Ectodermal Dysplasia Syndrome is a rare genetic condition that can significantly impact an individual’s quality of life. For those unfamiliar with the syndrome, it may seem daunting and complex. However, understanding its implications is vital for early detection and intervention. Early diagnosis not only enhances management strategies but also paves the way for better outcomes in patients.
This blog will explore various facets of Ectodermal Dysplasia Syndrome—from its definition and types to genetic underpinnings and clinical features. We’ll delve into how this condition manifests through hair, skin, teeth, nails and sweat glands while highlighting the importance of a multidisciplinary approach to care. With insights on living with this syndrome and emerging research trends, you’ll gain valuable knowledge that could make all the difference for affected individuals and their families. Join us as we unravel the complexities of Ectodermal Dysplasia Syndrome!

Understanding Ectodermal Dysplasia Syndrome
Ectodermal Dysplasia Syndrome refers to a group of inherited disorders that affect the development of ectodermal structures. These include skin, hair, nails, teeth, and sweat glands. Individuals with this syndrome often face a unique set of challenges due to these developmental anomalies.
The disorder can manifest in various forms depending on which ectodermal structures are impacted. Symptoms may vary widely among affected individuals, leading to differences in appearance and function.
“How Does Iatrogenic Cushing’s Syndrome Develop?”
Understanding the nuances of Ectodermal Dysplasia is crucial for healthcare providers. Early recognition can facilitate timely interventions that significantly improve quality of life for those diagnosed with the syndrome. Awareness also empowers families to seek appropriate support and resources tailored to their specific needs.
Ectodermal Dysplasia Syndrome Definition and Overview
Ectodermal Dysplasia Syndrome is a rare genetic disorder that affects the development of structures derived from the ectoderm, one of the three primary germ layers in embryos. This condition primarily influences skin, hair, nails, teeth, and sweat glands.
Individuals with this syndrome often experience abnormalities across these areas. For instance, they may have sparse or absent hair and missing or malformed teeth. Skin can also display unusual features such as dryness or sensitivity.
“What Causes Idiopathic Hypersomnia Syndrome? Sleep Guide”
The severity and specific symptoms vary widely among those affected. Some individuals may exhibit mild signs, while others face more significant challenges due to extensive manifestations of the syndrome.
Early detection is crucial for managing Ectodermal Dysplasia Syndrome effectively. Identifying it early allows for timely interventions that can significantly improve quality of life and reduce potential complications associated with this condition.
Types of Ectodermal Dysplasia
Ectodermal Dysplasia encompasses a variety of syndromes, each with distinct features. The most common types include X-linked Hypohidrotic Ectodermal Dysplasia (XLHED), which primarily affects males and leads to reduced sweating, hair loss, and dental issues.
Another notable type is Autosomal Dominant Hypohidrotic Ectodermal Dysplasia. This variant can occur in both genders and presents similar symptoms but may vary in severity among individuals.
“Why Does IRIS Syndrome Occur in HIV Patients?”
There are also forms like Anhidrotic Ectodermal Dysplasia that primarily impact sweat glands. Patients often struggle with temperature regulation due to the inability to produce sweat effectively.
Each type has unique inheritance patterns and clinical manifestations, making accurate diagnosis critical for effective management. Understanding these variants helps guide treatment options tailored to the specific needs of those affected by Ectodermal Dysplasia Syndrome.
Genetic Basis of Ectodermal Dysplasia
Ectodermal Dysplasia Syndrome is primarily caused by genetic mutations that affect the development of ectodermal structures. These include hair, nails, teeth, and skin. The underlying genetic factors are crucial for understanding this condition.
Inheritance patterns can vary significantly among families. Some forms are inherited in an X-linked manner, while others follow an autosomal dominant or recessive pattern. This complexity complicates diagnosis and family planning.
“How Does Inflammatory Bowel Disease Syndrome Affect Digestion?”
