Introduction to De Quervain Syndrome (De Quervain’s Tenosynovitis)
De Quervain Syndrome, also known as De Quervain’s Tenosynovitis, is a condition affecting the tendons at the base of your thumb. It can cause pain and discomfort that interferes with daily activities like gripping objects or even turning a door handle. If you’ve been experiencing persistent thumb and wrist pain, you might be wondering what’s going on.
This comprehensive guide will unravel the complexities of De Quervain Syndrome, offering insights into its causes, symptoms, diagnosis, and treatment options. Whether you’re seeking information for yourself or someone else dealing with this painful condition, you’ll find valuable knowledge to help navigate through it all. Get ready to explore what De Quervain Syndrome means for patients today!
Definition and Anatomy of De Quervain Syndrome
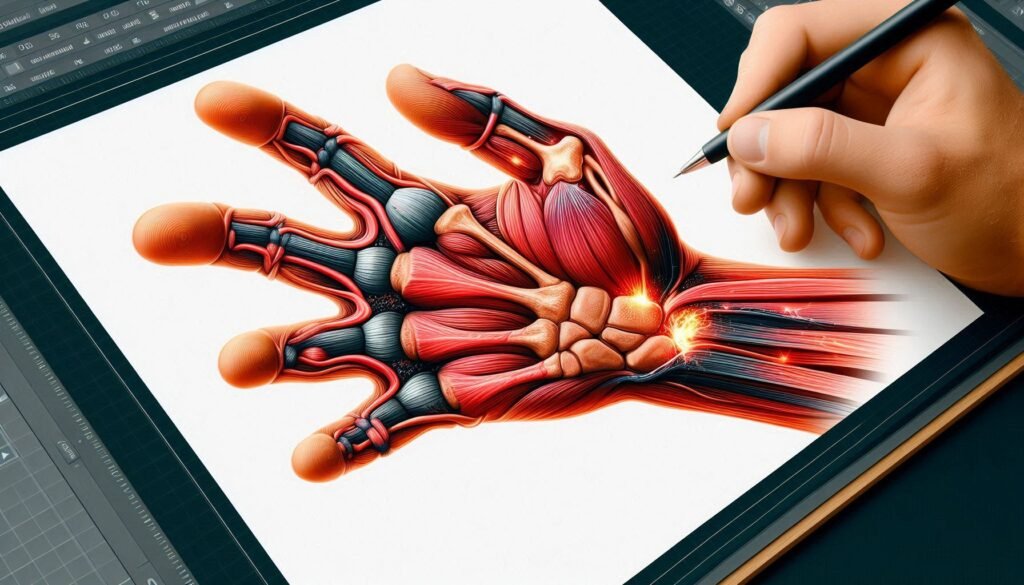
De Quervain Syndrome is a painful condition affecting the tendons located at the base of the thumb. It occurs when these tendons become inflamed in their synovial sheath, creating discomfort and limiting mobility.
Anatomically, this syndrome involves two primary tendons: the abductor pollicis longus (APL) and extensor pollicis brevis (EPB). These tendons play crucial roles in thumb movement and wrist function. When repetitive movements or excessive use occur, irritation develops around these structures.
“How Does Down Syndrome Affect Development? Complete Guide”
The inflammation can lead to swelling and pain that radiates from the wrist to the lower part of the thumb. Recognizing this anatomy helps understand how everyday activities may exacerbate symptoms. Addressing underlying issues early can prevent further complications related to De Quervain Syndrome.
Historical Background and Namesake
De Quervain’s Tenosynovitis, is named after the Swiss surgeon Fritz de Quervain. He first described this condition in 1895. His work focused on inflammation of the tendons around the thumb and wrist.
Fritz de Quervain’s detailed observations laid the foundation for understanding how repetitive motion affects tendon health. The syndrome was characterized by pain along the radial side of the wrist. This significant breakthrough helped shape future research and treatment approaches.
“What Are The Signs of De Barsy Syndrome in Infants?”
Over time, medical professionals recognized that specific activities could lead to this painful condition. As awareness grew, so did interest in effective management strategies. Today, both clinicians and patients have a better grasp of its origins and implications thanks to de Quervain’s pioneering contributions to medicine.
Causes and Risk Factors of De Quervain’s Tenosynovitis
De Quervain’s Tenosynovitis often arises from repetitive movements and overuse of the wrist and thumb. Activities such as typing, sewing, or playing musical instruments can strain the tendons.
Hormonal influences also play a role. Women are more likely to develop this condition during pregnancy or postpartum due to changes in hormone levels affecting tendon health.
“How Does Dejerine-Roussy Syndrome Cause Chronic Pain?”
Anatomical variations can increase susceptibility too. Some individuals might have a tighter anatomical space around their tendons, leading to irritation and inflammation.
Age is another factor; those between 30-50 years old are commonly affected. Additionally, certain medical conditions like rheumatoid arthritis may predispose individuals to De Quervain Syndrome by causing inflammation in nearby tissues. Understanding these causes helps with early identification and management of symptoms.
Repetitive Movements and Overuse
Repetitive movements are a common culprit behind De Quervain Syndrome. Tasks that require constant thumb or wrist usage can strain the tendons in this area. Activities like texting, typing, or even knitting can lead to irritation and inflammation over time.
The condition often arises from overuse in daily routines. Individuals who perform repetitive actions without proper breaks may experience discomfort as the tendons become overloaded. This chronic stress can trigger symptoms associated with De Quervain’s Tenosynovitis.
