Shapiro Syndrome is a rare and intriguing disorder that captivates both medical professionals and patients alike. Characterized by periodic hypothermia, this condition unfolds like a complex puzzle, presenting unique challenges for those affected. For many, it raises questions about the mechanisms behind sudden temperature drops and how to manage them effectively.
Imagine experiencing episodes where your body temperature unexpectedly plummets, leaving you shivering despite warm surroundings. This phenomenon can be alarming and confusing, prompting individuals to seek answers about their health. As research continues to shed light on Shapiro Syndrome, understanding its symptoms, causes and treatment options becomes increasingly important.
Join us as we delve into the intricate world of Shapiro Syndrome — from its historical roots to modern-day implications. Whether you’re seeking knowledge for yourself or a loved one facing this disorder, this exploration aims to provide clarity and insight into living with periodic hypothermia.
Shapiro Syndrome Unveiled: Definition and Historical Background
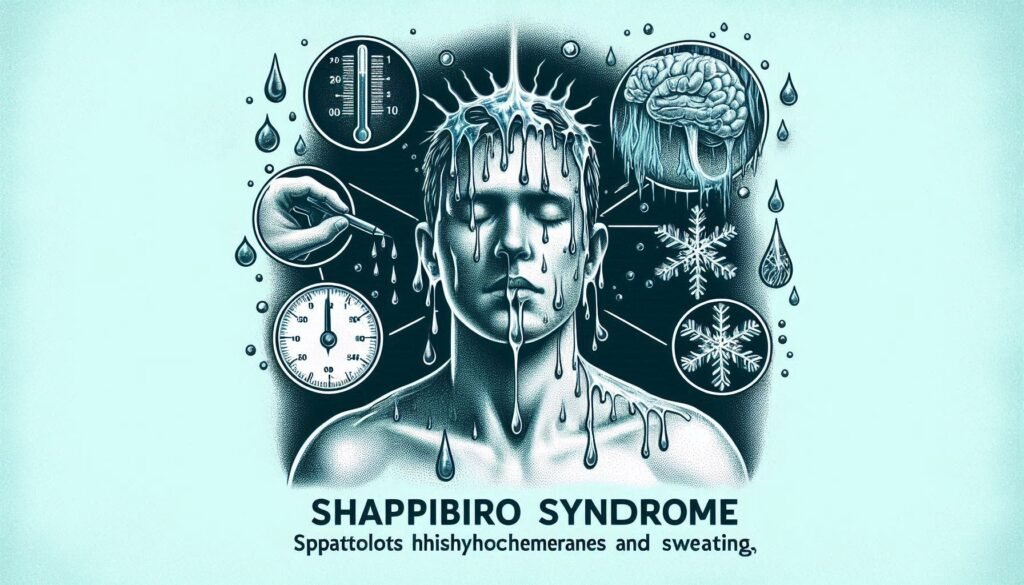
Shapiro Syndrome is a rare neurological disorder characterized by recurrent episodes of hypothermia, hyperhidrosis, and autonomic dysregulation. Patients experience sudden drops in body temperature, often accompanied by excessive sweating. This unique combination sets it apart from other medical conditions.
“Why Does Chronic Fatigue Syndrome Cause Persistent Tiredness?”
The syndrome was first described in 1965 by Dr. David Shapiro, who identified this perplexing behavior in patients presenting similar symptoms. Over the years, interest has grown among researchers and clinicians as they sought to understand its underlying mechanisms.
Though still not fully understood, Shapiro Syndrome highlights the complexity of human physiology and the brain’s role in regulating body temperature. As awareness increases, so does the potential for better diagnosis and management strategies for those affected by this enigmatic condition.
The Triphasic Nature of Shapiro Syndrome: Understanding Its Core Symptoms
Shapiro Syndrome is characterized by a distinctive triphasic pattern of symptoms. These phases include episodes of hypothermia, hyperhidrosis, and an intermediate state where the individual feels normal.
During hypothermic episodes, patients may experience a sudden drop in body temperature, leading to chills and discomfort. This phase can last from hours to days and often leaves individuals fatigued.
“What Triggers Cushing’s Syndrome? Complete Hormone Guide”
In contrast, the hyperhidrosis phase brings excessive sweating that can be both uncomfortable and socially challenging. Patients may find themselves drenched without any apparent trigger.
The transition between these states can happen unpredictably, complicating daily life for those affected. Each phase presents unique challenges affecting not only physical health but emotional well-being as well. Understanding this triphasic nature is essential for effective management and support for individuals with Shapiro Syndrome.