Genetic mutations leading to Ectodermal Dysplasia often occur in genes like EDA, EDAR, and EDARADD. Identifying these mutations can aid in establishing a definitive diagnosis.
Genetic testing plays a vital role in confirming suspicions of Ectodermal Dysplasia Syndrome. Families may benefit from genetic counseling to understand risks and implications for future generations.
Inheritance Patterns
Inheritance patterns of ectodermal dysplasia syndrome can vary significantly. Most commonly, it follows an X-linked recessive pattern. This means that males are more frequently affected than females.
In this case, the gene responsible for the condition is located on the X chromosome. Males have only one X chromosome, so a single mutated copy leads to symptoms. Females, having two X chromosomes, may be carriers without showing signs if they possess one normal gene.
“What Is Inclusion-Cell Syndrome? Complete Guide”
Autosomal dominant inheritance is another possibility but is less common. Here, only one mutated copy from either parent can cause the disorder in both males and females equally.
Furthermore, autosomal recessive inheritance also exists within certain types of ectodermal dysplasia syndromes. Both parents must carry a mutated gene for a child to express symptoms under this pattern. Understanding these inheritance mechanisms helps families anticipate risks and make informed decisions regarding genetic counseling.
Genetic Mutations
Genetic mutations play a crucial role in the development of Ectodermal Dysplasia Syndrome. These mutations often occur in specific genes responsible for ectodermal structures like hair, teeth, skin, and nails.
Most commonly affected genes include EDA, EDAR, and EDARADD. Mutations in these genes disrupt the normal formation and function of ectodermal tissues. This can lead to various physical manifestations associated with the syndrome.
“Why Does Immune Dysregulation Syndrome Occur?”
The nature of these mutations can vary widely—from small changes in DNA sequences to larger deletions or duplications. Each type affects individuals differently based on which gene is altered.
Understanding these genetic underpinnings aids healthcare professionals in diagnosing the condition more accurately. It also paves the way for potential future treatments that target specific genetic anomalies linked to Ectodermal Dysplasia Syndrome.
Genetic Testing and Counseling
Genetic testing plays a crucial role in diagnosing Ectodermal Dysplasia Syndrome. It helps identify specific mutations associated with the condition, providing valuable insights for families. Testing can confirm a diagnosis when clinical features are present but unclear.
“How Does ICF Syndrome Affect Immunity? Expert Guide”
Counseling is equally essential. Genetic counselors guide individuals and families through the complexities of genetic information. They explain test results clearly, helping to interpret their implications on health and family planning.
Moreover, counseling offers emotional support during what can be an overwhelming process. Families often have questions about inheritance patterns or risks for future children.
By combining genetic testing with counseling, affected individuals gain a better understanding of Ectodermal Dysplasia Syndrome. This proactive approach empowers patients and families to make informed decisions regarding management and treatment options tailored to their needs.
