Pregnancy is a beautiful journey, but it can also come with unexpected challenges. One such challenge that every expecting mother should be aware of is HELLP Syndrome. This serious condition can arise during pregnancy and poses significant risks to both mother and baby.
Understanding HELLP Syndrome—its symptoms, causes, and management—is crucial for ensuring the safety of both parties involved. Knowledge empowers you to recognize warning signs early on, paving the way for timely intervention. Let’s dive into what makes HELLP Syndrome so important to know during your pregnancy journey.
HELLP Syndrome Overview: A Life-Threatening Pregnancy Complication
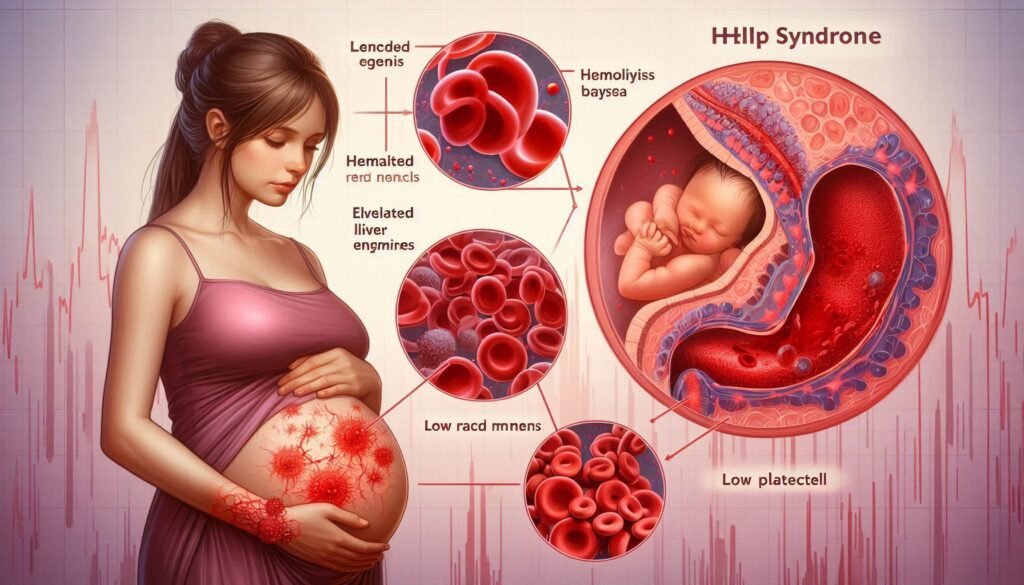
HELLP Syndrome is a serious pregnancy complication that can develop, usually in the third trimester. It stands for Hemolysis, Elevated Liver enzymes, and Low Platelet count. This condition affects about 0.5% to 0.9% of pregnancies but requires immediate medical attention.
“Why Does Yamamoto Syndrome Affect Muscle Function?”
Characterized by liver dysfunction and platelet abnormalities, HELLP Syndrome can lead to severe health issues for both mother and baby if not diagnosed early. Symptoms may include abdominal pain, nausea, headache, and visual disturbances.
Recognizing these signs is vital because HELLP Syndrome can rapidly progress to life-threatening situations such as stroke or liver rupture. Expecting mothers must stay vigilant about their health during pregnancy to ensure timely intervention when needed.
Understanding the HELLP Acronym: Hemolysis, Elevated Liver enzymes, Low Platelet count
HELLP Syndrome is a serious condition characterized by three key components. The acronym stands for Hemolysis, Elevated Liver enzymes, and Low Platelet count. Each element plays a crucial role in understanding the syndrome’s impact on pregnancy.
Hemolysis refers to the breakdown of red blood cells, which can lead to anemia. This may cause fatigue and weakness in expecting mothers. Elevated liver enzymes indicate liver stress or damage, leading to potential complications for both mother and baby.
“How Does Yarhosh Syndrome Impact Development?”