“What Causes DiGeorge Syndrome? Immune System Guide”
It’s essential to listen to your body when engaging in these activities. If you notice persistent pain or swelling, it might be time to adjust your routine. Incorporating periodic rest into tasks can significantly reduce the risk of developing this painful syndrome and improve overall hand health.
Hormonal Influences of De Quervain’s Tenosynovitis
Hormonal influences play a notable role in the development of De Quervain’s Tenosynovitis. Women, particularly during pregnancy and after childbirth, are more susceptible to this condition. The fluctuations in estrogen and relaxin hormones can affect tendon health.
Estrogen is known to impact collagen synthesis within tendons. When levels fluctuate, they may lead to increased laxity or inflammation around the tendons in the wrist and thumb area.
“Why Does Eagle Syndrome Cause Throat Pain? Expert Guide”
During pregnancy, hormonal changes often cause fluid retention and swelling. This additional pressure can exacerbate existing conditions or trigger new ones like De Quervain’s.
Postpartum women frequently experience heightened stress on their wrists due to activities such as lifting infants or repetitive motions involved in caregiving. These factors create an environment where hormonal shifts contribute significantly to pain and discomfort associated with this syndrome.
Anatomical Variations of De Quervain Syndrome
Anatomical variations can significantly influence the development of De Quervain Syndrome. The tendons responsible for thumb movement, specifically the abductor pollicis longus and extensor pollicis brevis, may have different anatomical paths in individuals.
Some people possess additional muscle bellies or variations in tendon attachments that increase friction within the wrist compartment. These differences can lead to an increased likelihood of irritation and inflammation.
“What Is Ectodermal Dysplasia Syndrome? Complete Guide”
Furthermore, bony structures like a prominent styloid process or changes in joint alignment can contribute to compression around these tendons. Recognizing these anatomical nuances is crucial for understanding how they might predispose someone to develop this painful condition.
Individual assessments often reveal unique characteristics that play a role in symptom presentation and treatment options. Tailored approaches are essential for effectively managing De Quervain Syndrome based on each person’s anatomy.
Signs and Symptoms of De Quervain’s Tenosynovitis
De Quervain’s Tenosynovitis manifests through distinct signs and symptoms that can significantly affect daily activities.
One of the primary indicators is pain located at the base of the thumb. This discomfort may radiate into the wrist or forearm, making simple tasks challenging.
Swelling and tenderness around the affected area are also common. The soft tissues may feel warm to touch, indicating inflammation.
“How Does Ehlers-Danlos Syndrome Affect Connective Tissue?”
Patients often experience difficulty with grip and pinch movements. Actions like holding a cup or turning a doorknob can become painful or awkward.
Additionally, pain typically worsens during thumb and wrist motion. Activities involving lifting or twisting motions tend to exacerbate discomfort, leading individuals to seek relief more urgently as their daily routine is disrupted.
Pain at the Base of the Thumb
Pain at the base of the thumb is one of the hallmark signs of De Quervain Syndrome. This discomfort often manifests as a sharp, aching sensation that can radiate into the wrist or down along the forearm.
Patients may notice that simple tasks—like gripping objects, turning keys, or even holding a cup—can exacerbate this pain. The thumb’s extensive use in daily activities makes it particularly vulnerable to strain and inflammation.
“What Causes Eale’s Disease Syndrome? Vision Loss Guide”
In many cases, this pain worsens during specific movements. Activities that involve repetitive gripping motions are especially problematic. As inflammation increases, individuals might find it challenging to perform everyday functions without discomfort.
Recognizing this symptom early on is crucial for effective management and treatment options. Addressing it promptly can help prevent further complications associated with De Quervain’s Tenosynovitis.
Swelling and Tenderness
Swelling and tenderness are hallmark signs of De Quervain Syndrome. Patients often notice a noticeable puffiness around the base of the thumb, primarily where the tendons run through their protective sheath.
This swelling occurs due to inflammation within the tendon sheaths. As these tendons become irritated from overuse, they can swell, pressing against surrounding structures. This pressure contributes to discomfort and pain during movement.
Tenderness typically accompanies this swelling. Many individuals report sensitivity when touching or applying pressure near the affected area. Simple tasks like gripping objects or turning doorknobs may exacerbate this sensation.
Recognizing these symptoms early is vital for effective management. If you experience persistent swelling and tenderness in your wrist or thumb region, seeking professional evaluation can help prevent further complications.
Difficulty with Grip and Pinch Movements
Difficulty with grip and pinch movements is a hallmark of De Quervain Syndrome. Individuals often experience an aching sensation that makes simple tasks seem daunting. This can include opening jars, holding utensils, or even grasping a pen.
The pain typically radiates from the base of the thumb towards the wrist, causing discomfort during these everyday activities. As inflammation worsens, it becomes increasingly challenging to perform actions requiring fine motor skills.
Patients may find themselves adapting their techniques unconsciously. For instance, they might use larger motions instead of precise grips to avoid triggering pain. Unfortunately, this compensatory behavior can lead to further strain on surrounding muscles and tendons.
Recognizing this difficulty early is essential for effective management and recovery strategies tailored specifically for those affected by De Quervain’s Tenosynovitis.