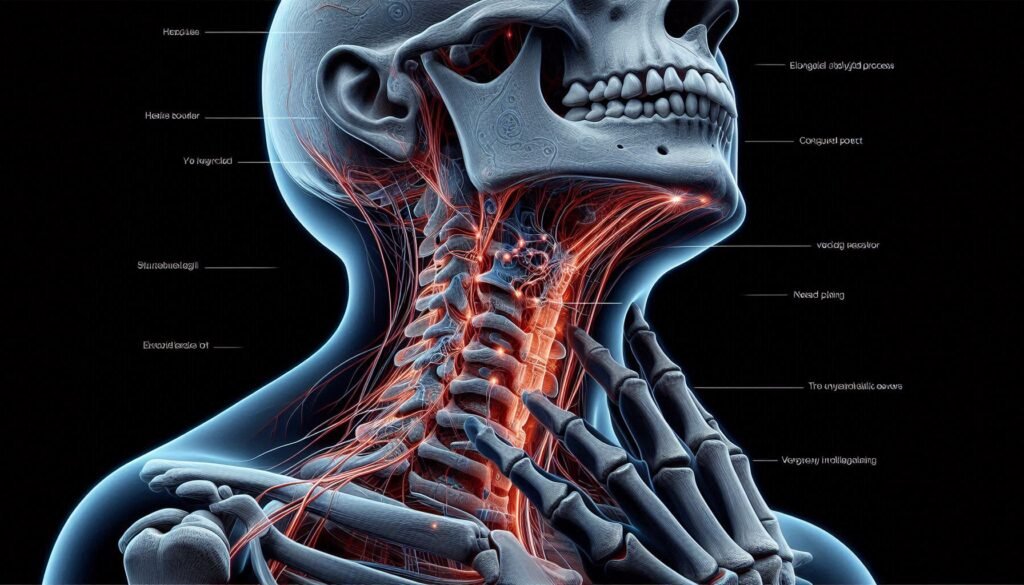
Ectodermal Dysplasia Syndrome Clinical Features and Symptoms
Ectodermal Dysplasia Syndrome presents a variety of clinical features that can significantly impact daily life. One primary symptom is hair abnormalities, where individuals may experience sparse or absent hair on the scalp and body.
Dental issues are also common, with many affected individuals having malformed teeth or missing teeth altogether. This can lead to difficulties in chewing and speaking.
“What Causes Jackson-Weiss Syndrome? Bone Development Guide”
Skin problems often manifest as dry skin or an inability to sweat properly. The lack of sweat glands creates challenges in regulating body temperature.
Nail anomalies may include ridges, pits, or complete absence of nails.
Sweat gland dysfunction further complicates matters by leading to overheating during physical activities. Each symptom presents its own set of challenges, making early detection crucial for effective management strategies tailored to individual needs.
Hair Abnormalities
Hair abnormalities are a hallmark of Ectodermal Dysplasia Syndrome. Individuals may experience sparse hair growth or total absence of hair, known as alopecia. This condition can affect the scalp as well as other areas of the body.
The texture and quality of existing hair often differ significantly from typical standards. Hair may appear fine, brittle, or lacking luster. The irregularities stem from developmental issues in hair follicles during embryonic stages.
In some cases, individuals might also face changes in pigmentation, leading to lighter or differently colored strands compared to their natural shade. These variations can impact self-esteem and social interactions.
Addressing these concerns is essential for psychosocial well-being. Specialized treatments and cosmetic solutions are available to help manage appearance and boost confidence among those affected by this syndrome.
Dental Issues
Dental issues are a hallmark of Ectodermal Dysplasia Syndrome. Individuals often experience a range of problems related to their teeth and oral health.
One common concern is the absence of teeth, known as hypodontia or anodontia. Many affected individuals have missing permanent teeth, which can impact chewing and speech development.
Moreover, the remaining teeth may be malformed or improperly aligned. This irregularity can lead to difficulties in maintaining hygiene, increasing the risk of cavities and gum disease.
Frequent dental visits are essential for those with this syndrome. Customized interventions such as dental crowns or implants may be necessary to improve function and aesthetics.
Early detection allows for tailored treatment plans that address these unique challenges effectively. By prioritizing dental care from an early age, individuals can enhance their quality of life significantly.
Skin Problems
Individuals with Ectodermal Dysplasia Syndrome often experience a range of skin problems. These can manifest as thin, dry, or fragile skin. The reduced sweat glands lead to difficulty regulating body temperature and increased risk of overheating.
Skin may also become more prone to infections due to compromised barrier function. Lesions, rashes, or other irritations can arise more easily in individuals affected by this syndrome.
Hypopigmentation is another common issue where areas of the skin lack color compared to surrounding patches. This results from an absence of melanin production, leading to lighter spots that are particularly visible on sun-exposed areas.
Managing these symptoms requires careful skincare routines tailored for sensitive skin types. Regular moisturizing and gentle cleansing help alleviate dryness and protect against environmental factors while promoting overall comfort.