Low platelet count signifies thrombocytopenia, increasing the risk of bleeding disorders. Monitoring these parameters is essential for timely intervention and management during pregnancy, ensuring better outcomes for mothers and their infants alike.
Pathophysiology of HELLP Syndrome
HELLP Syndrome is a complex condition that arises from severe preeclampsia. It involves the dysfunction of blood vessels and the placenta, leading to inadequate blood flow to various organs. This disruption triggers a cascade of inflammatory responses.
Hemolysis occurs when red blood cells are destroyed faster than they can be produced. Elevated liver enzymes indicate liver cell damage, while low platelet counts suggest impaired bone marrow function or increased consumption due to clotting disorders.
“What Causes Yates Syndrome? Complete Guide”
These physiological changes can lead to significant complications for both mother and baby if not promptly identified and managed. Understanding these mechanisms is vital for early intervention and improved outcomes in affected individuals.
Risk Factors and Predisposing Conditions
Several risk factors can increase the likelihood of developing HELLP Syndrome during pregnancy. Women with a history of hypertension or preeclampsia are at heightened risk. Additionally, those who have had HELLP in previous pregnancies may face similar complications.
Age also plays a role; women over 35 years old might be more susceptible to this condition. Furthermore, obesity and certain medical conditions, such as diabetes or kidney disease, can contribute to an increased risk.
“Why Does Yang Syndrome Affect Multiple Systems?”
Genetic predispositions cannot be overlooked either. A family history of hypertensive disorders in pregnancy may elevate the chances of experiencing HELLP Syndrome. Recognizing these factors is crucial for early detection and intervention.
Relationship Between HELLP Syndrome and Preeclampsia
HELLP Syndrome often develops as a severe manifestation of preeclampsia, which is characterized by high blood pressure and organ dysfunction during pregnancy. Both conditions share similar risk factors and can occur concurrently.
The presence of HELLP indicates that the body’s response to preeclampsia has escalated significantly, affecting liver function and platelet levels. Women with preeclampsia are closely monitored for signs of HELLP Syndrome.
“How Does Yashiro Syndrome Present?”
Prompt recognition is crucial since untreated HELLP can lead to serious complications for both mother and baby. Awareness of this relationship helps healthcare providers better manage at-risk pregnancies, ensuring timely interventions when necessary.
Clinical Presentation and Symptoms
HELLP Syndrome often presents with a combination of symptoms that may be mistaken for other pregnancy-related issues. Women typically experience abdominal pain, particularly in the upper right quadrant. This discomfort can be severe and is often accompanied by nausea or vomiting.
Other common signs include headaches, visual disturbances, and fatigue. Patients may also report swelling or edema due to fluid retention.
“What Are The Signs of Y Chromosome Infertility Syndrome?”
As the condition progresses, liver dysfunction may lead to jaundice, characterized by yellowing skin and eyes. It’s crucial for expecting mothers experiencing these symptoms to seek immediate medical attention for proper evaluation and care. Early recognition can significantly impact outcomes for both mother and baby.
Diagnostic Criteria and Laboratory Findings
Diagnosing HELLP Syndrome involves specific laboratory findings alongside clinical symptoms. The primary diagnostic criteria include evidence of hemolysis, elevated liver enzymes, and low platelet count.
Blood tests reveal increased levels of lactate dehydrogenase (LDH) and decreased haptoglobin, indicating hemolysis. Liver enzyme levels – particularly aspartate aminotransferase (AST) and alanine aminotransferase (ALT) – are significantly elevated.
Platelet counts typically drop below 100,000 cells per microliter. Healthcare providers often use a combination of these lab results with the patient’s clinical presentation to confirm HELLP Syndrome effectively. Early recognition is crucial for timely intervention and management during pregnancy.
