ICF Syndrome, short for Immunodeficiency, Centromeric instability, and Facial anomalies, is a rare genetic disorder that presents unique challenges for those affected. Understanding this syndrome is crucial not only for patients but also for families and healthcare providers. In this comprehensive guide, we will explore the underlying genetic basis of ICF Syndrome, its clinical features, and the various treatment strategies available.
Whether you’re seeking information out of personal interest or need support navigating this complex condition, our aim is to provide clear insights into all aspects of ICF Syndrome. Join us as we delve deeper into what makes this syndrome significant in today’s medical landscape.
ICF Syndrome: Understanding Immunodeficiency, Centromeric instability, and Facial anomalies
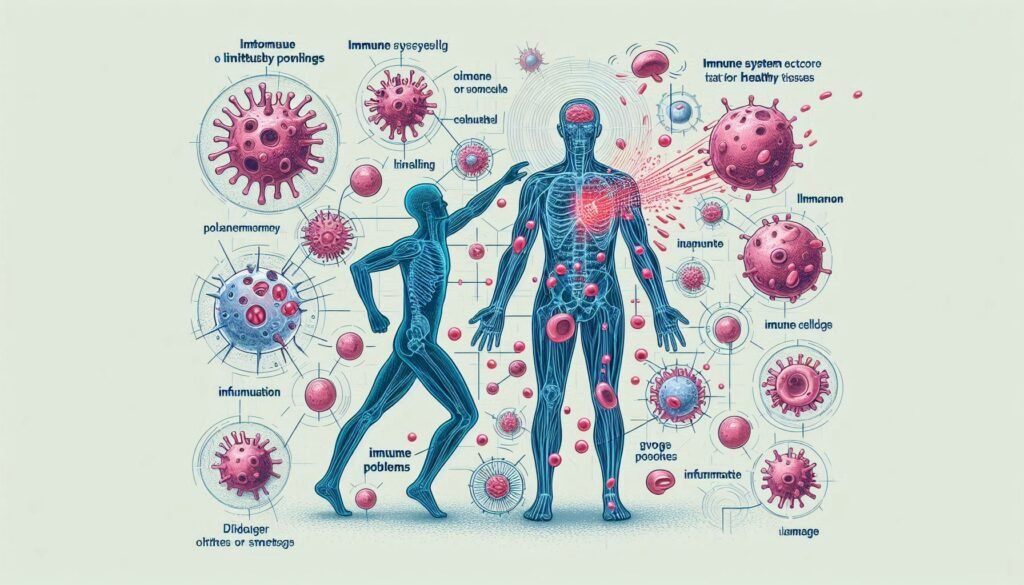
ICF Syndrome is a rare genetic disorder characterized by three main features: immunodeficiency, centromeric instability, and distinct facial anomalies. Individuals with ICF often experience immune system dysfunction, making them susceptible to infections. This aspect of the syndrome significantly impacts their overall health and quality of life.
“How Does Barlow’s Syndrome Impact Heart Valve Function?”
Centromeric instability refers to abnormalities in chromosome structure, leading to genomic instability that can affect cellular function. These chromosomal changes contribute to various developmental issues.
Facial anomalies associated with ICF Syndrome include unique physical traits such as a broad forehead and prominent ears. Understanding these characteristics helps healthcare professionals provide better diagnostic and therapeutic support for affected individuals and their families.
Genetic Basis: DNMT3B and Other Gene Mutations
ICF Syndrome is primarily linked to mutations in the DNMT3B gene. This gene plays a crucial role in DNA methylation, a process vital for regulating gene expression. When DNMT3B is mutated, it leads to abnormal methylation patterns.
In addition to DNMT3B, other genetic mutations have been associated with ICF Syndrome. These include changes in genes involved in chromosomal stability and immune function. Each mutation contributes uniquely to the syndrome’s clinical features.
“What Causes Beckwith-Wiedemann Syndrome in Infants?”