Nail Abnormalities
Nail abnormalities are a common manifestation of Ectodermal Dysplasia Syndrome. Individuals may experience thin, brittle nails that are prone to splitting and breaking easily. This can lead to discomfort and self-esteem issues.
The shape of the nails may also be affected. They could appear ridged or have an unusual curvature, which differs from typical nail anatomy. Some people might even notice a reduction in the number of fingernails or toenails present.
These changes often stem from the underlying genetic mutations associated with ectodermal dysplasia affecting skin appendages. Proper care is essential for managing these symptoms effectively.
Regular moisturizing can help improve nail health and prevent further damage. Consulting with healthcare providers specializing in dermatology can provide tailored advice on treatment options specific to each individual’s needs.
Sweat Gland Dysfunction
Sweat gland dysfunction is a significant concern for individuals with Ectodermal Dysplasia Syndrome. This condition often leads to an inability to produce sweat effectively, which can complicate temperature regulation.
Without adequate sweating, the body struggles to cool down during physical activities or in hot environments. As a result, affected individuals may experience overheating or heat intolerance.
This lack of thermal regulation poses risks during exercise or warm weather, as it can lead to heat exhaustion or even heat stroke if precautions aren’t taken.
Moreover, this dysfunction can impact daily life and overall comfort levels. It’s essential for caregivers and patients alike to be aware of these challenges and implement strategies that help manage body temperature effectively while maintaining safety in various situations.
Diagnosis of Ectodermal Dysplasia
Diagnosing Ectodermal Dysplasia Syndrome requires a comprehensive approach. It often starts with a clinical evaluation by a healthcare professional who specializes in genetic disorders. Observing the physical features associated with this syndrome is crucial, as these can indicate its presence.
Genetic testing methods play an essential role in confirming the diagnosis. These tests analyze DNA to identify specific mutations linked to ectodermal dysplasia. By pinpointing these genetic anomalies, doctors can provide more accurate diagnoses and tailored management plans.
For expectant parents or those at high risk, prenatal diagnostic options are available. Techniques such as chorionic villus sampling (CVS) or amniocentesis allow for early detection of potential abnormalities in fetus development related to ectodermal dysplasia syndromes, offering vital information before birth. This proactive approach enables families to prepare for any necessary interventions right from infancy.
Clinical Evaluation
Clinical evaluation is a critical step in diagnosing Ectodermal Dysplasia Syndrome. Physicians begin by gathering detailed medical histories, focusing on family backgrounds and any observable symptoms.
During the examination, doctors assess physical features closely. They look for characteristic signs such as sparse hair, missing teeth, or skin irregularities. Observations from parents regarding developmental milestones are also essential.
Moreover, healthcare providers often utilize specific criteria to confirm diagnoses. These include evaluating sweat gland function and assessing dental health through X-rays or other imaging techniques.
A multidisciplinary approach may be employed during this process to ensure comprehensive care. Collaborating with dermatologists and dentists can help draw a clearer picture of the condition’s impact on an individual’s life.
This thorough clinical evaluation lays the groundwork for further testing and tailored management plans suited to individuals’ needs.
Genetic Testing Methods
Genetic testing methods for Ectodermal Dysplasia Syndrome vary in complexity and purpose. One common approach is targeted gene sequencing, which focuses on specific genes known to be associated with the condition. This method allows for a precise identification of mutations.
Another technique is whole exome sequencing. It examines all coding regions of the genome, providing a broader perspective on potential genetic causes that may not have been considered previously.
Additionally, chromosomal microarray analysis can detect large deletions or duplications in DNA that might contribute to the syndrome’s symptoms. This comprehensive approach offers insights into complex cases where traditional methods fall short.
Testing typically begins with a clinical evaluation followed by counseling to discuss options and implications. These advanced techniques can facilitate early diagnosis and appropriate management strategies tailored to individual needs.
