Buschke-Ollendorff Syndrome: An Introduction
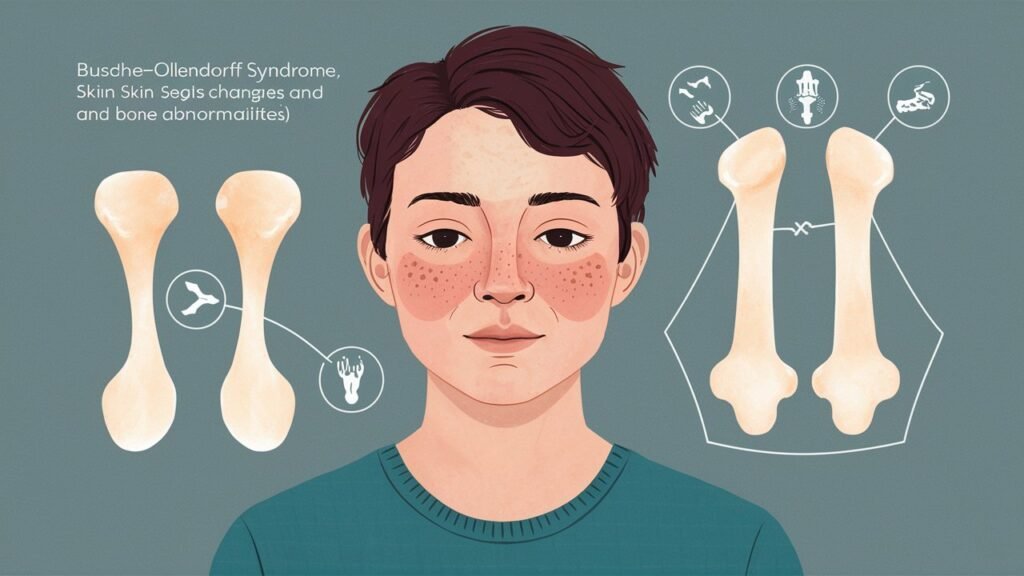
Buschke-Ollendorff Syndrome is a rare genetic condition that often flies under the radar. For those affected, it holds significant implications for their skin and bone health. Characterized by unique dermatological features and skeletal anomalies, this syndrome offers a fascinating glimpse into the intricacies of human genetics.
Patients with Buschke-Ollendorff Syndrome frequently experience connective tissue nevi—benign growths on the skin that can vary in appearance. Alongside these skin manifestations, individuals may also encounter osteopoikilosis, a condition marked by abnormal bone density patterns.
Understanding this syndrome not only sheds light on its clinical presentation but also highlights its impact on patients’ overall well-being. From diagnosis to management strategies, there’s much to explore about how Buschke-Ollendorff Syndrome shapes lives and what advancements are being made in research.
Whether you’re a medical professional seeking insights or someone personally touched by this condition, this comprehensive guide will delve deeply into every aspect of Buschke-Ollendorff Syndrome—from its genetic roots to orthopedic considerations and beyond.
Genetic Basis: LEMD3 Gene Mutations
Buschke-Ollendorff Syndrome is primarily linked to mutations in the LEMD3 gene. This gene plays a crucial role in maintaining the structural integrity of connective tissues.
LEMD3 encodes a protein that is essential for proper cellular function and development. Mutations disrupt this process, leading to abnormal skin and bone formations.
“Why Is It Called Baboon Syndrome? Understanding SDRIFE”
These genetic alterations can be inherited or occur sporadically. The variations often result in connective tissue nevi, which are benign growths on the skin.
Understanding these mutations provides insight into disease mechanisms. It also opens doors for targeted therapies and improved patient management strategies. Researchers continue to study LEMD3 to unravel its complexities further.
Inheritance Pattern and Family History
Buschke-Ollendorff Syndrome follows an autosomal dominant inheritance pattern. This means that a single copy of the mutated gene is enough to cause the disorder. If one parent carries the mutation, there is a 50% chance of passing it on to each child.
Family history plays a crucial role in understanding this syndrome. Individuals with affected relatives often have insights into their own risk. Genetic counseling can provide valuable information about potential implications for family members.
“What Is Banti’s Syndrome & How Does It Affect The Spleen?”
It’s not uncommon for symptoms to appear sporadically within families due to variable expressivity. In some cases, individuals may present mild signs while others experience more pronounced features.
Gathering detailed information about family medical history aids in early detection and management strategies for those at risk of developing Buschke-Ollendorff Syndrome.