Differential Diagnosis: Similar Pregnancy Complications
Differentiating HELLP syndrome from other pregnancy complications is crucial for effective management. Conditions such as gestational hypertension and preeclampsia share similar symptoms, including high blood pressure and swelling. However, the presence of hemolysis, elevated liver enzymes, or low platelet counts distinguishes HELLP.
Acute fatty liver of pregnancy (AFLP) is another condition that mimics HELLP but involves severe liver dysfunction without significant hemolysis. Recognizing this difference can significantly impact treatment approaches.
Cholecystitis may also present with abdominal pain in pregnant women. This could confuse clinicians, but specific lab findings help pinpoint the correct diagnosis and ensure appropriate care for both mother and baby.
Management Strategies for HELLP Syndrome
Management of HELLP Syndrome primarily involves timely delivery, which is often the most effective treatment. The decision on timing depends on gestational age and maternal-fetal stability. If the pregnancy is less than 34 weeks, doctors may attempt to stabilize the mother and fetus before proceeding.
Supportive care is crucial during management. This includes monitoring vital signs, laboratory values, and urine output to assess kidney function. Blood transfusions may be necessary in cases of severe anemia or low platelet counts.
Medications like corticosteroids can help mature fetal lungs if early delivery is anticipated. Antihypertensive drugs are also used to control blood pressure effectively while ensuring the safety of both mother and baby during this critical time.
Timing of Delivery: Balancing Maternal and Fetal Risks
Determining the timing of delivery in cases of HELLP Syndrome is critical. Clinicians must carefully weigh the risks to both mother and baby. Often, early delivery is necessary to prevent severe maternal complications.
However, premature birth can pose significant challenges for fetal health. The maturity of the fetus plays a crucial role in this decision-making process. A balance between ensuring maternal safety and providing optimal conditions for neonatal development must be achieved.
In some situations, immediate delivery may take precedence over gestational age, especially if symptoms worsen rapidly. Continuous monitoring helps healthcare providers make informed choices tailored to each unique case while prioritizing well-being on both sides.
Postpartum Course and Monitoring
After delivery, mothers who experienced HELLP Syndrome require careful monitoring. The postpartum course can be complex due to potential lingering effects of the condition. Regular assessments are essential to evaluate liver function and platelet counts.
Healthcare providers often perform blood tests to track any abnormalities. Symptoms such as fatigue, headache, or abdominal pain should be reported immediately, as they may indicate complications. Close observation helps catch issues early.
Patients should also have follow-up appointments to discuss their recovery process. Emotional support is crucial during this time since many women experience anxiety related to their health and the well-being of their newborns. Effective communication with healthcare teams fosters a better recovery experience for mothers after HELLP Syndrome.
Complications of HELLP Syndrome
HELLP Syndrome can lead to several serious complications for both the mother and baby. One of the most critical concerns is liver rupture, which poses a significant risk during pregnancy. This emergency situation requires immediate medical intervention.
Additionally, HELLP Syndrome increases the chance of placental abruption, where the placenta detaches from the uterus prematurely. This condition can result in severe bleeding and jeopardizes fetal health.
For mothers, complications may include renal failure or disseminated intravascular coagulation (DIC), a disorder affecting blood clotting. These risks highlight the need for vigilant monitoring throughout pregnancy when HELLP Syndrome is suspected or diagnosed.
Maternal Outcomes and Prognosis
Maternal outcomes following HELLP syndrome can vary significantly. Many women experience a full recovery, especially with prompt diagnosis and treatment. However, some may face serious complications like liver rupture or kidney failure, which can be life-threatening.
The prognosis largely depends on the severity of the condition at presentation and the effectiveness of management strategies employed. Early intervention often leads to better maternal health outcomes.
Long-term follow-up is essential for mothers who have experienced HELLP syndrome. They may have increased risks for future cardiovascular issues and other health concerns that warrant monitoring by healthcare providers. Regular check-ups ensure ongoing health and well-being in subsequent years.