Prenatal Diagnosis
Prenatal diagnosis of Ectodermal Dysplasia Syndrome involves advanced screening techniques to identify potential genetic abnormalities before birth. These methods are essential for at-risk families, especially when there is a known family history.
Ultrasound plays a crucial role in this process. It can reveal physical anomalies associated with the syndrome, such as unusual hair patterns or skin conditions. However, these signs may not always be definitive indicators.
Amniocentesis and chorionic villus sampling (CVS) are more invasive procedures used for genetic testing during pregnancy. They allow healthcare providers to analyze fetal DNA for mutations linked to ectodermal dysplasia.
Early identification enables parents to prepare for the challenges ahead and seek appropriate medical care immediately after birth. Genetic counseling also provides invaluable support by helping families understand their options and make informed decisions regarding prenatal care and management strategies.
Ectodermal Dysplasia Management and Treatment Approaches
Managing Ectodermal Dysplasia Syndrome requires a tailored approach focusing on individual symptoms. Dental care is often a priority, as many affected individuals experience missing or malformed teeth. Early intervention with prosthodontics can significantly improve function and aesthetics.
Skin and hair management plays a vital role in treatment. Regular moisturizing and appropriate shampoos help alleviate dryness and irritation, while protective clothing aids against sun exposure.
Temperature regulation strategies are crucial due to sweat gland dysfunction. Cooling vests or fans can assist during hot weather, ensuring comfort for those affected.
Respiratory care should not be overlooked. Maintaining clear airways through regular check-ups helps prevent infections associated with respiratory issues common in this syndrome.
A multidisciplinary team—including dentists, dermatologists, geneticists, and mental health professionals—ensures comprehensive support tailored to the unique needs of each patient living with Ectodermal Dysplasia Syndrome.
Dental Care and Interventions
Dental care is crucial for individuals with Ectodermal Dysplasia Syndrome. Due to the congenital absence of teeth or abnormal tooth formation, these individuals often face unique challenges.
Early dental interventions are essential. Regular check-ups help monitor oral health and address issues promptly. Pediatric dentists experienced in managing ectodermal dysplasia can recommend tailored treatment plans.
Prosthetics may be necessary for those missing teeth. These devices not only enhance aesthetics but also improve functionality when chewing and speaking.
Preventive measures are vital as well. Maintaining strict oral hygiene practices minimizes the risk of decay and gum disease, which can exacerbate existing problems.
Fluoride treatments might be beneficial in strengthening enamel if present, further protecting vulnerable teeth from damage or decay. Educating patients about proper brushing techniques is equally important to foster long-term oral health habits.
Skin and Hair Management
Managing skin and hair in individuals with Ectodermal Dysplasia Syndrome requires a tailored approach. Due to the condition’s impact on sweat glands, maintaining skin hydration is crucial. Regular use of emollient creams helps combat dryness and prevents irritation.
For hair care, gentle shampoos and conditioners are recommended to avoid further damage. Individuals may experience thinning or absent hair, so styles that require less manipulation can promote healthier growth.
Sun protection is essential as well. Sensitive skin can easily burn; therefore, applying sunscreen before going outdoors protects against harmful UV rays.
Regular dermatological check-ups enable early identification of potential issues, allowing for prompt intervention when necessary. This proactive strategy supports both comfort and overall quality of life for those affected by this syndrome.
Temperature Regulation Strategies
Temperature regulation is crucial for individuals with Ectodermal Dysplasia Syndrome due to their reduced sweat gland function. Lack of sweating can lead to overheating, especially in hot weather or during physical activity.
One effective strategy is staying hydrated. Drinking plenty of fluids helps maintain body temperature and replace lost moisture. Cold drinks or ice chips can provide immediate relief.
Wearing breathable clothing made from natural fibers also aids in temperature control. Loose-fitting garments help air circulate around the skin, allowing for better cooling.
Using fans and air conditioning indoors creates a more comfortable environment. This ensures that temperatures remain manageable, reducing the risk of heat-related complications.