Dermatological Manifestations: Connective Tissue Nevi
Connective tissue nevi are a hallmark of Buschke-Ollendorff Syndrome. These skin lesions appear as firm, raised nodules or plaques. They typically range in color from flesh-toned to brown.
These nevi often develop during childhood or adolescence. As individuals age, the lesions can increase in number and size, becoming more prominent on the skin surface. Their distribution can vary but is commonly observed on the trunk and limbs.
“How Does Barlow’s Syndrome Impact Heart Valve Function?”
The texture of these nevi may feel rubbery or thickened due to an excess production of collagen fibers within the dermis. This characteristic gives them a unique appearance that distinguishes them from other dermatological conditions.
It’s essential for patients with Buschke-Ollendorff Syndrome to monitor these skin changes regularly. Any sudden alterations in size, shape, or color should prompt further evaluation by a dermatologist for proper management and care options.
Skeletal Abnormalities: Osteopoikilosis
Osteopoikilosis is a skeletal abnormality commonly associated with Buschke-Ollendorff Syndrome. This condition is characterized by the presence of small, round bone lesions that can be found throughout the skeleton.
These lesions are typically benign and often remain asymptomatic. However, their discovery during imaging studies can raise concerns for patients and healthcare providers alike.
“What Causes Beckwith-Wiedemann Syndrome in Infants?”
Affected individuals may experience varying degrees of skeletal changes, which could lead to increased fragility in certain bones. Although fractures do not usually occur due to osteopoikilosis alone, awareness of this condition is vital when assessing overall bone health.
Radiographic evaluations reveal distinctive patterns that help differentiate osteopoikilosis from other similar conditions. Early detection through imaging techniques allows for better management strategies and monitoring over time. Understanding these abnormalities contributes to a clearer picture of the implications for those with Buschke-Ollendorff Syndrome.
Age of Onset and Disease Progression
Buschke-Ollendorff Syndrome typically manifests during childhood or early adolescence. The age of onset can vary, with some individuals noticing symptoms in infancy while others exhibit them later.
“Why Does Benedikt Syndrome Affect Eye Movement? Complete Guide”
As the condition progresses, skin lesions become more pronounced. Connective tissue nevi often appear as firm, dome-shaped nodules on the trunk and limbs. These growths may multiply over time, leading to a greater cosmetic impact.
Skeletal abnormalities like osteopoikilosis are usually identified around the same time as dermatological symptoms. Bone changes tend to remain stable throughout life but require monitoring for any potential complications.
Individuals with this syndrome generally do not experience severe health issues related to their skin or bones. However, regular check-ups are essential for tracking disease progression and managing any emerging concerns effectively.
Diagnostic Criteria and Clinical Evaluation
Diagnosing Buschke-Ollendorff Syndrome requires a comprehensive clinical evaluation. The primary focus is on identifying characteristic skin lesions and skeletal abnormalities.
“What Is Birt-Hogg-Dubé Syndrome? Cancer Risk & Management”
Healthcare professionals typically assess for specific dermatological manifestations, such as connective tissue nevi. These lesions often appear as firm, raised bumps that may vary in color. Their distribution across the body can provide clues to the diagnosis.
Radiological assessments play a vital role too. X-rays help reveal osteopoikilosis, which presents as small bone densities throughout the skeleton.
Family history is another critical aspect of the evaluation process. Gathering detailed information about relatives’ health can shed light on potential genetic patterns associated with this syndrome.
A multidisciplinary approach involving dermatologists and radiologists enhances diagnostic accuracy. This collaborative effort ensures that all aspects of the patient’s condition are addressed effectively during assessment.
Radiographic Findings in Buschke-Ollendorff Syndrome
Radiographic findings play a crucial role in identifying Buschke-Ollendorff Syndrome. Key features typically include osteopoikilosis, characterized by multiple bone lesions. These appear as small, round sclerotic areas on X-rays.
The most commonly affected bones are the pelvis and long bones. This pattern of bone involvement can aid healthcare providers in making an accurate diagnosis.
In some cases, additional imaging studies like CT scans or MRIs may reveal more details about these skeletal anomalies. However, the classic radiological signs often suffice for initial assessments.
It’s important to remember that while these findings are indicative of the syndrome, they don’t solely confirm it. A comprehensive evaluation incorporating clinical features is essential for a definitive diagnosis.
