Nasal glioma syndrome might sound like an unfamiliar term, but it describes a fascinating and complex medical condition. This congenital anomaly involves the presence of abnormal neural tissue in or around the nasal cavity. For many, this can lead to various health concerns that warrant attention and understanding.
Many individuals may be surprised to learn that nasal gliomas are not true brain tumors; instead, they represent a unique blend of embryonic tissues that do not belong where they are found. Navigating through the intricacies of diagnosis and treatment requires careful consideration from both patients and healthcare providers.
If you or someone you know is affected by this condition, it’s essential to understand its origins, manifestations, and potential impacts on quality of life. Let’s delve deeper into what nasal glioma syndrome entails so you can arm yourself with knowledge about this intriguing yet challenging issue.
Nasal Glioma: Congenital Masses of Heterotopic Neural Tissue
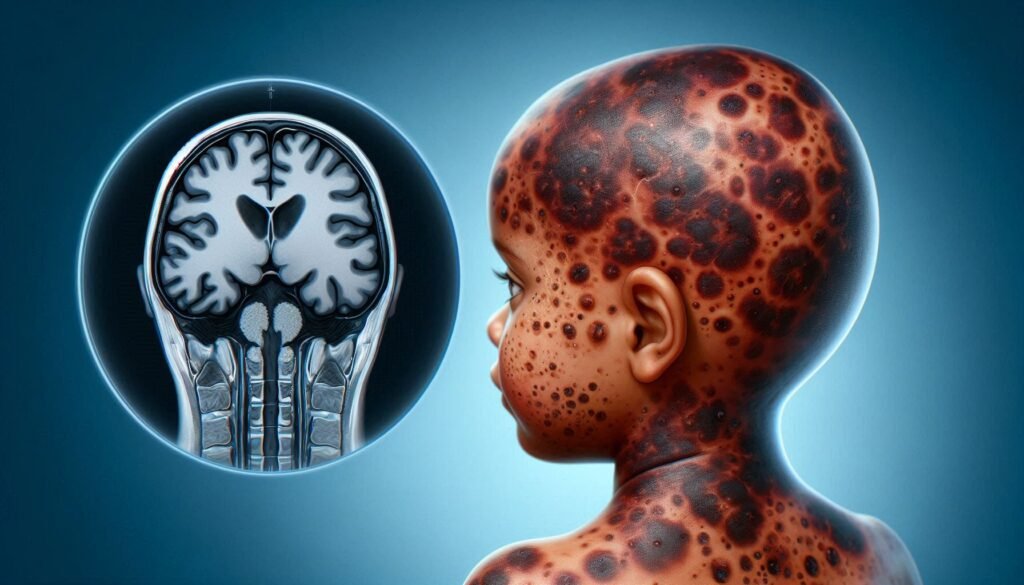
Nasal glioma is a rare congenital condition characterized by the presence of heterotopic neural tissue in or around the nasal region. Unlike typical brain tumors, these masses are not derived from brain cells but instead originate from aberrant embryonic development.
Typically, they form during gestation when there’s an error in the migration of neuroectodermal tissue. This results in small nodules that can appear either intranasally or extranasally. Their exact location often influences symptoms and complications.
“How Does Tarsal Tunnel Syndrome Affect Foot Function?”
These lesions may be asymptomatic at birth but can lead to nasal obstruction, infections, or aesthetic concerns as the individual grows. Understanding their nature is crucial for diagnosis and effective management strategies tailored to each patient’s needs.
Embryology: Origin and Development of Nasal Gliomas
Nasal gliomas are intriguing congenital masses that arise from ectopic neural tissue during embryonic development. These tumors typically originate from the neuroectoderm, which is responsible for forming the brain and spinal cord. During early fetal growth, disruptions in this process can lead to abnormal placements of neural cells.
As the fetus develops, these misplaced tissues may form along the nasal structures or even outside them. The precise cause of this aberration is not fully understood but could involve genetic factors or environmental influences impacting normal cell migration.
“What Are The Signs of Temple-Baraitser Syndrome?”
The result is a spectrum of nasal glioma presentations ranging from extranasal to intranasal types. Understanding the embryological origin helps in diagnosing and managing this condition effectively while highlighting its complexity within pediatric health care.