During outdoor activities, planning outings during cooler parts of the day can make a significant difference. Shade and frequent breaks are essential for preventing overheating while enjoying time outside.
Respiratory Care
Respiratory care is a crucial aspect of managing Ectodermal Dysplasia Syndrome. Individuals with this condition may face challenges due to structural abnormalities affecting their airways.
Regular evaluations by a respiratory specialist can help identify specific issues early on. These assessments often include pulmonary function tests and imaging studies.
Implementing strategies such as proper hydration, humidification, and using saline nasal sprays can aid in maintaining airway moisture. This approach helps improve overall lung function.
In some cases, physical therapy focused on breathing exercises can enhance respiratory strength. Families should be educated about recognizing signs of respiratory distress to ensure timely intervention.
Maintaining an allergen-free environment is also essential for those affected by this syndrome. It reduces the likelihood of complications related to asthma or bronchitis while promoting better health outcomes overall.
Multidisciplinary Care Approach
A multidisciplinary care approach is essential for managing Ectodermal Dysplasia Syndrome effectively. This strategy involves a team of healthcare professionals from various specialties working together to address the diverse needs of individuals with this condition.
Dentists play a crucial role, providing interventions such as custom prosthetics and orthodontic treatments to tackle dental issues commonly seen in patients. Dermatologists are vital for managing skin problems, offering therapies that enhance skin health and comfort.
Speech therapists may assist those facing feeding difficulties or speech delays. Additionally, genetic counselors guide families through understanding inheritance patterns and available testing options.
This collaborative effort ensures comprehensive care tailored to each patient’s unique challenges. By uniting their expertise, these professionals can improve outcomes and enhance the quality of life for individuals affected by Ectodermal Dysplasia Syndrome.
Living with Ectodermal Dysplasia
Living with Ectodermal Dysplasia presents unique challenges for individuals and their families. The early years can be particularly difficult as children navigate social interactions while coping with physical differences.
Support from family, friends, and medical professionals is crucial during childhood. Encouraging open communication about the condition fosters understanding and acceptance among peers.
As adolescents transition into adulthood, they may face additional hurdles related to self-esteem and identity. Ongoing support can help them develop resilience.
Psychosocial factors play a significant role in managing life with this syndrome. Accessing mental health resources ensures that emotional well-being is prioritized alongside physical care.
Engagement in community groups or online forums offers valuable connections for sharing experiences and advice. These networks provide an essential sense of belonging for those affected by Ectodermal Dysplasia Syndrome.
Childhood Challenges
Children with Ectodermal Dysplasia Syndrome face unique challenges that can affect their daily lives. One of the most significant hurdles is dealing with dental issues. Many children experience abnormal tooth development, leading to missing or misshapen teeth. This can impact their self-esteem and social interactions.
Skin problems also present difficulties. Children may have sensitive skin prone to irritation, making everyday activities uncomfortable. Proper skincare routines are essential but can be hard for young ones to maintain consistently.
Additionally, hair abnormalities contribute to feelings of difference among peers. Sparse or absent hair might lead some kids to feel self-conscious in social settings.
Managing temperature regulation poses a challenge due to sweat gland dysfunction. Parents often need strategies in place for hot weather, ensuring their child stays cool and comfortable during outdoor playtime or school activities.
Adolescent and Adult Care
Adolescents and adults with Ectodermal Dysplasia Syndrome face unique challenges. As they grow, their physical appearance can affect self-esteem and social interactions. Supportive counseling is essential during these formative years.
Regular dental care becomes increasingly important. Many individuals may require orthodontic treatment or prosthetics to address missing teeth. Maintaining oral hygiene is crucial for overall health.
Skin and hair management should also be prioritized. Tailored skincare routines can alleviate discomfort from dryness or sensitivity. Finding appropriate hairstyles that complement any hair loss can boost confidence.
