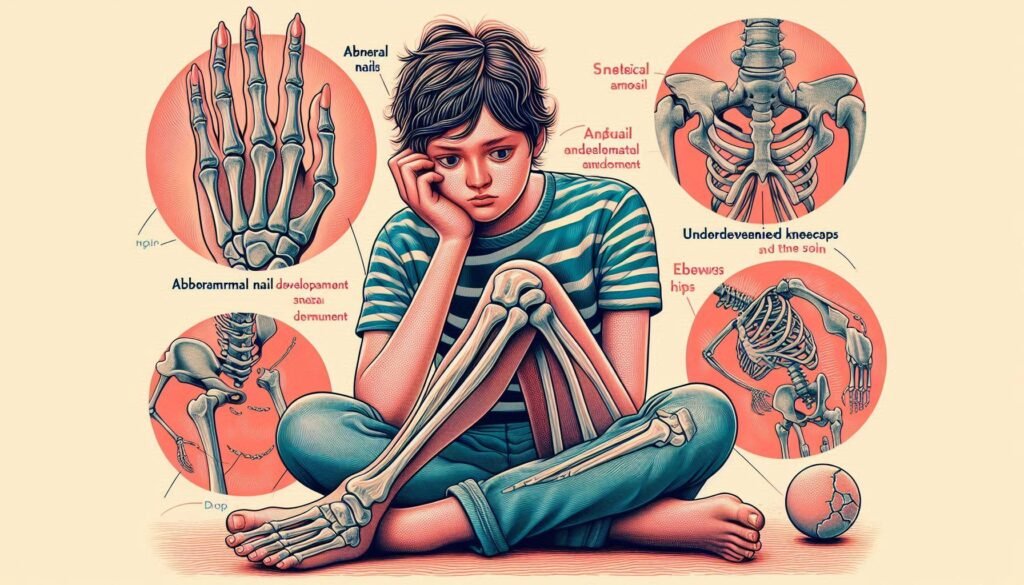
Neurocutaneous Melanosis Syndrome is characterized by distinct diagnostic criteria involving cutaneous and neurological manifestations. Patients typically present with large congenital melanocytic nevi, often covering significant body areas. These skin lesions can vary in color and size, serving as one of the first indicators of the syndrome.
“Why Does Ulnar-Mammary Syndrome Affect Development?”
Neurological involvement includes abnormalities detectable through clinical evaluation or neuroimaging. Symptoms might range from developmental delays to seizures, which can arise due to associated central nervous system (CNS) changes.
Diagnosis hinges on a thorough examination that assesses both skin lesions and neurological health. Early identification is crucial for interventions that can improve outcomes for affected individuals and their families.
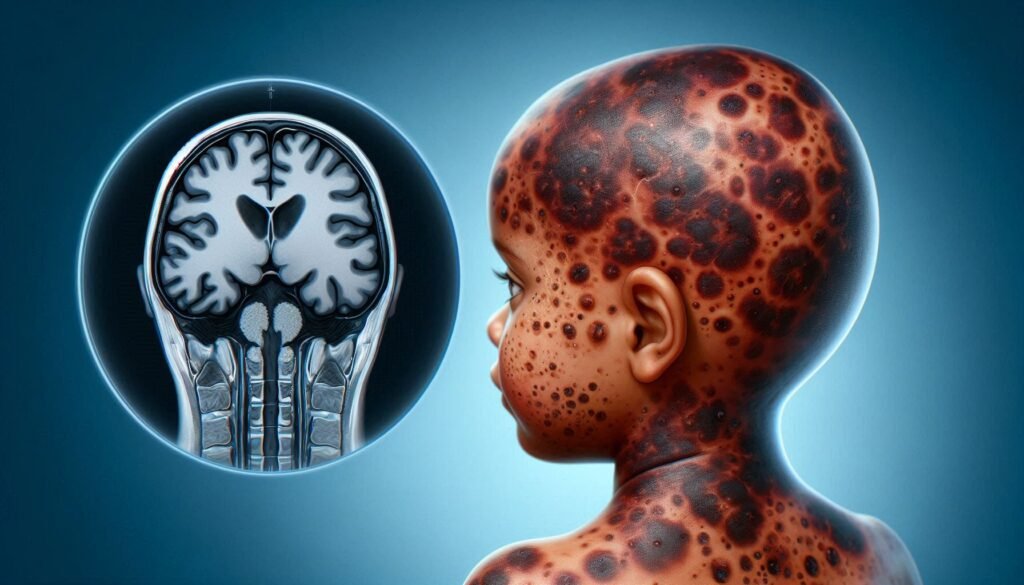
Neuroimaging Findings: MRI Characteristics of CNS Melanosis
Neuroimaging, particularly MRI, plays a crucial role in diagnosing Neurocutaneous Melanosis Syndrome. Characteristic findings often include hyperintense lesions on T1-weighted images. These lesions typically represent areas of melanotic tissue within the central nervous system.