Differential Diagnosis and Similar Conditions
Differential diagnosis for Buschke-Ollendorff Syndrome often includes conditions that present with similar skin and bone features. One notable condition is Fibrous Dysplasia, characterized by abnormal growth of fibrous tissue in bones.
Another consideration is Nevoid Basal Cell Carcinoma Syndrome, which can lead to various skin lesions and skeletal abnormalities. While it shares some manifestations with Buschke-Ollendorff Syndrome, the genetic basis differs significantly.
Scleroderma may also be a potential misdiagnosis due to its connective tissue involvement. Patients might exhibit overlapping symptoms but lack the specific dermatofibrosis lenticularis disseminata observed in this syndrome.
Osteogenesis Imperfecta can mimic some skeletal features but does not involve the same cutaneous changes. Accurate identification of these conditions requires careful clinical evaluation and patient history analysis.
Skin Biopsy and Histopathological Features
A skin biopsy is a vital tool for diagnosing Buschke-Ollendorff Syndrome. This procedure involves removing a small section of the affected skin for examination.
Histopathological analysis reveals specific features that are characteristic of this syndrome. The presence of dermal connective tissue nevi, marked by dense collagen bundles and spindle-shaped fibroblasts, is often observed.
Additionally, there may be an increased number of vessels within the lesions. These findings help differentiate it from other dermatological conditions.
The biopsy results provide crucial insights into disease progression and guide management options. They also assist in understanding the underlying genetic aspects more clearly.
Timely biopsies can significantly enhance patient care by ensuring accurate diagnoses and tailored treatment plans based on individual histopathology profiles.
Genetic Testing and Counseling
Genetic testing plays a crucial role in diagnosing Buschke-Ollendorff Syndrome. Individuals suspected of having the condition can benefit from analyzing mutations in the LEMD3 gene. This test helps confirm whether genetic factors are at play.
Counseling is equally important for families affected by this syndrome. It provides insight into inheritance patterns and potential risks for future generations. Healthcare professionals guide parents through understanding how the disorder may manifest within their family.
Additionally, counseling prepares families emotionally and practically for managing associated challenges. Knowledge about possible outcomes can significantly ease anxiety surrounding the diagnosis.
With advancements in genetics, more options become available for those navigating this journey. Genetic counselors can also offer resources tailored to specific needs, helping families make informed decisions regarding health management and planning.
Management of Cutaneous Lesions
Management of cutaneous lesions in Buschke-Ollendorff Syndrome focuses primarily on the cosmetic and functional aspects. Many patients seek treatment for the appearance of connective tissue nevi, which can be unsightly or cause discomfort.
Topical therapies may help reduce irritation or inflammation associated with these lesions. However, surgical excision remains a common approach for individuals who experience significant psychosocial distress or substantial physical symptoms.
Laser therapy has also gained popularity. It offers a minimally invasive option to improve skin texture and color without extensive recovery time.
Regular dermatological evaluations are important to monitor any changes in existing lesions. This proactive approach aids in identifying potential complications early on. Education about proper skincare routines is equally crucial, as it helps manage symptoms effectively while fostering self-esteem among those affected by this condition.
Orthopedic Considerations and Bone Health
Individuals with Buschke-Ollendorff Syndrome often face unique orthopedic challenges. The presence of osteopoikilosis can lead to varying degrees of bone density abnormalities. Understanding these issues is crucial for proactive management.
Regular monitoring through imaging studies helps assess skeletal health. Physicians may recommend periodic X-rays to track any changes in bone structure or density over time.
Physical activity plays a vital role in maintaining strong bones. Weight-bearing exercises are generally encouraged, but patients should consult healthcare providers to tailor routines that avoid excessive strain.
In some cases, orthopedic interventions might be necessary. These could include physical therapy or surgical options to address specific deformities or pain.
Maintaining optimal calcium and vitamin D levels is essential for bone health. Nutritional guidance can aid in preventing complications associated with low-density bones.
Associated Systemic Manifestations
Buschke-Ollendorff Syndrome is primarily known for its dermatological and skeletal features. However, it can also present with systemic manifestations that may complicate the clinical picture.
Some individuals experience vascular issues such as venous malformations or lymphatic anomalies. These conditions could lead to edema or other circulatory problems in affected areas.
Gastrointestinal involvement has been observed in rare cases. Patients may report symptoms like abdominal pain or bowel irregularities, suggesting a need for careful monitoring of digestive health.
Additionally, some patients show an increased risk for certain tumors, particularly soft tissue sarcomas. This association underscores the importance of regular check-ups and screenings throughout life.