Temperature regulation remains a key concern in adulthood, as sweat gland abnormalities persist. Staying hydrated and wearing suitable clothing are vital strategies for managing heat intolerance.
Encouraging independence while providing emotional support fosters resilience in navigating life’s complexities related to Ectodermal Dysplasia Syndrome. Accessing community resources can further enhance quality of life for these individuals as they transition into adulthood.
Psychosocial Aspects
Living with Ectodermal Dysplasia Syndrome can pose unique psychosocial challenges. Individuals may face social stigma due to visible differences, such as hair loss or dental issues. This can lead to feelings of isolation and anxiety.
Children with the syndrome might struggle to fit in with peers, leading to low self-esteem. Supportive families and communities play a vital role in helping them navigate these challenges. Open communication about their condition fosters understanding and acceptance.
Adolescents often grapple with identity formation while managing their symptoms. They may require additional emotional support during this critical developmental stage.
Accessing mental health resources is essential for coping strategies. Therapy or counseling can provide valuable tools for resilience against societal pressures and personal struggles associated with Ectodermal Dysplasia Syndrome.
Associated Complications
Ectodermal Dysplasia Syndrome can lead to various complications that impact quality of life. One significant concern is respiratory issues. Individuals may experience frequent infections or difficulty breathing due to structural abnormalities in the airways.
Feeding difficulties are common in infants with this syndrome, often resulting from dental anomalies and oral malformations. These challenges can lead to inadequate nutrition and growth concerns if not addressed early.
Hearing and vision problems also present additional hurdles for those affected by Ectodermal Dysplasia Syndrome. Hearing loss might stem from ear canal abnormalities, while visual impairments could arise from eye conditions associated with the disorder.
Addressing these complications requires a proactive approach, involving multiple healthcare professionals working together to provide comprehensive care tailored to individual needs.
Respiratory Issues due to Ectodermal Dysplasia Syndrome
Individuals with Ectodermal Dysplasia Syndrome often face various respiratory challenges. These issues can stem from structural anomalies in the airways or reduced immune function. As a result, patients may experience recurrent respiratory infections and complications.
The absence of normal hair follicles affects the nasal passages’ filtration system, making it easier for pathogens to enter the lungs. This can lead to increased susceptibility to conditions like asthma or bronchitis.
Additionally, some individuals might exhibit poor development of sinuses, which further exacerbates breathing difficulties and contributes to chronic sinusitis.
Early detection is crucial for managing these respiratory concerns effectively. Interventions such as pulmonary rehabilitation or targeted therapies can improve quality of life significantly and prevent severe complications down the line. Regular monitoring also plays a vital role in ensuring that any emerging issues are addressed promptly.
Feeding Difficulties in Infants
Feeding difficulties in infants with Ectodermal Dysplasia Syndrome can pose significant challenges. Many babies may struggle to latch properly during breastfeeding due to oral abnormalities, such as missing teeth or malformed gums.
This can lead to frustration for both the infant and the caregiver. Formula feeding might also become complicated, especially if there are issues with sucking or swallowing.
Parents often notice that their child exhibits signs of discomfort while eating. This could result from sensitivity around the mouth or throat, making meals a stressful experience instead of a bonding one.
Additionally, these children may have difficulty transitioning to solid foods later on. Textures and tastes that seem normal for other infants could be overwhelming for those affected by this syndrome, requiring careful introduction and patience from caregivers.
Addressing these challenges early on is vital, ensuring proper nutrition and promoting healthy growth in infants dealing with Ectodermal Dysplasia Syndrome.
Hearing and Vision Problems
Individuals with Ectodermal Dysplasia Syndrome may face hearing and vision problems. These complications arise due to the syndromic nature of the condition, which affects multiple body systems.
Hearing difficulties can manifest as conductive or sensorineural loss. Structural abnormalities in the ear can hinder sound transmission. As a result, early intervention through audiological assessments is crucial.