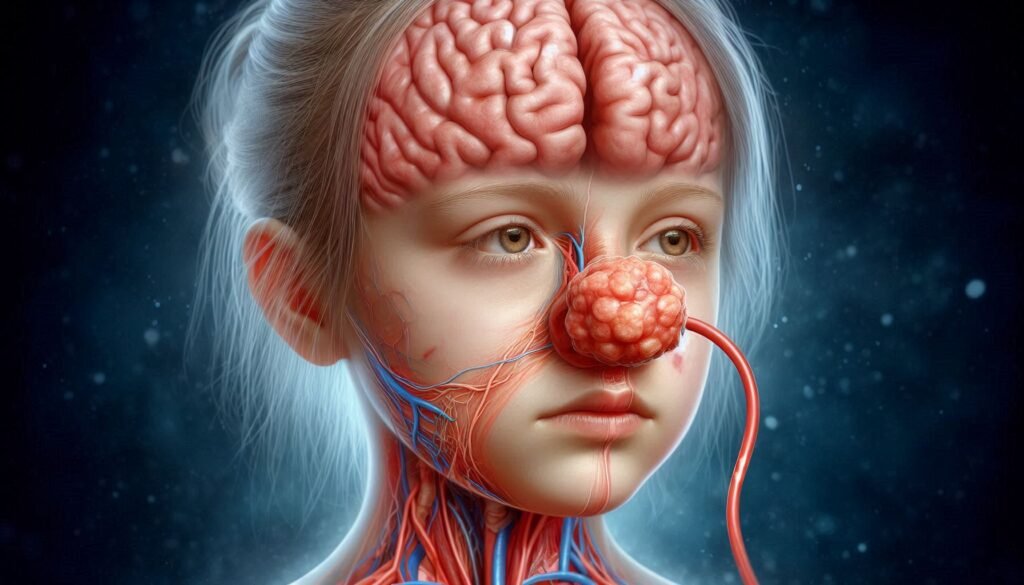
Clinical Presentation: Extranasal, Intranasal, and Combined Types
Nasal gliomas can present in various forms, primarily classified as extranasal and intranasal types. Extranasal nasal gliomas typically appear as firm masses located outside the nasal cavity. These growths may be palpable on examination and often protrude through the skin of the forehead or bridge of the nose.
“Why Does Thrombocytopenia-Absent Radius Syndrome Occur?”
Intranasal nasal gliomas are found within the nasal passages. Patients with this type may experience symptoms like nasal obstruction or frequent sinus infections due to blockage. These lesions can sometimes be mistaken for other conditions affecting the sinuses.
Combined types showcase characteristics from both external and internal presentations. This dual occurrence can complicate diagnosis, leading to a range of symptoms that vary between patients depending on the extent of involvement in both areas.
Differential Diagnosis: Distinguishing from Other Nasal Masses
When assessing nasal glioma syndrome, it’s crucial to differentiate these masses from other conditions. Various types of lesions can arise in the nasal cavity, including juvenile nasopharyngeal angiofibroma and inverted papilloma. These tumors often present with similar symptoms but have distinct characteristics.
“How Does Toxic Shock Syndrome Develop? Prevention Guide”
Other important considerations include rhabdomyosarcoma and neuroblastoma, particularly in pediatric patients. Their aggressive nature necessitates a careful evaluation to avoid misdiagnosis, which could delay appropriate treatment.
Infections such as fungal or bacterial sinusitis may mimic the presentation of nasal gliomas. A thorough clinical history and physical examination are essential for accurate diagnosis and effective management strategies tailored to each unique case.
Imaging Studies: CT, MRI, and Their Role in Diagnosis
Imaging studies play a crucial role in diagnosing Nasal Glioma Syndrome. Both CT and MRI are valuable tools that help visualize the extent of these congenital masses.
CT scans provide detailed cross-sectional images, highlighting bony structures and any associated calcifications. They can quickly reveal the presence of nasal gliomas and help assess their relationship with surrounding anatomical features.
“What Causes Uhl Anomaly Syndrome? Heart Guide”
MRI offers superior soft tissue contrast, making it ideal for evaluating the mass’s exact nature and connection to adjacent neural tissues. This imaging modality is particularly effective in identifying intracranial involvement, guiding treatment decisions effectively while minimizing potential complications during surgery.
Histopathological Features: Microscopic Characteristics of Nasal Gliomas
Nasal gliomas exhibit distinct histopathological features that assist in their diagnosis. Microscopically, they present as well-circumscribed lesions composed predominantly of glial tissue. The presence of astrocytes is typical, often arranged in a fibrillary pattern.
“Why Does Ullrich Congenital Muscular Dystrophy Affect Muscles?”
Additionally, scattered neurons and neuroglial components may be observed within the mass. This combination can lead to varying degrees of cellularity and organization depending on the specific case.
An important aspect is the absence of typical brain architecture; nasal gliomas do not form true brain tissue structures. Instead, they demonstrate a blend of neural elements embedded within fibrous stroma, which contributes to their unique characteristics under microscopic examination.
Genetic Associations: Current Understanding and Research
Research into the genetic associations of Nasal Glioma Syndrome has been limited but is gradually expanding. Current studies have identified potential links between certain genetic mutations and the development of these congenital masses. These findings suggest that aberrations in neural crest cell migration may play a significant role.