“How Does Ulysses Syndrome Impact Migrants?”
The distribution of these lesions can vary significantly among patients. Commonly affected regions are the brain and spinal cord, leading to potential complications like hydrocephalus or seizures. Identifying the extent of CNS involvement helps guide management decisions for these individuals.
Advanced imaging techniques may reveal additional abnormalities not visible on standard scans. This provides valuable insights into disease progression and assists healthcare providers in tailoring a multidisciplinary approach for optimal care and support.
Cutaneous Manifestations: Large Congenital Melanocytic Nevi
Large congenital melanocytic nevi are a hallmark of Neurocutaneous Melanosis Syndrome. These pigmented skin lesions appear at birth or shortly after, often presenting as dark brown to black patches on the skin. Their size can vary significantly, and they may cover large areas of the body.
“What Are The Signs of VACTERL Syndrome in Newborns?”
These nevi result from abnormal development and migration of melanocytes during embryonic growth. Patients with Neurocutaneous Melanosis Syndrome typically have numerous such lesions, which can be both alarming and distressing for families.
Monitoring these nevi is crucial due to their potential complications. While most remain benign, there is an associated risk of malignant transformation over time. Regular dermatological assessments help ensure early detection and intervention if necessary.
Neurological Complications: Hydrocephalus, Seizures, and Developmental Delays
Neurocutaneous Melanosis Syndrome often includes significant neurological complications. One of the most common issues is hydrocephalus, which occurs due to an abnormal buildup of cerebrospinal fluid in the brain’s ventricles. This condition can lead to increased intracranial pressure and requires careful monitoring.
“Why Does Van der Woude Syndrome Cause Cleft Lip?”
Seizures are another serious concern for patients with this syndrome. These episodes may vary in severity, frequency, and type, requiring tailored management strategies from healthcare providers. Early intervention is crucial to minimize their impact on quality of life.
Developmental delays frequently accompany these neurological challenges. Children with Neurocutaneous Melanosis Syndrome may experience setbacks in cognitive and motor skills. Regular assessments by specialists help create personalized support plans to address individual needs effectively.
Diagnostic Approaches: Skin Examination and Neuroimaging Studies
Diagnostic approaches for Neurocutaneous Melanosis Syndrome often begin with a thorough skin examination. Dermatologists look for the presence of large congenital melanocytic nevi, which are key indicators of this condition. The size, number, and location of these nevi can provide crucial insights into the severity of potential neurological involvement.
Neuroimaging studies play a pivotal role in confirming the diagnosis. Magnetic resonance imaging (MRI) is commonly employed to evaluate central nervous system structures. This advanced imaging technique helps identify any abnormalities associated with CNS melanosis.
Radiologists focus on signs such as abnormal pigmentation or lesions within the brain and spinal cord. Early detection through these methods is vital for timely intervention and management, making accurate diagnoses essential for affected individuals and their families.
Genetic Aspects: Current Understanding and Ongoing Research
Neurocutaneous Melanosis Syndrome has garnered attention in genetic research due to its complex origins. The disorder is believed to stem from abnormalities in neural crest cells, which play a crucial role in the development of melanocytes and various nervous system structures.
Current studies are investigating specific gene mutations linked to this syndrome. Researchers have identified potential candidate genes that could contribute to the manifestation of both cutaneous and neurological symptoms.
Ongoing research aims to deepen our understanding of these genetic factors. As scientists explore molecular pathways involved in neurocutaneous melanin production, they hope to uncover targeted therapies that could improve patient outcomes and quality of life for affected individuals and families.
Management Strategies: Multidisciplinary Care Approach
Effective management of Neurocutaneous Melanosis Syndrome requires a multidisciplinary care approach. This means that various healthcare professionals collaborate to address the diverse needs of patients. Dermatologists, neurologists, neurosurgeons, and pediatricians work together to create individualized treatment plans.
Regular monitoring is essential for skin lesions as well as neurological symptoms. Coordination among specialists ensures timely interventions when complications arise. For instance, dermatological assessments can help track changes in cutaneous melanocytic nevi.
Additionally, supportive services such as physical therapy and occupational therapy may enhance developmental outcomes for affected children. This comprehensive strategy allows families to access a range of resources tailored to improve both medical care and quality of life for those living with this condition.
Neurosurgical Interventions: Indications and Techniques
Neurosurgical interventions for Neurocutaneous Melanosis Syndrome may be necessary when neurological complications arise, such as hydrocephalus or significant mass effect from CNS melanotic lesions. These procedures aim to alleviate pressure on the brain and improve the patient’s quality of life.
Techniques can include shunt placement to manage fluid accumulation or tumor resection if lesions become symptomatic. Surgeons assess each case carefully, taking into account individual risks and benefits.
