Nephrotic syndrome is a complex kidney disorder that affects thousands of individuals worldwide. Characterized by significant proteinuria, swelling, and other critical symptoms, it can lead to serious health complications if left untreated.
Understanding nephrotic syndrome is vital for both patients and caregivers alike. This blog will delve into the intricacies of this condition—from its causes to treatment options—equipping you with essential knowledge about managing nephrotic syndrome effectively. Whether you’re facing this diagnosis or seeking information for a loved one, our comprehensive guide promises valuable insights to navigate your journey towards better kidney health.
Nephrotic Syndrome: Understanding Proteinuria and Edema
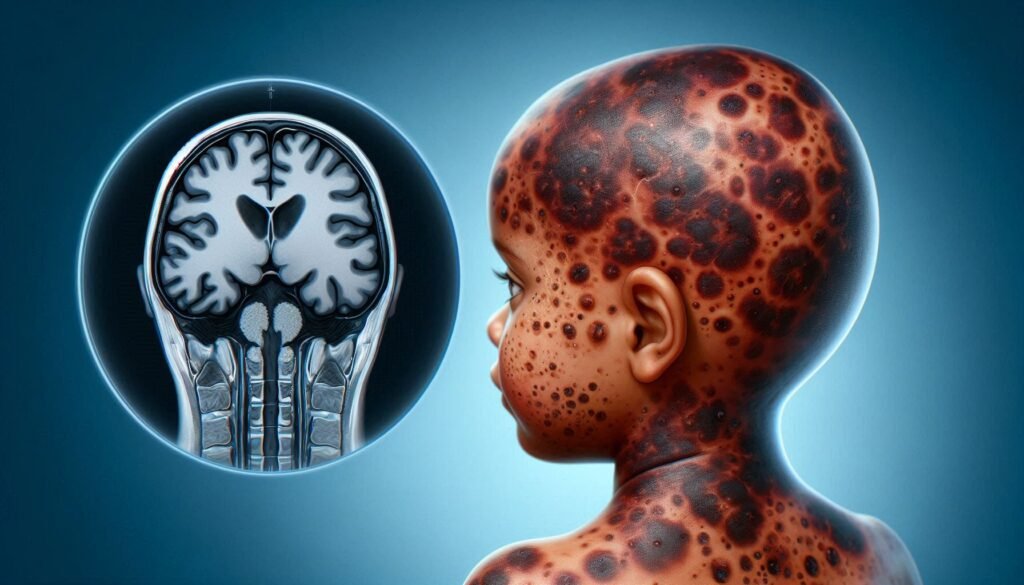
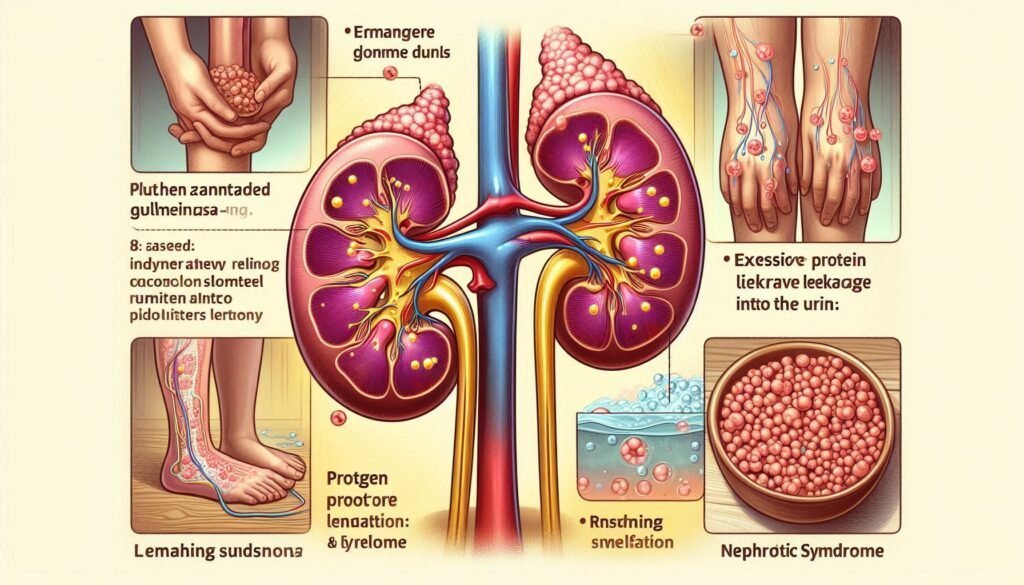
Nephrotic syndrome primarily manifests through two hallmark symptoms: proteinuria and edema. Proteinuria refers to the excessive loss of protein in urine, a result of damaged kidney filters. Healthy kidneys typically retain proteins; however, in nephrotic syndrome, these filters become compromised.