Pain Worsening with Thumb and Wrist Motion
Pain associated with De Quervain Syndrome often intensifies during thumb and wrist motion. This discomfort typically arises from irritation of the tendons surrounding the thumb as they glide through a narrow compartment at the wrist.
Simple tasks like gripping an object or twisting your wrist can become excruciating. Patients frequently report sharp pain that radiates along the forearm, particularly when performing actions such as writing or lifting items.
The underlying inflammation constricts tendon movement, leading to increased friction and subsequent pain. It can be frustrating since everyday activities, from opening jars to texting, may aggravate this condition further.
Recognizing this symptom is crucial for timely intervention. Addressing it early on can help prevent more severe limitations in mobility and enhance overall quality of life. Seeking professional guidance will provide clarity on effective management strategies tailored to individual needs.
Diagnosis of De Quervain Syndrome
Diagnosing De Quervain Syndrome begins with a thorough physical examination. A healthcare provider will assess the patient’s medical history and observe for signs of pain or discomfort in the thumb and wrist area.
One key test used is the Finkelstein Test. During this maneuver, patients are asked to grasp their thumb and bend their wrist toward the little finger. If pain occurs on the side of the wrist, it indicates potential De Quervain’s Tenosynovitis.
Imaging studies like X-rays may be performed to rule out fractures or arthritis. Ultrasound can also help visualize swelling in tendons surrounding the affected areas.
A detailed differential diagnosis is crucial to distinguish De Quervain syndrome from other conditions that cause similar symptoms, such as carpal tunnel syndrome or arthritis. Accurate diagnosis ensures appropriate treatment strategies are implemented promptly.
Physical Examination Techniques
Physical examination techniques are vital for diagnosing De Quervain Syndrome. A healthcare provider will start with a thorough assessment of the patient’s medical history and symptoms.
Observation plays a key role, as swelling or visible deformities around the wrist and thumb can indicate inflammation. The clinician may then assess range of motion by asking the patient to move their thumb and wrist in various directions.
Palpation is another important technique where the doctor gently presses on specific areas near the base of the thumb. This helps identify pain points that correlate with De Quervain’s Tenosynovitis.
Additionally, functional tests might be performed to evaluate grip strength. These examinations provide comprehensive insights into how much discomfort is present during typical hand movements. Each step contributes to forming a complete picture necessary for accurate diagnosis and effective treatment planning.
Finkelstein Test for De Quervain Syndrome
The Finkelstein Test is a simple yet effective physical examination technique used to diagnose De Quervain Syndrome. It focuses on assessing pain associated with the tendons of the thumb.
To perform this test, patients are asked to make a fist while enclosing their thumb inside. Then, they gently tilt their wrist towards the little finger side. If this movement elicits sharp pain along the base of the thumb or in the wrist area, it suggests inflammation of the affected tendons.
This diagnostic method is quick and can be performed in a clinical setting without any special equipment. Although it’s not definitive on its own, positive results often lead healthcare providers to further evaluate for De Quervain’s Tenosynovitis.
The Finkelstein Test plays an essential role in guiding treatment options based on accurate diagnosis and patient symptoms.
Imaging Studies: X-rays and Ultrasound
Imaging studies play a crucial role in diagnosing De Quervain Syndrome. Both X-rays and ultrasound are commonly utilized techniques.
X-rays are typically the first step. They help rule out fractures or other bone-related issues that may mimic symptoms of De Quervain’s tenosynovitis. Although X-rays don’t directly show soft tissue problems, they provide essential context for the physician.
Ultrasound, on the other hand, offers a comprehensive view of the tendons and surrounding structures in real-time. This imaging technique can reveal inflammation or swelling around the affected tendons. It also allows for dynamic assessment, which means doctors can observe how these structures move with thumb and wrist motions.
Together, these imaging modalities enhance diagnostic accuracy, guiding treatment plans effectively while ensuring patients receive appropriate care based on their specific needs.
De Quervain Syndrome Differential Diagnosis
Differentiating De Quervain Syndrome from other conditions is essential for effective treatment. Several disorders can mimic its symptoms, making accurate diagnosis critical.
Carpal tunnel syndrome often presents with wrist pain and numbness in the fingers. However, it primarily affects the median nerve, not the tendons at the thumb’s base.
Intersection syndrome is another contender. It involves irritation where two tendon groups cross near the wrist but usually entails more localized swelling than De Quervain’s.
Osteoarthritis of the basal joint may also resemble this condition. Patients typically experience pain during pinch movements or gripping due to degenerative changes in cartilage at the thumb’s base.
Rheumatoid arthritis can cause similar discomfort but usually affects multiple joints symmetrically and involves systemic symptoms like fatigue or fever. A thorough clinical evaluation helps ensure an accurate diagnosis and appropriate management plan tailored to individual needs.
De Quervain Syndrome Conservative Treatment Options
Conservative treatment options for De Quervain Syndrome focus on alleviating pain and restoring function. Rest and activity modification are crucial. Reducing activities that exacerbate symptoms can significantly aid recovery.
Splinting or bracing the wrist provides support, limiting movement while allowing healing. A well-fitted splint keeps the thumb in a neutral position, reducing strain on affected tendons.
Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen help manage pain and inflammation effectively. These medications can be taken as needed to improve comfort levels.
Applying ice packs to the inflamed area offers immediate relief. Alternating between cold and heat therapy may further enhance recovery by stimulating circulation and easing tension in surrounding muscles. Regular therapeutic exercises tailored for gradual improvement can also play a vital role in rehabilitation without overexertion or additional strain on the joint structures involved.