Fetal and Neonatal Considerations
Fetal and neonatal considerations are critical aspects when managing HELLP Syndrome. The condition can significantly impact fetal well-being, often leading to premature delivery. Early intervention may be necessary to minimize risks.
Babies born to mothers with HELLP Syndrome face potential complications such as low birth weight, respiratory distress syndrome, and even stillbirth in severe cases. Monitoring during pregnancy becomes vital for assessing fetal growth and health.
Neonatal care is essential after delivery. Affected infants may require specialized treatment, including supportive care in a neonatal intensive care unit (NICU). Ensuring close monitoring helps address any immediate health concerns that arise from the mother’s condition.
Long-term Health Implications for Mothers
Women who experience HELLP Syndrome may face long-term health implications that extend beyond pregnancy. Research indicates an increased risk of cardiovascular diseases, metabolic syndrome, and chronic hypertension later in life. These conditions can arise due to the physiological changes triggered by HELLP.
Additionally, studies show that women with a history of HELLP are more likely to develop kidney problems. This is linked to the stress placed on organs during this critical condition. Regular monitoring of kidney function is essential.
Mental health can also be impacted after experiencing HELLP Syndrome. Many mothers report anxiety or post-traumatic stress symptoms related to their pregnancy complications. Addressing these psychological aspects is crucial for holistic recovery.
Recurrence Risk in Subsequent Pregnancies
Women who have experienced HELLP Syndrome are at an increased risk for recurrence in subsequent pregnancies. Studies suggest that the risk can range from 5% to 50%, depending on individual health factors and previous pregnancy complications.
Close monitoring during future pregnancies is essential. Regular check-ups allow healthcare providers to identify early signs of potential issues, enabling timely intervention if necessary.
It’s crucial for expecting mothers to communicate their medical history with their obstetricians. This information guides personalized care plans aimed at minimizing risks associated with HELLP Syndrome reoccurrence while ensuring optimal maternal and fetal outcomes throughout the pregnancy journey.
Preventive Measures and Early Detection
Preventive measures and early detection of HELLP Syndrome are crucial for the health of both mother and baby. Regular prenatal check-ups can help monitor blood pressure and protein levels in urine, indicating potential complications.
Educating mothers about the warning signs is equally important. Symptoms like severe headaches, vision changes, or abdominal pain should prompt immediate medical attention.
Encouraging a healthy lifestyle during pregnancy can also reduce risks. A balanced diet rich in nutrients, regular exercise as advised by healthcare providers, and managing stress contribute to overall well-being. Being proactive about these factors helps ensure better outcomes for expectant mothers experiencing HELLP Syndrome.
Psychological Impact on Patients and Families
The psychological impact of HELLP Syndrome on patients and families can be profound. Expecting mothers may experience anxiety, fear, and depression due to the sudden onset of a serious condition. This emotional turmoil is often exacerbated by uncertainty about their own health and that of their baby.
Families also face significant stress during this challenging time. Partners and relatives may feel helpless or overwhelmed as they navigate medical complexities alongside emotional concerns. Communication becomes crucial; sharing feelings can help alleviate some pressure.
Support systems play an essential role in coping with these challenges. Counseling services and support groups can offer valuable resources for both mothers and families, helping them process their experiences together.
Current Research and Clinical Trials
Current research on HELLP Syndrome is focused on improving diagnosis and management strategies. Clinical trials are exploring the effectiveness of various treatments, including corticosteroids and magnesium sulfate. Researchers aim to identify biomarkers that can predict the onset of HELLP Syndrome early in pregnancy.
Studies are also investigating long-term health implications for affected mothers and their babies. Insight into genetic predispositions may help tailor preventive measures for at-risk populations. Keeping abreast of these developments is crucial for healthcare providers and expecting mothers alike.
As our understanding deepens, it has the potential to significantly enhance maternal-fetal outcomes related to this serious condition. Awareness and education about current findings will empower women with knowledge as they navigate their pregnancies safely.