“What Causes Stockholm Syndrome? Psychology Guide”
As a consequence of significant protein loss, fluid shifts occur within the body. This leads to edema—swelling caused by fluid accumulation in tissues. Patients often notice this swelling around their eyes or ankles and may experience abdominal discomfort due to ascites.
Understanding these symptoms is crucial for early detection and effective management of nephrotic syndrome. Recognizing the signs can prompt timely medical intervention, ultimately improving outcomes for those affected by this condition.
Pathophysiology: Glomerular Barrier Dysfunction in Nephrotic Syndrome
Nephrotic syndrome primarily involves dysfunction of the glomerular filtration barrier. This multi-layered structure consists of endothelial cells, a basement membrane, and podocytes. When this barrier is compromised, it allows excessive protein to leak into the urine—a condition known as proteinuria.
“Why Does Scheie Syndrome Affect Metabolism?”
Podocyte injury plays a critical role in this dysfunction. These specialized cells maintain the integrity of the filtration barrier. Damage can occur due to various factors such as inflammation or genetic mutations.
As proteins escape into the urine, serum albumin levels drop, leading to hypoalbuminemia. This decrease in plasma oncotic pressure results in fluid shifting from blood vessels into surrounding tissues, causing edema—another hallmark symptom of nephrotic syndrome.
Types of Nephrotic Syndrome: Minimal Change Disease, FSGS, and Others
Nephrotic syndrome is categorized into various types, each presenting distinct features. Minimal Change Disease (MCD) is the most common form in children. It often responds well to steroid therapy and tends to have a good prognosis.
Focal Segmental Glomerulosclerosis (FSGS), on the other hand, affects adults more frequently. This condition involves scarring of some kidney glomeruli and may be resistant to standard treatments.
“How Does Seckel Syndrome Impact Growth?”
Other forms include Membranous Nephropathy and Secondary Nephrotic Syndrome caused by conditions like diabetes or lupus. Each type has unique underlying mechanisms and treatment protocols that require careful diagnosis for effective management.
Clinical Presentation: Key Symptoms and Signs of Nephrotic Syndrome
Nephrotic syndrome often presents with distinct symptoms that can significantly impact daily life. One of the hallmark signs is proteinuria, leading to a frothy appearance in urine due to excessive protein loss. This condition may also manifest as noticeable swelling or edema, primarily in the legs, ankles, and around the eyes.
“What Are The Signs of Sandhoff Syndrome in Infants?”
Patients frequently experience fatigue and weight gain due to fluid retention. These changes can be alarming and may prompt individuals to seek medical attention.
Additionally, nephrotic syndrome might cause high blood pressure and elevated cholesterol levels. Recognizing these symptoms early is crucial for effective management and treatment options moving forward.
Diagnosis: Laboratory Tests, Imaging Studies, and Kidney Biopsy
Diagnosis of nephrotic syndrome begins with a thorough evaluation of symptoms and medical history. Laboratory tests play a crucial role, especially urine tests that measure protein levels. High levels of proteinuria are indicative of the condition.
“Why Does Schwartz-Jampel Syndrome Cause Muscle Stiffness?”
Blood tests help assess kidney function through measurements like serum creatinine and albumin. Imaging studies such as ultrasound may be used to examine kidney structure for abnormalities or blockages.
A kidney biopsy is often necessary for definitive diagnosis, particularly when determining the underlying cause. This procedure involves taking a small tissue sample from the kidney to analyze its condition under a microscope. The results can guide treatment decisions effectively while providing valuable insights into disease progression.
Causes of Nephrotic Syndrome: Primary and Secondary Etiologies
Nephrotic syndrome can stem from various causes, classified into primary and secondary etiologies. Primary nephrotic syndrome originates within the kidneys and includes conditions like Minimal Change Disease (MCD) and Focal Segmental Glomerulosclerosis (FSGS). These disorders directly affect the glomeruli, leading to significant proteinuria.
On the other hand, secondary nephrotic syndrome results from systemic diseases or external factors. Conditions such as diabetes mellitus, lupus erythematosus, infections, and certain medications can trigger kidney damage.