Understanding these systemic aspects allows for better management strategies tailored to individual needs and enhances overall patient care. Early identification of any associated complications can significantly improve quality of life.
Impact on Growth and Development
Buschke-Ollendorff Syndrome can significantly influence growth and development in affected individuals. The presence of connective tissue nevi, which are benign skin lesions, may cause psychosocial challenges during childhood and adolescence.
These skin manifestations can affect self-esteem and body image, leading to social withdrawal or anxiety. As children navigate these emotional hurdles, their overall development might be impacted.
Skeletal abnormalities like osteopoikilosis can also pose physical constraints. These bone changes may lead to discomfort or mobility issues that hinder participation in sports and other activities crucial for healthy growth.
Additionally, surveillance for potential complications related to the skeletal system is essential. Early intervention strategies focusing on physical therapy can help enhance mobility and encourage active lifestyles among those with Buschke-Ollendorff Syndrome. This supportive approach fosters a more positive developmental trajectory despite the challenges posed by the condition.
Psychological Aspects and Body Image
Living with Buschke-Ollendorff Syndrome can impact more than just physical health. The visible skin lesions associated with the condition, known as connective tissue nevi, may lead to concerns about body image.
Individuals often face challenges in social situations due to their appearance. This can result in feelings of self-consciousness and anxiety. Negative perceptions from others may exacerbate these emotions, leading to isolation.
Support systems play a crucial role in addressing these psychological aspects. Open conversations with family and friends help foster understanding and acceptance. Counseling or therapy might also be beneficial for those struggling with self-esteem issues related to their condition.
Promoting awareness about Buschke-Ollendorff Syndrome is essential for reducing stigma. Educational resources can empower individuals living with this syndrome, encouraging them to embrace their uniqueness rather than hide it away.
Long-term Prognosis and Life Expectancy
Long-term prognosis for individuals with Buschke-Ollendorff Syndrome varies, primarily influenced by the severity of dermatological and skeletal manifestations. Most patients experience slow disease progression, allowing for a relatively normal life expectancy.
The condition is often benign in nature. Many affected individuals lead fulfilling lives without significant complications. However, regular monitoring is crucial to address any potential orthopedic issues or skin-related concerns that may arise over time.
Early intervention can make a substantial difference in managing symptoms effectively. Collaboration between dermatologists, orthopedists, and genetic counselors ensures comprehensive care tailored to each patient’s needs.
Emotional support also plays a vital role as individuals navigate their unique challenges related to body image and self-esteem. With appropriate management strategies in place, many people live active and healthy lives despite this rare genetic disorder.
Pregnancy and Genetic Counseling for Carriers
Pregnancy can present unique challenges for individuals carrying the genetic mutation associated with Buschke-Ollendorff Syndrome. It’s crucial to understand these implications early on.
Genetic counseling plays a vital role in this context. Professionals can provide insights into inheritance patterns and potential risks for offspring. They help prospective parents navigate their options and make informed decisions.
Testing for the LEMD3 gene mutation is available and can offer clarity about the likelihood of passing on the condition. This information allows families to prepare for various outcomes, both physically and emotionally.
Expectant mothers should also consider regular monitoring during pregnancy. Healthcare providers may recommend additional screenings or interventions tailored to individual risk factors related to bone health or dermatological manifestations.
Open communication with medical professionals ensures that all aspects of care are addressed throughout pregnancy, promoting overall well-being for both parent and child.
Current Research and Clinical Studies
Current research and clinical studies are shedding light on Buschke-Ollendorff Syndrome, exploring new avenues for understanding its complexities. These investigations aim to clarify the genetic mechanisms behind LEMD3 gene mutations and their role in symptom development.
Researchers are also focused on identifying potential biomarkers that could aid in the early diagnosis of this syndrome. By studying patient samples and analyzing genetic profiles, scientists hope to develop more effective screening tools.
Clinical trials are underway to test innovative treatment options for managing skin lesions associated with dermatofibrosis lenticularis disseminata. The goal is to improve both the cosmetic outcomes and overall quality of life for those affected.
Additionally, multidisciplinary approaches combining dermatology, genetics, orthopedics, and psychology have gained traction. This holistic view acknowledges that the impact of Buschke-Ollendorff Syndrome extends beyond physical manifestations.
As researchers continue their work, there is optimism about finding comprehensive care strategies that address not only medical needs but also emotional support. This evolving landscape highlights a commitment within the medical community to enhance understanding and management of this rare condition.