Rest and Activity Modification
Rest is one of the most crucial steps in managing De Quervain Syndrome. Giving your thumb and wrist time to heal can significantly reduce inflammation and pain. It’s essential to listen to your body and avoid activities that exacerbate symptoms.
Activity modification plays a pivotal role as well. Identify repetitive motions or tasks causing discomfort, such as gripping, pinching, or lifting. Minimize these actions when possible.
Consider altering how you perform daily tasks. For example, using larger tools with ergonomic grips can lessen strain on the affected area. Adjusting your workspace setup might also help—keeping items within easy reach reduces unnecessary wrist movement.
Engaging in gentle movements instead of complete immobilization is beneficial too. Light stretching promotes blood flow without overexertion, aiding recovery while maintaining some functionality in the hand.
Splinting and Bracing
Splinting and bracing are effective methods for managing De Quervain Syndrome. These devices help immobilize the thumb and wrist, reducing strain on the affected tendons. By limiting movement, they allow the inflamed tissues to heal more effectively.
A well-fitted splint can provide significant relief from pain during everyday activities. It keeps the thumb in a neutral position, minimizing stress while performing tasks that require grip or pinch movements.
Braces can be beneficial for both daytime use and nighttime support. Nighttime braces prevent wrist flexion, which can exacerbate symptoms during sleep.
When choosing a splint or brace, consult with a healthcare professional to ensure proper fit and function. Regular adjustments may be necessary as healing progresses.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Non-Steroidal Anti-Inflammatory Drugs, commonly known as NSAIDs, play a crucial role in managing pain and inflammation associated with De Quervain Syndrome. These medications are widely available and can be easily obtained over-the-counter.
NSAIDs work by inhibiting enzymes that contribute to inflammation. This action helps reduce swelling around the affected tendons, ultimately alleviating discomfort. Common options include ibuprofen and naproxen.
While effective for short-term relief, it’s important to use these drugs judiciously. Prolonged use may lead to gastrointestinal issues or other side effects. Therefore, consulting with a healthcare provider before starting any medication is advisable.
Incorporating NSAIDs into a broader treatment strategy often enhances recovery outcomes for those suffering from De Quervain’s Tenosynovitis. Always follow recommended dosages and guidelines when using these medications for optimal results.
Ice and Heat Therapy for De Quervain’s Tenosynovitis
Ice and heat therapy can be effective for managing pain associated with De Quervain’s Tenosynovitis. Ice is often the first line of defense, especially during flare-ups. Applying an ice pack to the affected area helps reduce inflammation and numbs sharp pain.
For best results, use ice for 15-20 minutes several times a day. Remember to wrap the ice pack in a towel to protect your skin from frostbite.
On the other hand, heat therapy can help when stiffness sets in after initial swelling decreases. A warm compress or heating pad applied gently on the wrist may enhance blood flow and relax tense muscles.
Alternating between cold and heat treatments may also provide combined benefits. Listen to your body; some prefer one method over another based on individual comfort levels and responses to treatment strategies.
De Quervain Syndrome Medical Interventions
Corticosteroid injections are a common medical intervention for De Quervain Syndrome. These injections target the inflamed tendons, providing quick relief from pain and swelling. They can significantly improve mobility in affected individuals.
Ultrasound-guided injections enhance accuracy during this procedure. By using real-time imaging, healthcare providers can ensure that the medication is delivered precisely where it’s needed most, maximizing effectiveness.
Oral medications also play a role in managing symptoms. Non-steroidal anti-inflammatory drugs (NSAIDs) help alleviate discomfort and reduce inflammation when corticosteroids aren’t suitable or desired.
Each patient’s response to treatment varies. Therefore, it’s essential to work closely with healthcare professionals to tailor an approach that best suits individual needs and preferences while monitoring progress throughout the recovery process.
Corticosteroid Injections for De Quervain Syndrome
Corticosteroid injections are a common medical intervention for managing De Quervain Syndrome. These injections deliver potent anti-inflammatory medications directly into the affected area, providing relief from pain and swelling.
The corticosteroids work by reducing inflammation in the tendons surrounding the thumb and wrist. This targeted approach can lead to significant improvement in symptoms, often within a few days of administration.
Patients typically experience minimal discomfort during the injection process, although some may feel temporary soreness afterward. The effects can last weeks or even months, making it an attractive option for those seeking non-surgical solutions.
It’s essential to discuss potential side effects with your healthcare provider before opting for this treatment. Repeated injections may be necessary but should be carefully monitored to avoid complications such as tendon weakening or infection.
Ultrasound-Guided Injections
Ultrasound-guided injections are a minimally invasive procedure used to treat De Quervain Syndrome. This technique allows healthcare providers to visualize the affected area in real-time, ensuring accurate placement of medication.
During the procedure, ultrasound technology helps identify specific anatomical structures and guide the needle directly into the inflamed tendon sheath. This precision enhances the effectiveness of corticosteroid injections, reducing pain and inflammation associated with this condition.
Patients often experience quick relief from symptoms following an ultrasound-guided injection. The targeted approach minimizes damage to surrounding tissues, promoting faster recovery.
Additionally, this method can be performed in an outpatient setting without requiring general anesthesia. As a result, patients can return to daily activities shortly after treatment while enjoying improved thumb function and reduced discomfort.