“How Does Shapiro Syndrome Affect Body Temperature?”
Other contributors may involve genetic mutations that impact kidney function. Understanding these causes is crucial for targeted treatments and effective management strategies in patients with nephrotic syndrome.
Pediatric vs Adult Nephrotic Syndrome: Age-Related Differences
Nephrotic syndrome presents differently in children compared to adults. In pediatric cases, minimal change disease is the most common form. This type often responds well to steroid therapy and frequently remits after treatment. Children may also experience more pronounced edema due to their smaller body size.
Adults typically encounter focal segmental glomerulosclerosis (FSGS) or membranous nephropathy, which can be more challenging to manage. These forms are often resistant to steroids and may require additional immunosuppressive therapies.
“What Causes Sudden Infant Death Syndrome? Prevention Guide”
Moreover, the underlying causes vary significantly by age group. While many pediatric cases are idiopathic, adult nephrotic syndrome might stem from systemic diseases like diabetes or hypertension, complicating treatment options and prognosis for older patients.
Treatment Approaches: Steroids and Immunosuppressive Therapies
Treatment of nephrotic syndrome often begins with corticosteroids. These medications help reduce inflammation and proteinuria by targeting the immune system. For many patients, steroids can lead to significant improvement in symptoms.
However, some individuals do not respond adequately to steroid therapy. In these cases, immunosuppressive agents may be necessary. Drugs like cyclophosphamide or mycophenolate mofetil are commonly used to manage more severe forms of nephrotic syndrome.
Monitoring for side effects is crucial when using these treatments. Patients might experience increased susceptibility to infections or other complications from long-term use of immunosuppressants. Regular follow-ups with healthcare providers ensure appropriate adjustments and management strategies are in place.
Management of Edema: Diuretics and Fluid Balance
Edema, a common symptom of nephrotic syndrome, occurs due to fluid retention. Effective management is crucial for improving the patient’s quality of life. Diuretics are often prescribed to help reduce excess fluid buildup in the body.
These medications work by increasing urine production, which can alleviate swelling and discomfort. However, monitoring kidney function is essential when using diuretics since they may affect electrolyte balance and hydration status.
In addition to medication, maintaining proper fluid intake is vital. Patients should collaborate with healthcare providers to determine the right amount of fluids needed based on their individual condition. A balanced approach ensures that edema is managed effectively while avoiding potential complications associated with dehydration or over-hydration.
Complications: Thromboembolism, Infections, and Acute Kidney Injury
Nephrotic syndrome increases the risk of thromboembolism due to elevated levels of protein in urine. This condition leads to changes in blood coagulability, making patients more susceptible to clot formation. Deep vein thrombosis and pulmonary embolism are serious complications that require immediate attention.
Infections also pose a significant threat for individuals with nephrotic syndrome. The loss of immunoglobulins through proteinuria weakens the immune system, heightening vulnerability to infections like pneumonia and cellulitis. Prompt recognition and treatment are critical to prevent severe outcomes.
Acute kidney injury can occur as a result of the underlying disease process or its complications. Decreased renal perfusion from dehydration or thrombosis may lead to rapid deterioration in kidney function, necessitating close monitoring by healthcare providers.
Dietary Considerations: Sodium, Protein, and Fluid Restrictions
Dietary considerations play a crucial role in managing nephrotic syndrome. Sodium intake should be limited to reduce edema and high blood pressure. A low-sodium diet helps control fluid retention, making daily meals more manageable.
Protein consumption requires careful attention as well. While protein is essential for health, excessive intake can burden the kidneys further. Balancing protein levels based on individual needs is vital for maintaining kidney function without exacerbating symptoms.
Fluid restrictions may also be necessary depending on the severity of edema and overall kidney function. Monitoring fluid intake helps prevent overload while ensuring hydration remains adequate. Collaborating with healthcare professionals or nutritionists can provide tailored dietary plans that support better outcomes in nephrotic syndrome management.
Monitoring Disease Activity: Proteinuria and Albumin Levels
Monitoring disease activity in nephrotic syndrome primarily involves tracking proteinuria and albumin levels. Proteinuria, or the presence of excess protein in urine, is a key indicator of kidney function. Regular urine tests help assess how well kidneys are filtering proteins.
The measurement of serum albumin is equally important. Low levels often signify significant protein loss through the kidneys, prompting further evaluation and adjustment to treatment plans. Elevated protein loss can lead to complications like edema and increased risk for infections.