Multidisciplinary collaboration is essential in planning these interventions. Neurologists, dermatologists, and neurosurgeons work closely together to ensure comprehensive care tailored to the patient’s needs. This holistic approach aims not only at treating symptoms but also at enhancing long-term outcomes for individuals with this rare syndrome.
Dermatological Care: Monitoring and Managing Skin Lesions
Dermatological care plays a crucial role in managing Neurocutaneous Melanosis Syndrome. Regular monitoring of cutaneous melanocytic nevi is essential to identify any changes that may indicate complications. Dermatologists often recommend periodic skin examinations to assess lesion size, color, and texture.
Management strategies can include laser therapy for cosmetic concerns or surgical intervention if lesions become problematic. Educating families about signs of malignant transformation is vital for early detection and treatment.
Emotional support is equally important, as visible skin lesions can impact self-esteem. Engaging with support groups helps patients and their families navigate the psychological challenges associated with this condition while fostering a sense of community and understanding.
Oncological Considerations: Risk of Malignant Transformation
Patients with Neurocutaneous Melanosis Syndrome face unique oncological considerations due to the presence of large congenital melanocytic nevi. These lesions have a documented risk of malignant transformation into melanoma, which can significantly impact patient health.
Regular monitoring is essential for early detection of any changes in these nevi. Dermatologists often recommend periodic skin examinations and imaging studies to assess lesion characteristics over time.
Understanding the potential for malignancy helps families make informed decisions about treatment options and surveillance strategies. Collaboration between dermatology, oncology, and neurology teams can enhance care and address concerns effectively throughout the patient’s life journey.
Psychosocial Impact: Living with Visible Skin Lesions and Neurological Issues
Living with Neurocutaneous Melanosis Syndrome often presents unique psychosocial challenges. Individuals may experience feelings of self-consciousness due to visible skin lesions, which can lead to anxiety or depression. This is particularly true in social situations where appearance plays a significant role.
Children and adolescents may face bullying or social exclusion because of their condition. Such experiences can hinder their emotional development and impact self-esteem. Support from family, friends, and support groups is essential for fostering resilience.
Additionally, neurological issues associated with the syndrome can complicate everyday life. Learning difficulties or developmental delays might create further barriers to social integration and personal growth. Addressing these complexities requires a compassionate approach that acknowledges both physical and emotional needs.
Quality of Life: Challenges and Supportive Care
Living with Neurocutaneous Melanosis Syndrome can present unique challenges for patients and their families. The visible skin lesions often lead to social stigma, impacting self-esteem and interactions with peers. These psychological effects can be profound, making supportive care essential.
Additionally, neurological complications such as seizures or developmental delays further complicate daily life. Families may face emotional strain while navigating educational needs and healthcare services tailored to these challenges.
Support groups play a vital role in providing emotional assistance. Connecting with others who understand the journey fosters resilience. Comprehensive care that includes mental health support is crucial for enhancing overall quality of life amidst the complexities of this syndrome.
Latest Research: Molecular Studies and Potential Therapies
Recent molecular studies on Neurocutaneous Melanosis Syndrome have focused on the genetic mutations linked to neural crest cells. Understanding these mutations can illuminate the pathogenesis of this rare condition, shedding light on why melanocytes behave abnormally in affected individuals.
Researchers are also exploring targeted therapies that could mitigate symptoms or halt disease progression. Advances in gene therapy show promise, aiming to correct underlying genetic defects associated with this syndrome.
Additionally, innovative drug developments are being investigated to manage neurological complications effectively. With continued research efforts, there is hope for new treatment avenues that improve patient outcomes and enhance quality of life for those living with Neurocutaneous Melanosis Syndrome.
Genetic Counseling: Implications for Family Planning
Genetic counseling plays a crucial role for families affected by Neurocutaneous Melanosis Syndrome. It provides valuable information about the genetic aspects of this rare disorder, helping families understand their risks and options.
Counselors assess family history and may recommend genetic testing to identify mutations associated with the syndrome. This knowledge can aid in making informed decisions regarding future pregnancies.
Additionally, counseling offers emotional support as parents navigate potential challenges related to having a child with this condition. By addressing concerns early on, families can better prepare themselves for any medical or developmental issues that may arise in their children’s lives.
Long-term Prognosis and Disease Progression
Long-term prognosis for individuals with Neurocutaneous Melanosis Syndrome varies widely. Factors influencing outcomes include the extent of cutaneous and neurological involvement. Some patients may lead relatively stable lives, while others face significant challenges due to complications.
Disease progression typically involves close monitoring of both skin and central nervous system manifestations. Regular imaging studies can help detect changes early on, allowing for timely intervention.
Medical advancements continue to enhance understanding of this rare condition, contributing to improved management strategies and outcomes. Ongoing research aims to clarify genetic factors driving disease development, offering hope for targeted therapies in the future.
Families navigating this syndrome should work closely with a multidisciplinary care team tailored to their individual needs. This collaborative approach is essential in addressing both medical concerns and psychosocial support necessary for a better quality of life.