Oral Medications of De Quervain’s Tenosynovitis
Oral medications are often a key component in managing De Quervain’s Tenosynovitis. Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen can help reduce pain and inflammation. These medications work by inhibiting enzymes that contribute to the inflammatory process.
For patients with more severe discomfort, doctors may prescribe stronger analgesics or corticosteroids in pill form. Corticosteroids provide significant relief from swelling and pain, allowing for better function during daily activities.
It’s essential to follow a healthcare provider’s guidance when using oral medications. Overuse can lead to side effects like gastrointestinal issues or cardiovascular risks.
Patients should also discuss their complete medical history before starting any medication regimen. This ensures personalized treatment tailored to individual health needs while minimizing potential complications associated with oral treatments for De Quervain’s syndrome.
Surgical Treatment for De Quervain Syndrome
For those who do not respond to conservative treatments, surgical intervention may be necessary. The primary goal is to relieve pressure on the affected tendons at the base of the thumb.
The most common procedure involves a surgical release technique. Surgeons make a small incision over the wrist and create space around the inflamed tendons. This helps restore mobility and alleviate pain.
Minimally invasive techniques have also gained popularity in recent years. These methods often result in less scarring and quicker recovery times. Patients can typically resume daily activities sooner than with traditional surgery.
Post-surgical rehabilitation plays a crucial role in recovery. Physical therapy focuses on restoring strength, range of motion, and function in the wrist and thumb area after surgery. Adhering to these rehabilitation protocols can significantly enhance overall outcomes for patients dealing with De Quervain Syndrome.
Surgical Release Procedure
The surgical release procedure for De Quervain Syndrome aims to alleviate pressure on the affected tendons. This is typically performed when conservative treatments fail to provide relief.
During surgery, an incision is made near the wrist, allowing access to the first dorsal compartment where the tendons are located. Surgeons carefully cut through the fibrous sheath surrounding these tendons. This creates more space for them to glide freely during movement.
Patients generally receive local anesthesia or sedation during this outpatient procedure. Recovery time varies but often includes a splint for support and limited motion initially.
After surgery, physical therapy may be recommended to restore strength and flexibility in the thumb and wrist. It’s important for patients to follow their healthcare provider’s guidelines closely for optimal outcomes following this intervention.
Minimally Invasive Techniques
Minimally invasive techniques for treating De Quervain Syndrome focus on reducing recovery time and minimizing tissue damage. These procedures involve smaller incisions, which leads to less postoperative pain and scarring.
One common approach is endoscopic surgery. This method utilizes a tiny camera inserted through small openings to guide the surgeon in releasing the affected tendons. It allows for precise movements while preserving surrounding tissues.
Another technique involves ultrasound-guided interventions that enhance accuracy during corticosteroid injections. Using real-time imaging, healthcare providers can deliver medication directly into the inflamed area, improving efficacy and comfort.
These methods not only expedite healing but also allow patients to return to their daily activities sooner than traditional surgical approaches would permit. As medical technology advances, these options become increasingly favorable for those suffering from De Quervain Syndrome.
Post-Surgical Rehabilitation
Post-surgical rehabilitation plays a critical role in recovery from De Quervain Syndrome surgery. After the procedure, it’s essential to follow a structured rehabilitation plan to regain strength and mobility.
Initially, gentle range-of-motion exercises are introduced. This helps maintain flexibility without straining the healing tissue. Gradually, patients can progress to strengthening exercises tailored for the wrist and thumb.
Physical therapy sessions often include modalities like ultrasound or electrical stimulation, which support healing and reduce pain. Manual therapy techniques may also be employed to enhance circulation and promote tissue repair.
Consistency is key during this phase. Regularly practicing prescribed exercises at home complements professional therapy sessions. Adhering to activity modifications ensures that patients do not overexert their recovering hand.
Engaging with an experienced therapist provides guidance on proper technique and adjustments based on individual needs. This collaborative approach fosters an effective pathway back to daily activities while minimizing complications.
Physical Therapy and Rehabilitation
Physical therapy plays a crucial role in the recovery from De Quervain Syndrome. Targeted exercises can help restore mobility and reduce pain.
Stretching exercises are especially beneficial. They promote flexibility in the wrist and thumb, aiding in healing. Gradual stretching helps maintain joint function without aggravating inflammation.
Strengthening programs focus on building muscle endurance around the affected area. A stronger support system allows for better hand function during daily activities.
Manual therapy techniques offer additional relief by improving circulation and reducing tension in surrounding muscles. These hands-on approaches facilitate quicker recovery times.
Ergonomic training is also vital for preventing recurrence. Patients learn to adopt proper postures and movements that minimize stress on their wrists while performing tasks at home or work.
Stretching Exercises for De Quervain’s Tenosynovitis
Stretching exercises play a vital role in managing De Quervain’s Tenosynovitis. They help improve flexibility and reduce tension around the affected tendons.
One effective stretch involves extending your arm in front of you with the palm facing up. Gently pull back on your fingers using the opposite hand, holding for 15 to 30 seconds. This targets both the wrist and thumb muscles, providing relief.
Another beneficial exercise is the thumb stretch. With your other fingers tucked into your palm, gently move your thumb away from your palm while keeping it straight. Hold this position for several seconds before releasing.
Perform these stretches daily, but always listen to your body. If you experience pain during any movement, stop immediately and consult a healthcare professional for guidance tailored to your needs. Regular stretching can significantly contribute to recovery and improved hand function over time.