Understanding these genetic factors can help researchers develop targeted therapies and improve diagnostic methods for patients affected by ICF Syndrome. Identifying specific mutations offers insights into disease mechanisms and potential treatment strategies.
Pathophysiology of ICF Syndrome: DNA Methylation Defects
ICF Syndrome is characterized by defects in DNA methylation, which plays a crucial role in gene regulation. In individuals with this syndrome, abnormal methylation patterns lead to the silencing of specific genes necessary for immune function and chromosomal stability.
“Why Does Benedikt Syndrome Affect Eye Movement? Complete Guide”
The most prominent genetic alteration associated with ICF Syndrome involves mutations in the DNMT3B gene. This gene encodes an enzyme responsible for adding methyl groups to DNA, ensuring proper expression of vital genes. Without adequate functioning of DNMT3B, cells cannot maintain normal epigenetic landscapes.
Consequently, these alterations result in genomic instability and contribute to clinical manifestations such as immunodeficiency and distinct facial anomalies observed in affected patients. Understanding this pathophysiology sheds light on potential therapeutic avenues.
Clinical Features and Characteristic Facial Anomalies
ICF Syndrome presents a range of clinical features that vary among individuals. Common manifestations include immunodeficiency, leading to recurrent infections and other health challenges. Affected patients often display distinct facial anomalies.
“What Is Birt-Hogg-Dubé Syndrome? Cancer Risk & Management”
Characteristic facial features may include a broad forehead, hypertelorism (widely spaced eyes), and low-set ears. These traits can contribute to the identification of ICF Syndrome in affected individuals at an early age.
Additionally, patients might exhibit malformations like cleft lip or palate, contributing further to their unique presentation. Recognition of these signs is crucial for timely diagnosis and intervention strategies aimed at managing the syndrome effectively.
Immunological Manifestations in ICF Syndrome
ICF Syndrome is characterized by significant immunological challenges. Patients often experience a range of immune deficiencies, primarily affecting both humoral and cellular immunity. This can lead to recurrent infections that may vary in severity.
“How Does Blue Baby Syndrome Affect Oxygen Levels?”
One notable aspect of ICF Syndrome is the reduced production of immunoglobulins. This deficiency compromises the body’s ability to fight off common pathogens, making patients more susceptible to infections.
Additionally, T-cell counts may be diminished or dysfunctional in affected individuals. These immune anomalies contribute to increased vulnerability and require careful monitoring and management strategies tailored for each patient’s needs. Early intervention can help mitigate some risks associated with these manifestations.
Recurrent Infections: Patterns and Management
Recurrent infections are a significant concern in individuals with ICF Syndrome. These patients often experience frequent respiratory, gastrointestinal, and skin infections due to their compromised immune systems. The underlying immunodeficiency leads to an increased susceptibility to pathogens.
Management of recurrent infections involves prompt treatment with appropriate antibiotics or antiviral medications. Patients may require a tailored vaccination schedule to enhance protection against common infectious agents.
“What Causes Brugada Syndrome & Why Is It Dangerous?”
Regular monitoring by healthcare providers is essential for timely intervention when symptoms arise. Supportive care measures, such as proper nutrition and hygiene practices, can also help minimize the risk of infection and improve overall health outcomes for those affected by ICF Syndrome.
Chromosomal Instability: Cytogenetic Findings
Chromosomal instability is a hallmark of ICF Syndrome, primarily affecting the stability of centromeric regions. This condition leads to various cytogenetic findings that are crucial for diagnosis and understanding disease progression.
Patients often exhibit specific chromosomal abnormalities, including increased rates of chromosome breaks and rearrangements. These anomalies can be visualized through karyotyping and fluorescence in situ hybridization (FISH) techniques.
“Why Does Burning Mouth Syndrome Occur? Treatment Guide”
The presence of these cytogenetic alterations not only aids in confirming the diagnosis but also provides insights into potential treatment strategies. Understanding these instabilities can help clinicians monitor patients more effectively over time.
Growth and Developmental Delays in ICF Syndrome
Individuals with ICF Syndrome often experience growth and developmental delays. These challenges can manifest early in childhood, affecting motor skills and cognitive development.