Vision issues are also common among those affected. Problems may include refractive errors, such as myopia or hyperopia, necessitating corrective lenses. Additionally, some individuals might experience cataracts or other ocular anomalies that require monitoring and treatment.
Regular screenings for both hearing and vision are vital for managing these challenges effectively. Identifying issues early allows for timely interventions that enhance quality of life and support overall development in children with Ectodermal Dysplasia Syndrome.
Research and Future Prospects
Research in Ectodermal Dysplasia Syndrome is evolving rapidly. Scientists are exploring gene therapy as a potential game-changer for affected individuals. This approach aims to correct genetic mutations responsible for the syndrome, potentially restoring normal function.
Improving diagnostic techniques is also crucial. Advanced imaging and biomarker identification can lead to earlier detection, which enhances treatment outcomes significantly. The goal is to develop non-invasive methods that provide accurate diagnoses without unnecessary stress on families.
Furthermore, there’s an ongoing effort to create new treatment options tailored specifically for patients with ectodermal dysplasia. Researchers are investigating innovative therapies that address not just symptoms but also underlying causes of the condition, paving the way for more comprehensive care strategies in the future.
These advancements hold promise for improving quality of life and health management among those living with this syndrome. Continued research will shape how we understand and treat ectodermal dysplasia moving forward.
Gene Therapy Potential
Gene therapy represents a promising frontier in the management of Ectodermal Dysplasia Syndrome. This innovative approach aims to address the root cause by correcting genetic mutations responsible for this condition.
By delivering functional copies of affected genes directly into patients’ cells, gene therapy has the potential to restore proper protein function. This could lead to improvements in symptoms associated with hair, teeth, and skin abnormalities.
Research is still in its early stages, but initial studies indicate that targeted therapies may one day provide lasting solutions. Advances in techniques such as CRISPR-Cas9 are enhancing our ability to edit genes precisely and safely.
As scientists continue exploring these possibilities, they hope that gene therapy will become a viable option for those living with Ectodermal Dysplasia Syndrome. The future looks bright as we uncover new strategies to combat this complex condition through genetic advancements.
Improving Diagnostic Techniques
Improving diagnostic techniques for Ectodermal Dysplasia Syndrome is crucial for timely intervention. Advanced imaging technologies, such as high-resolution MRI and 3D facial scanning, can provide detailed insights into physical manifestations.
Additionally, the role of artificial intelligence in analyzing genetic data cannot be overlooked. AI algorithms can swiftly identify patterns linked to specific mutations associated with ectodermal dysplasia.
Moreover, developing comprehensive screening protocols that focus on early symptoms enhances detection rates. Healthcare providers should be trained to recognize subtle signs during routine pediatric check-ups.
Collaboration among geneticists, dermatologists, and dental specialists also plays an essential part in refining diagnosis methods. A multidisciplinary approach ensures all aspects of the syndrome are evaluated thoroughly.
As research continues, integrating these innovative techniques will pave the way for more accurate diagnoses and better outcomes for affected individuals.
Developing New Treatment Options
Developing new treatment options for Ectodermal Dysplasia Syndrome remains a critical area of research. Scientists are exploring innovative therapies that target the underlying genetic mutations responsible for this condition. Advances in gene therapy hold promise, potentially allowing for corrections at the DNA level.
Furthermore, researchers are investigating ways to improve existing management strategies through personalized medicine approaches. This includes tailoring treatments based on individual symptoms and needs, which could enhance the quality of life for those affected by Ectodermal Dysplasia.
Collaboration between medical professionals and researchers is essential to push forward these advancements. Continued investment in clinical trials will pave the way for discovering effective interventions that address both physical manifestations and psychosocial aspects of living with this syndrome.
The hope is that ongoing studies will yield breakthroughs not only in symptom management but also in preventive measures. As awareness grows, so does the potential for significant improvements in care and support systems available to individuals diagnosed with Ectodermal Dysplasia Syndrome.