Strengthening Programs
Strengthening programs focus on building the muscles surrounding the wrist and thumb. This supports recovery from De Quervain Syndrome while preventing future injuries.
Exercises often include resistance training using small weights or elastic bands. These help improve muscle endurance and stability in the forearm.
Another effective approach is targeted grip-strengthening exercises. Squeezing a stress ball or using hand grippers can enhance dexterity and overall strength.
Incorporating wrist curls into your routine can further fortify those essential muscles. Aim for controlled movements to avoid strain, ensuring safety throughout each exercise.
Consistency is key when following a strengthening program. Gradually increasing intensity will yield noticeable improvements over time, making daily activities easier and more comfortable.
Manual Therapy Techniques
Manual therapy techniques are hands-on approaches used by physical therapists to alleviate pain and improve function in patients with De Quervain Syndrome. These methods focus on manipulating the soft tissues surrounding the affected area.
One common technique involves mobilization of the thumb and wrist joints. This helps restore proper movement patterns, reducing stiffness and enhancing mobility.
Another approach is myofascial release, which targets tight fascia or connective tissue. By applying gentle pressure, therapists can help release tension and promote blood flow to the region.
Soft tissue massage is also beneficial for relieving muscle tightness around the tendons involved in De Quervain’s Tenosynovitis. Improved circulation from massage aids healing processes.
Incorporating these manual therapy techniques into rehabilitation can significantly enhance recovery outcomes and allow individuals to return to their daily activities more comfortably.
Ergonomic Training
Ergonomic training focuses on optimizing the workspace to reduce strain and enhance comfort. It emphasizes proper posture, equipment setup, and movement techniques during tasks.
Participants learn how to adjust their chairs, desks, and tools for maximum efficiency. Simple changes can prevent overuse injuries like De Quervain Syndrome.
Training often includes demonstrations of correct hand positioning while typing or using a mouse. This is crucial for reducing wrist stress.
Additionally, ergonomic training encourages regular breaks from repetitive activities. These pauses help alleviate tension in joints and muscles.
Employers may offer workshops or online resources to educate staff about ergonomic principles. Everyone benefits from an ergonomically designed environment that supports healthy habits at work and home.
Alternative and Complementary Therapies
Alternative and complementary therapies can play a significant role in managing De Quervain Syndrome. These approaches often focus on holistic healing, addressing both physical symptoms and emotional well-being.
Acupuncture is one popular method. By inserting thin needles at specific points, it aims to relieve pain and improve circulation around the affected area. Many patients report reduced discomfort after sessions.
Massage therapy is another effective option. Gentle manipulation of the muscles surrounding the wrist and thumb can alleviate tension, increase blood flow, and promote relaxation.
Kinesiology taping may also help support injured areas while allowing for greater movement flexibility. This technique uses adhesive tape that mimics skin elasticity to reduce strain during activities.
These therapies should complement traditional treatments rather than replace them. Always consult with healthcare professionals before starting any alternative methods to ensure safety and effectiveness tailored to your condition.
Acupuncture
Acupuncture is an ancient practice rooted in Traditional Chinese Medicine. It involves inserting thin needles into specific points on the body. This technique aims to balance energy flow, known as “Qi,” and promote healing.
For those suffering from De Quervain Syndrome, acupuncture can provide relief by reducing inflammation and improving circulation around the affected area. By targeting pain pathways, it may alleviate discomfort and enhance mobility.
Many patients report feeling relaxed during sessions, which can contribute to a decrease in stress-related tension. Acupuncturists often tailor treatments based on individual symptoms, making each experience unique.
As with any therapy, it’s essential to consult with a qualified practitioner who understands your specific condition. Combining acupuncture with other treatment modalities can create a comprehensive approach for managing De Quervain’s Tenosynovitis effectively.
Massage Therapy for De Quervain’s Tenosynovitis
Massage therapy can be an effective complementary treatment for De Quervain’s tenosynovitis. It focuses on relieving tightness in the muscles surrounding the thumb and wrist. By using various techniques, a skilled massage therapist can enhance blood circulation to the affected area.
Gentle strokes and kneading may help reduce inflammation and pain. This hands-on approach promotes relaxation, which is crucial when managing discomfort from overuse injuries. Additionally, massaging the forearm can alleviate tension that radiates down to the wrist.
Therapists often incorporate stretching into their sessions. These stretches target specific muscle groups, improving flexibility and range of motion. Patients might find that regular massage not only eases symptoms but also contributes to overall hand function.
Incorporating massage with other treatments like physical therapy or splinting offers a holistic approach to recovery from this condition. Each session should be tailored to individual needs for optimal results.
Kinesiology Taping
Kinesiology taping is a popular method used in rehabilitation, especially for conditions like De Quervain Syndrome. It involves the application of elastic tape to support and stabilize muscles and joints without restricting their range of motion.
The technique works by lifting the skin slightly, which can reduce pressure on pain receptors. This action may help alleviate discomfort associated with inflammation and overuse injuries.
When applied correctly, kinesiology tape can improve circulation around the affected area. Better blood flow contributes to healing and recovery while providing stability during movement.
Patients often find that kinesiology taping enhances proprioception—the body’s ability to sense movement, action, and location. By using this supportive measure alongside other treatments, individuals with De Quervain’s Tenosynovitis may enjoy improved function in daily activities.