Genetic testing is becoming more relevant as we strive to understand this condition better. While specific genes associated with nasal gliomas are not yet fully characterized, emerging data point to possible hereditary patterns in some families.
Ongoing research aims to uncover the intricate molecular mechanisms behind nasal gliomas. Future discoveries could lead to targeted therapies and improved diagnostic tools, enhancing our understanding of how genetics influence this syndrome’s presentation and management.
Surgical Management: Approaches and Techniques
Surgical management of nasal glioma syndrome primarily involves the excision of the mass. The approach depends on the location and extent of the lesion. Extranasal masses may require a more extensive procedure, while intranasal lesions can often be accessed through less invasive techniques.
Techniques vary from traditional open surgery to newer endoscopic methods. Endoscopy allows surgeons to operate with minimal disruption, reducing recovery time and complications. This method is particularly beneficial for pediatric patients or those presenting with significant anatomical challenges.
Surgeons must carefully consider potential connections to intracranial structures during surgery. Knowledge of these relationships helps in planning an effective resection strategy that minimizes risks while ensuring complete removal of the abnormal tissue.
Endoscopic Surgery: Minimally Invasive Options for Nasal Gliomas
Endoscopic surgery presents a minimally invasive option for treating nasal gliomas, offering several advantages over traditional surgical methods. This technique utilizes small incisions and specialized instruments guided by a camera, allowing surgeons to navigate the intricate nasal anatomy with precision.
During the procedure, surgeons can access both intranasal and extranasal components of the tumor without compromising surrounding tissues. This approach reduces recovery time and minimizes postoperative discomfort for patients.
Moreover, endoscopic surgery often leads to fewer complications compared to open surgeries. With its ability to provide clear visualization of the surgical site, it enhances safety while effectively removing the mass. As technology advances, endoscopic techniques continue to improve outcomes for individuals diagnosed with nasal glioma syndrome.
Complications: Cerebrospinal Fluid Leak and Intracranial Connection
Nasal Glioma Syndrome can lead to significant complications, particularly concerning cerebrospinal fluid (CSF) leaks. These leaks occur when the protective barriers surrounding the brain and spinal cord are breached, often during surgical intervention or as a result of the mass’s intrinsic nature.
An intracranial connection may be present in some cases, allowing for direct communication between nasal gliomas and the cranial cavity. This connection poses risks such as meningitis or other serious infections due to pathogens gaining access to sensitive areas.
Monitoring for signs of CSF leakage is crucial post-surgery. Symptoms like clear drainage from the nose or changes in hearing should prompt immediate medical attention. Addressing these complications early prevents further neurological issues and ensures better patient outcomes.
Recurrence Risk: Follow-up and Monitoring Strategies
Recurrence risk for nasal glioma syndrome varies based on the surgical approach and completeness of tumor removal. After surgery, ongoing monitoring is essential to detect any signs of regrowth early. Regular follow-ups with imaging studies like MRI can help assess the surgical site.
Patients should be educated about symptoms that might indicate recurrence, such as nasal obstruction or changes in facial appearance. Empowering individuals with knowledge aids prompt reporting and timely intervention.
Multidisciplinary care enhances surveillance strategies by involving specialists from various fields, including ENT surgeons and radiologists. This coordinated effort ensures comprehensive management and supports optimal patient outcomes throughout their recovery journey.
Aesthetic Considerations: Reconstructive Techniques After Removal
Aesthetic outcomes are a crucial consideration following the surgical removal of nasal gliomas. The location and size of these lesions often necessitate careful planning to minimize visible scarring. Surgeons typically employ techniques that aim to preserve surrounding tissue, ensuring a more natural appearance post-surgery.
Reconstructive methods can include skin grafts or local flaps, which help restore the contour and function of the nose. Utilizing advanced suturing techniques further enhances aesthetic results while facilitating healing.
For pediatric patients, special attention is given to growth patterns and developmental changes. This approach ensures that any reconstruction accommodates future growth, maintaining both form and function as children develop into adulthood.