Children may have difficulty reaching milestones such as sitting, walking, or speaking. Delays are not uniform; some might struggle more than others depending on the severity of their condition.
Additionally, social interactions can be impacted due to these developmental hurdles. Early intervention programs focusing on physical therapy, speech therapy, and educational support are crucial for improving outcomes and enhancing quality of life for affected individuals.
Neurological Manifestations and Cognitive Impact
Neurological manifestations in ICF Syndrome can vary significantly among affected individuals. Common issues include developmental delays, speech difficulties, and motor skill challenges. These symptoms often stem from the underlying genetic mutations impacting neurological development.
Cognitive impacts are also notable, with some patients experiencing learning disabilities or intellectual disability. The degree of impairment can range widely; some may function well academically while others require substantial support.
Additionally, behavioral problems such as anxiety and attention deficits have been reported. Early intervention through therapies tailored to each individual’s needs can help improve outcomes and enhance quality of life for those affected by ICF Syndrome.
Diagnostic Criteria and Genetic Testing Approaches
ICF Syndrome is diagnosed through a combination of clinical evaluation and genetic testing. The presence of characteristic symptoms, especially facial anomalies and recurrent infections, often prompts further investigation.
Genetic testing focuses on identifying mutations in the DNMT3B gene, which plays a crucial role in DNA methylation. Additional abnormalities may also be explored to confirm the diagnosis.
Flow cytometry can assess immunological function, revealing T-cell deficiencies linked to ICF Syndrome. A multidisciplinary approach ensures accurate diagnosis and guides tailored management strategies for affected individuals.
Differential Diagnosis: Other Combined Immunodeficiencies
Differentiating ICF syndrome from other combined immunodeficiencies is essential for accurate diagnosis and effective management. Conditions such as Severe Combined Immunodeficiency (SCID) present with similar clinical features, including recurrent infections and growth delays.
Other disorders like Hyper-IgM syndrome also exhibit immunological deficiencies but have distinct genetic underpinnings. These include mutations affecting CD40 ligand or related pathways that do not overlap with those seen in ICF.
A thorough evaluation involving family history, clinical presentation, and targeted genetic testing helps pinpoint the exact disorder. Understanding these differences ensures patients receive appropriate therapies tailored to their specific needs.
Treatment Strategies: Managing Immunodeficiency
Managing immunodeficiency in ICF Syndrome requires a multifaceted approach. Patients often benefit from regular monitoring and tailored treatment plans based on their specific needs.
Prophylactic antibiotics are commonly prescribed to reduce the risk of infections. These medications help maintain health by preventing bacteria from taking hold during vulnerable periods.
In some cases, antiviral or antifungal treatments may also be necessary. Supportive therapies can include vaccinations, but these should be approached cautiously due to the weakened immune response in affected individuals. Regular consultations with healthcare professionals ensure that patients receive comprehensive care tailored to their unique circumstances.
Immunoglobulin Replacement Therapy in ICF Syndrome
Immunoglobulin Replacement Therapy (IRT) is a key component in managing ICF Syndrome. This therapy aims to restore the deficient immune function caused by the underlying immunodeficiency.
Patients receive regular infusions of immunoglobulins, which provide essential antibodies to fight infections. These treatments can significantly reduce the frequency and severity of recurrent infections associated with ICF Syndrome.
Regular monitoring is crucial during IRT to assess response and adjust dosages as needed. The ultimate goal is to enhance the patient’s quality of life while minimizing complications from infections that often arise due to their weakened immune system.
Hematopoietic Stem Cell Transplantation: Indications and Outcomes
Hematopoietic stem cell transplantation (HSCT) can be a critical treatment option for individuals with ICF Syndrome. It is particularly indicated in cases where severe immunodeficiency leads to recurrent infections or other complications not manageable through conventional therapies.
The procedure involves replacing defective bone marrow with healthy stem cells, potentially restoring the immune system’s function. HSCT may significantly improve survival rates and reduce infection severity among patients.