De Quervain Syndrome Prevention Strategies
Preventing De Quervain Syndrome involves a proactive approach to daily activities and ergonomics. Start by assessing your workspace. Ensure that your desk, chair, and tools promote good posture.
When performing repetitive tasks, pay attention to technique. Use proper hand positioning to minimize strain on the thumb and wrist. Small adjustments can make a significant difference over time.
Incorporate regular breaks into your routine. Short pauses allow muscles to relax and recover from continuous motion. Stretching during these breaks can improve flexibility and reduce tension.
Strengthening exercises for the wrists and hands are also beneficial. Focus on building endurance in those muscle groups through targeted workouts.
Consider ergonomic training if you frequently engage in repetitive motions at work or home. This guidance can help you identify potential issues before they lead to pain or injury associated with De Quervain Syndrome.
Workplace Ergonomics
Workplace ergonomics refers to designing workspaces that promote comfort and efficiency. Proper ergonomic setups can significantly reduce the risk of developing musculoskeletal disorders, including De Quervain Syndrome.
Start by ensuring your workstation is set up correctly. Keep your monitor at eye level to prevent neck strain. Your chair should support your lower back while allowing feet to rest flat on the floor.
Adjusting tools and devices is equally important. Use a keyboard and mouse that fit comfortably in hand, minimizing excessive wrist movements. Consider using an ergonomic thumb grip for frequently used tools.
Regular breaks are essential as well. Stand up, stretch, or reposition yourself every hour to relieve tension in muscles and joints. These simple changes can enhance productivity while safeguarding against potential injuries related to repetitive tasks.
Proper Technique for Repetitive Tasks
Using proper technique during repetitive tasks is essential for preventing De Quervain Syndrome. Simple adjustments can make a significant difference.
First, maintain a neutral wrist position. Avoid bending your wrist excessively while performing activities like typing or using handheld devices. This reduces strain on the tendons.
Second, ensure that your hands are relaxed. Tension can exacerbate symptoms and lead to injury over time. Take breaks to shake out any stiffness in your fingers and wrists.
Third, use tools designed for comfort and efficiency. Ergonomic grips on utensils or tools can minimize stress on your joints.
Alternate tasks whenever possible. Switching between different motions helps distribute stress evenly across various muscle groups and tendons, giving specific areas a chance to recover from fatigue.
Strengthening and Flexibility Exercises
Strengthening and flexibility exercises play a crucial role in managing De Quervain Syndrome. These targeted movements help alleviate pain and promote recovery.
To enhance strength, focus on wrist curls with light weights. This exercise builds the muscles around the wrist, providing better support for thumb movements. Another effective option is to perform grip squeezes using a soft stress ball. This promotes both endurance and strength in your hand.
Flexibility is equally important. Gentle stretches like thumb extensions can improve range of motion without exacerbating discomfort. Try holding your fingers back gently while keeping your palm flat on a table for added stretch.
Incorporating these exercises into your daily routine can aid recovery. Performing them consistently fosters resilience in affected areas, ultimately leading to improved functionality throughout daily activities.
Regular Breaks and Stretching
Taking regular breaks is essential for preventing De Quervain Syndrome, especially if your work involves repetitive hand motions. Short pauses throughout your day allow muscles and tendons to recover from strain.
During these breaks, focus on gentle stretching exercises. Simple thumb stretches can help alleviate tension in the affected area. Extend your fingers wide, hold for a few seconds, then relax. This promotes flexibility and circulation.
Incorporating wrist rotations can also be beneficial. Move your wrist in circular motions several times to relieve stiffness and promote mobility.
Setting reminders on your phone or computer can ensure you take these necessary pauses consistently. Just a few minutes of rest every hour can make a significant difference in reducing the risk of developing or worsening symptoms associated with De Quervain Syndrome. Prioritizing breaks will not only protect your hands but also enhance overall productivity throughout the day.
De Quervain’s Tenosynovitis Complications and Long-term Effects
Living with De Quervain Syndrome can lead to complications if not addressed properly. Chronic pain syndrome is one of the most significant concerns. Persistent discomfort may hinder daily activities and affect overall quality of life.
Many individuals find their ability to perform routine tasks diminished, impacting both personal and professional aspects. This struggle can cause frustration and limit engagement in hobbies or social interactions.
The psychological effects shouldn’t be overlooked either. Ongoing pain and mobility issues can lead to feelings of anxiety or depression. Patients may feel isolated due to their limitations, which further exacerbates mental health challenges.
Long-term exposure to untreated symptoms might even result in permanent dysfunction within the wrist or thumb area. Seeking timely intervention becomes crucial for maintaining functionality and well-being as a person navigates through this condition’s challenges.
Chronic Pain Syndrome
Chronic Pain Syndrome can emerge from conditions like De Quervain Syndrome, where pain lingers beyond the expected healing time. This persistent discomfort often affects daily life and mental health.
Patients may experience heightened sensitivity to pain stimuli, leading to a cycle of distress. The ongoing nature of chronic pain can cause fatigue, sleep disturbances, and emotional challenges such as anxiety or depression.
Treatment approaches for Chronic Pain Syndrome typically involve multidisciplinary strategies. These might include physical therapy, cognitive behavioral therapy, and medication management tailored to individual needs.
Addressing both the physical and psychological aspects is vital in managing this complex condition. Educating patients about their symptoms empowers them to seek help early and advocate for effective treatment options.