Pediatric Considerations: Management in Infants and Children
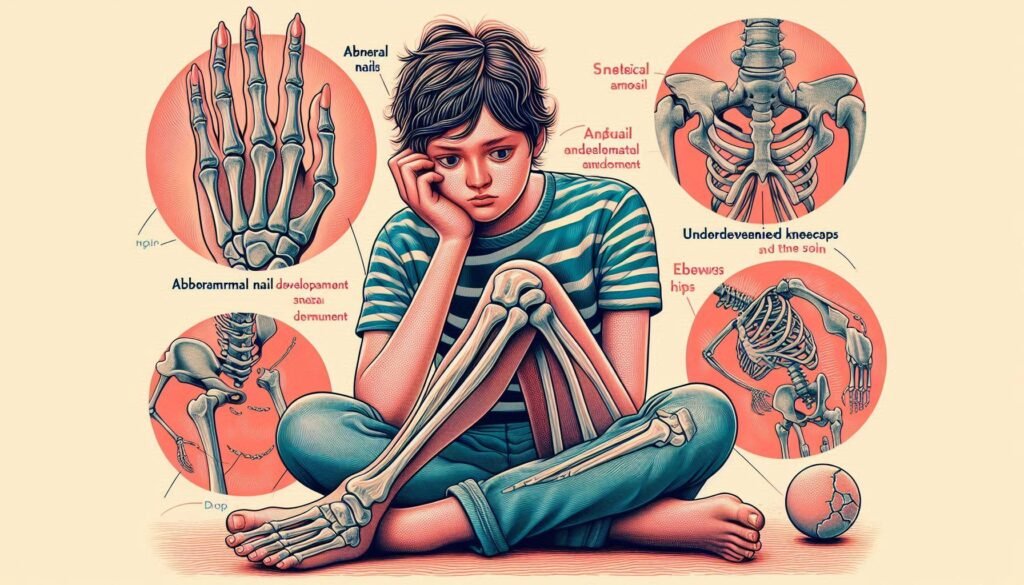
Nasal glioma syndrome poses unique challenges in pediatric patients. Infants and children are at a higher risk for complications due to their developing anatomy. Early diagnosis is essential to prevent airway obstruction and other associated issues.
Management often involves a multidisciplinary team, including pediatricians, ENT specialists, and neurosurgeons. Treatment plans should be tailored to the child’s age, size, and overall health status. Surgical intervention is usually recommended if the mass causes significant symptoms or risks associated complications.
Post-operative care is critical in this population. Monitoring for potential recurrence or new symptoms helps ensure that any issues are addressed promptly. Parents must also receive guidance on supporting their child’s emotional well-being throughout treatment and recovery.
Impact on Nasal Function: Breathing and Olfactory Issues
Nasal glioma syndrome can significantly impact nasal function, particularly breathing and the sense of smell. The presence of congenital masses obstructs airflow in the nasal passages, leading to difficulties in respiration. Patients may experience chronic nasal congestion or difficulty inhaling deeply.
Olfactory issues are also common among affected individuals. Nasal gliomas often disrupt the normal functioning of olfactory receptors, which play a crucial role in detecting scents. This disruption can result in partial or complete loss of smell, impacting daily life and enjoyment.
Moreover, these complications might lead to secondary problems such as sleep apnea due to impaired airflow during sleep. Addressing these functional issues is essential for improving quality of life for those impacted by nasal glioma syndrome.
Psychological Support: Addressing Concerns in Affected Individuals
Living with Nasal Glioma Syndrome can be challenging for both patients and their families. The uncertainty surrounding the condition often leads to anxiety, fear, and emotional distress. Addressing these psychological concerns is crucial for overall well-being.
Support from mental health professionals plays a vital role in helping affected individuals cope with their feelings. Therapy sessions can provide a safe space to discuss fears related to diagnosis, treatment options, and potential outcomes.
Peer support groups also offer valuable connections among those facing similar challenges. Sharing experiences fosters a sense of community and normalizes the emotional journey associated with this syndrome. Encouraging open discussions about mental health promotes resilience and aids in coping strategies throughout the treatment process.
Latest Research: Molecular Studies and New Diagnostic Tools
Recent studies on nasal glioma syndrome have focused heavily on the molecular underpinnings of this unique condition. Researchers are investigating genetic mutations associated with the development of these congenital masses. Understanding these factors can pave the way for early detection and targeted therapies.
New diagnostic tools have emerged, enhancing our ability to identify nasal gliomas more accurately. Techniques such as advanced imaging modalities combined with molecular diagnostics provide a clearer picture of tumor characteristics. This progress allows for better differentiation from other nasal lesions.
The integration of liquid biopsies is also gaining attention in research circles. These non-invasive tests could help detect genetic markers associated with nasal glioma syndrome, providing valuable information without extensive surgical procedures.
Multidisciplinary Approach: Coordinating Care Among Specialists
A multidisciplinary approach is crucial for effectively managing Nasal Glioma Syndrome. Coordinating care among various specialists ensures comprehensive treatment and improved patient outcomes. This often involves collaboration between pediatricians, otolaryngologists, neurosurgeons, radiologists, and genetic counselors.
Each specialist plays a vital role in addressing the complexities of this condition. For instance, an otolaryngologist may evaluate nasal function while a neurosurgeon addresses any intracranial connections. Radiologists provide essential imaging insights that guide surgical planning and monitoring.
Regular follow-ups and open communication among healthcare providers are key to adapting treatment plans as needed. This collaborative framework not only enhances medical care but also supports families during their journey with Nasal Glioma Syndrome. By bringing together diverse expertise, patients receive more holistic care tailored to their unique needs.