Both parameters guide healthcare providers in tailoring therapies effectively. Consistent monitoring helps identify relapses early on, ensuring timely interventions to maintain kidney health and overall wellbeing for patients with nephrotic syndrome.
Steroid-Resistant Nephrotic Syndrome: Challenges and Management
Steroid-resistant nephrotic syndrome presents significant challenges for both patients and healthcare providers. Unlike typical cases that respond well to corticosteroids, these patients often experience persistent proteinuria and edema despite treatment. This resistance complicates management strategies.
Identifying the underlying causes is crucial in tailoring treatment options. Genetic factors or secondary conditions may contribute to steroid resistance, necessitating further investigation through kidney biopsies or genetic testing.
Management of steroid-resistant nephrotic syndrome typically involves immunosuppressive therapies such as calcineurin inhibitors and mycophenolate mofetil. Close monitoring of kidney function and potential side effects from medications is essential for optimizing patient care while minimizing risks associated with long-term treatment.
Long-term Prognosis: Remission, Relapse, and Kidney Function
The long-term prognosis for nephrotic syndrome varies significantly among individuals. Some patients achieve complete remission with appropriate treatment, often leading to a near-normal quality of life. Regular monitoring is essential to track kidney function and protein levels.
However, relapses can occur, particularly in those with minimal change disease or focal segmental glomerulosclerosis (FSGS). Identifying triggers for these relapses can help manage the condition more effectively.
Kidney function must be closely monitored over time as chronic nephrotic syndrome can lead to progressive renal impairment in some cases. Early intervention and adherence to treatment plans are crucial for preserving kidney health and preventing complications associated with declining function.
Genetic Forms of Nephrotic Syndrome: Inheritance and Testing
Nephrotic syndrome can have genetic origins, with several inherited forms linked to mutations in specific genes. These genetic variants affect the function of glomerular filtration and may lead to proteinuria and edema from an early age.
Inheritance patterns vary, with some forms following an autosomal dominant or recessive pattern while others are X-linked. Understanding these inheritance mechanisms is crucial for family planning and risk assessment.
Genetic testing plays a vital role in diagnosing hereditary nephrotic syndrome. It helps identify mutations responsible for the condition, guiding treatment options and providing insights into prognosis. Genetic counseling can support families navigating this complex landscape, offering information on potential outcomes and implications for future generations.
Psychosocial Impact: Coping with a Chronic Kidney Condition
Living with nephrotic syndrome can profoundly affect emotional and mental well-being. Patients often experience anxiety, depression, or feelings of isolation due to their chronic condition. The uncertainty around disease progression can amplify these emotions.
Support from family and friends plays a crucial role in coping. Open discussions about feelings and challenges can foster understanding and create a supportive environment. Connecting with others facing similar struggles through support groups may also provide comfort.
Professional help, such as counseling or therapy, is beneficial for many individuals dealing with the psychosocial aspects of nephrotic syndrome. Mental health professionals can offer strategies to manage stress while promoting resilience in the face of ongoing health issues.
Transition of Care: Pediatric to Adult Nephrotic Syndrome Management
Transitioning from pediatric to adult care in nephrotic syndrome requires careful planning. Pediatric patients often have a different set of needs and caregivers than adults. As they grow, their management strategies must evolve to reflect this change.
During this transition, communication between the child’s pediatric nephrologist and an adult specialist is crucial. This ensures continuity of care while addressing any new health concerns that may arise as the patient matures.
Education plays a key role during this phase. Young adults should be empowered with knowledge about their condition, treatment options, and self-management techniques. By fostering independence and understanding, healthcare providers can help these individuals navigate their ongoing journey with nephrotic syndrome effectively.
Latest Research: Novel Therapies and Clinical Trials
Research into nephrotic syndrome continues to evolve, offering hope for improved treatments. Recent studies are exploring novel therapies that target specific pathways involved in kidney function and proteinuria reduction.
Biologics and targeted immunotherapy have shown promise in clinical trials, providing alternatives to traditional steroids. These advancements may lead to better management of steroid-resistant patients who struggle with standard treatments.
Additionally, genetic research is paving the way for personalized medicine approaches tailored to individual patient’s needs. As science progresses, new treatment strategies aim not only at remission but also at preventing relapses and preserving kidney function long-term.
Staying informed about ongoing clinical trials can empower patients and caregivers as they navigate this complex condition. Engaging with healthcare providers about emerging options can help ensure optimal care moving forward.