Impact on Daily Activities and Work
De Quervain Syndrome can significantly disrupt daily routines. Simple tasks, such as gripping a pen or turning a doorknob, may become painful and challenging. This limitation often leads to frustration and decreased productivity.
At work, the impact is even more pronounced. Jobs that require repetitive wrist movements or fine motor skills can exacerbate symptoms. Employees might find themselves taking frequent breaks to manage discomfort.
Social interactions can also be affected. Hobbies like knitting or playing sports may become difficult, leading to feelings of isolation or sadness.
Adjustments in the workplace are crucial for those suffering from this condition. Employers who understand these challenges can implement ergonomic solutions and promote an accommodating environment for their employees’ well-being.
De Quervain Syndrome Psychological Effects
De Quervain Syndrome can significantly impact a person’s mental well-being. Chronic pain often leads to frustration and anxiety, affecting daily life and activities.
The inability to perform routine tasks can foster feelings of helplessness. Individuals may find themselves withdrawing from social interactions due to discomfort or embarrassment about their condition.
Stress levels may increase as people worry about work performance or the ability to care for family members. This added pressure can result in sleep disturbances, further compounding psychological distress.
Additionally, those with De Quervain’s Tenosynovitis might develop negative thought patterns about their health and capabilities. Seeking support from healthcare professionals or joining support groups can be beneficial in managing these emotional challenges. Acknowledging both physical and mental aspects of this syndrome is essential for comprehensive treatment and recovery.
Living with De Quervain Syndrome
Living with De Quervain Syndrome can present daily challenges, but there are ways to adapt. Many individuals find that modifying their routines helps ease discomfort. Simple changes in how you hold objects or perform tasks can make a significant difference.
Adaptive techniques for daily activities include using your whole hand rather than just your thumb. This reduces strain on affected tendons and minimizes pain during gripping motions.
Assistive devices like ergonomic tools or specialized grips can provide support when performing repetitive tasks. They help distribute pressure more evenly, making it easier to manage everyday responsibilities.
Pain management strategies are essential as well. Regularly applying ice packs may reduce swelling and relieve discomfort after an intensive activity. Experimenting with heat therapy can also soothe tight muscles around the wrist and thumb area, promoting better mobility throughout the day.
Adaptive Techniques for Daily Tasks
Living with De Quervain Syndrome can make everyday tasks challenging. However, there are adaptive techniques that can simplify your routine.
For cooking, use tools with ergonomic handles. This reduces strain on your thumb and wrist. Consider using lightweight pots and pans as well to ease the burden.
When typing or texting, utilize voice recognition software. It allows you to communicate without straining your hands. Alternatively, try a larger keyboard or smartphone for improved accessibility.
In addition to these adaptations, consider using assistive devices like jar openers or reachers. These gadgets help minimize the need for grip strength during daily chores.
Practice mindful movements throughout the day. Slow down and be conscious of how you position your hands while performing tasks to avoid exacerbating pain in affected areas.
Assistive Devices and Tools
Assistive devices and tools can significantly enhance daily living for those with De Quervain Syndrome. These specially designed items help reduce strain on the thumb and wrist, making tasks easier to perform.
Grip aids are particularly beneficial. They provide support during activities like opening jars or holding utensils. Tools with ergonomic designs encourage a more comfortable hand position, which is crucial for minimizing pain.
Adaptive kitchen gadgets, such as jar openers or easy-grip peelers, allow individuals to maintain their independence while reducing discomfort. Similarly, writing aids can simplify note-taking without exacerbating symptoms.
Splints are another important resource. Wearing a splint supports the thumb and wrist during physical activity or rest periods. This added stability helps prevent further irritation of the tendons involved in De Quervain Syndrome.
Finding the right assistive devices tailored to individual needs can make a significant difference in managing daily challenges effectively.
Pain Management Strategies
Living with De Quervain’s tenosynovitis can be challenging, but effective pain management strategies are available to help you regain control over your daily activities. Understanding how to manage discomfort is essential for improving your quality of life.
One key approach involves using appropriate medications. Non-steroidal anti-inflammatory drugs (NSAIDs) can provide significant relief from pain and inflammation associated with this condition. However, it’s important to consult a healthcare provider before starting any new medication regimen.
In addition to pharmacological options, incorporating physical therapy into your routine can greatly aid in managing symptoms. A qualified therapist will design exercises tailored specifically for you, focusing on stretching and strengthening the muscles around the thumb and wrist. This personalized program plays a critical role in restoring function while alleviating pain.
Mindfulness techniques also prove beneficial for many individuals experiencing chronic pain related to De Quervain Syndrome. Practices such as deep breathing exercises or meditation may help reduce stress levels, which often exacerbate feelings of discomfort.
Utilizing assistive devices like ergonomic tools or braces can further enhance comfort during daily tasks. These aids minimize strain on the affected area while promoting proper hand positioning—essential components when navigating life with De Quervain’s tenosynovitis.
Don’t underestimate the power of regular breaks and movement throughout the day! Implementing short pauses during repetitive activities allows your body time to recover and reduces overall fatigue in the wrist and thumb areas.
By combining these various approaches—medication, physical therapy, mindfulness practices, supportive devices, and scheduled rest periods—you take significant steps toward effectively managing pain linked with De Quervain Syndrome. Embracing these strategies empowers you not only physically but mentally too as you navigate through challenges posed by this condition.