Outcomes vary based on several factors, including the patient’s age and overall health at the time of transplant. While many patients experience better immune responses post-transplant, careful monitoring remains essential for managing any long-term effects or complications.
Supportive Care and Infection Prevention
Supportive care plays a vital role in managing ICF Syndrome. It focuses on enhancing the quality of life for patients through regular monitoring and symptom management. Care plans should be tailored to each individual, addressing their specific needs.
Infection prevention is crucial due to the immunodeficiency associated with ICF Syndrome. Patients are more susceptible to infections, making vaccination programs and hygiene practices essential. Regular education about handwashing techniques helps reduce infection risk.
Additionally, caregivers should recognize early signs of illness and seek prompt medical attention when necessary. Collaboration between healthcare providers and families ensures comprehensive support that improves patient outcomes while minimizing complications related to infections.
Prognosis and Long-term Outlook
The prognosis for individuals with ICF Syndrome varies significantly based on the severity of their symptoms and overall health status. Many patients experience recurrent infections, which can complicate their long-term outlook. Early intervention is crucial in managing these complications.
Long-term survival has improved due to advances in treatment strategies such as immunoglobulin replacement therapy and hematopoietic stem cell transplantation. However, some individuals may still face persistent immune challenges.
Additionally, growth and developmental delays can impact quality of life. Ongoing surveillance for neurological issues and other associated conditions is essential to support optimal outcomes for affected individuals.
Genetic Counseling and Prenatal Diagnosis
Genetic counseling plays a vital role for families affected by ICF Syndrome. It provides essential information about inheritance patterns and risks of transmission to future generations. Families can explore their options, leading to informed decisions.
Prenatal diagnosis techniques, such as chorionic villus sampling (CVS) or amniocentesis, allow early detection of genetic conditions like ICF Syndrome. These tests analyze fetal DNA for mutations in genes associated with the syndrome.
Discussing potential outcomes and management strategies is crucial during this process. Genetic counselors support families emotionally while guiding them through available testing options and implications for family planning. This holistic approach ensures that parents are well-equipped to handle any challenges ahead.
Current Research and Emerging Therapies
Current research on ICF Syndrome focuses on understanding the underlying genetic mutations and their impact on disease manifestation. Scientists are exploring how DNMT3B mutations affect DNA methylation, which could lead to innovative therapeutic targets.
Emerging therapies aim to address immunodeficiency and improve patient outcomes. Gene therapy is being investigated as a potential approach to correct the genetic defects responsible for ICF Syndrome.
Additionally, advancements in stem cell research may offer new possibilities for treatment. These studies emphasize collaboration among researchers, clinicians, and families affected by ICF Syndrome to develop effective strategies that enhance care and quality of life for patients.
Quality of Life Considerations for Patients and Families
Quality of life for patients with ICF Syndrome often hinges on comprehensive care. Families must navigate the complexities of ongoing medical needs, which can be overwhelming. Access to specialized healthcare providers is crucial.
Emotional support plays a significant role in enhancing well-being. Counseling services and support groups offer spaces for families to share experiences and coping strategies. These connections help mitigate feelings of isolation.
Educational accommodations are also essential for children affected by ICF Syndrome. Individualized education plans (IEPs) ensure that their unique learning needs are met, fostering an inclusive environment where they can thrive academically and socially.
Patient Registry and Collaborative Research Initiatives
Patient registries and collaborative research initiatives play a vital role in advancing our understanding of ICF Syndrome. These platforms gather valuable data from affected individuals, enabling researchers to identify patterns and improve diagnostic criteria. By sharing information across institutions, scientists can collaborate on clinical trials and investigate new therapeutic options.
Participation in patient registries offers families the opportunity to contribute to groundbreaking studies that may lead to novel treatments. Furthermore, these initiatives foster connections among patients, caregivers, and healthcare professionals, creating a supportive community for those impacted by ICF Syndrome. As research continues to evolve, the collective effort will enhance knowledge about this complex condition and ultimately aim for better health outcomes for patients.