Etiology of Shapiro Syndrome: Exploring Potential Causes and Triggers
The etiology of Shapiro Syndrome remains an intriguing area of study, as it is classified as a rare neurological disorder. While exact causes are still being investigated, several potential triggers have been identified.
Genetic factors may play a role in the development of this condition. Some research suggests that mutations affecting the hypothalamus could contribute to its characteristic symptoms.
“How Does Carpal Tunnel Syndrome Develop? Prevention Tips”
Environmental influences might also be significant. For instance, exposure to extreme temperatures or infections has been noted in some cases leading up to episodes of hypothermia and hyperhidrosis.
Additionally, hormonal imbalances may exacerbate the syndrome’s manifestation. Fluctuations in hormones related to temperature regulation can trigger severe reactions for those affected by Shapiro Syndrome.
Understanding these contributing elements is crucial for developing effective management strategies and improving patient outcomes. Ongoing research continues to shed light on this complex disorder’s origins and mechanisms.
Neurological Basis: The Role of Hypothalamus in Shapiro Syndrome
The hypothalamus plays a crucial role in regulating body temperature and maintaining homeostasis. In Shapiro Syndrome, this small yet significant brain region is often implicated in the dysfunction that leads to periodic hypothermia.
Research suggests that abnormalities within the hypothalamus disrupt its normal functions. This can result in an impaired thermoregulatory response, causing patients to experience episodes of excessive coldness followed by hyperhidrosis or profuse sweating.
“What Makes Cauda Equina Syndrome a Medical Emergency?”
Dysregulation may also affect other autonomic processes governed by the hypothalamus, such as heart rate and blood pressure. Consequently, understanding these neurological underpinnings offers insight into why Shapiro Syndrome manifests the way it does.
Ongoing studies continue to explore the intricate connections between hypothalamic function and symptomatology in affected individuals. As researchers delve deeper into this relationship, they aim to uncover potential therapeutic targets for more effective management strategies.
Clinical Presentation: Recognizing the Signs and Symptoms
Shapiro Syndrome is characterized by a unique set of symptoms that can sometimes be challenging to identify. The hallmark feature is periodic hypothermia, where patients experience episodes of abnormally low body temperature. These events may occur unexpectedly and vary in duration.
“Why Does CHARGE Syndrome Affect Multiple Body Systems?”
Alongside the hypothermic episodes, individuals also report hyperhidrosis—excessive sweating during or after these spells. This combination can lead to significant discomfort and distress.
Patients might also experience alterations in their level of consciousness during episodes, which can range from confusion to complete unresponsiveness. Other neurological signs may include muscle rigidity and tremors.
It’s essential for healthcare providers to recognize this triphasic response: hypothermia, hyperhidrosis, and neurological changes. Early recognition helps in managing the syndrome effectively while improving patient quality of life.
Diagnostic Challenges: The Journey to Identifying Shapiro Syndrome
Identifying Shapiro Syndrome can be a daunting task. The rarity of the condition often leads to misdiagnosis or delayed diagnosis, as many physicians may not be familiar with its symptoms.
The triphasic nature of the syndrome complicates matters further. Patients experience alternating phases of hypothermia and hyperhidrosis, which can easily mimic other conditions like thyroid disorders or autonomic dysfunctions.
Diagnostic tests often yield inconclusive results. Conventional assessments may overlook the neurological underpinnings crucial for an accurate diagnosis. This underscores the need for specialized expertise in understanding this rare disorder.
In many cases, patients undergo a series of evaluations before receiving a confirmed diagnosis. This journey can be frustrating and disheartening, highlighting the importance of awareness among healthcare providers about Shapiro Syndrome’s existence and characteristics.
Imaging Studies: MRI and Other Neurological Investigations
Imaging studies play a crucial role in diagnosing Shapiro Syndrome. Magnetic Resonance Imaging (MRI) is often the preferred method for visualizing brain structures.
An MRI can reveal abnormalities in the hypothalamus, which may be linked to this rare disorder. Specific patterns or lesions often provide insight into underlying neurological issues associated with periodic hypothermia.
Other imaging techniques, such as CT scans and PET scans, can also contribute valuable information. These methods help rule out other conditions that might mimic Shapiro Syndrome symptoms.
Additionally, functional neuroimaging can assess how different parts of the brain interact during episodes of temperature dysregulation. This level of detail aids clinicians in understanding each patient’s unique presentation of the syndrome.
Comprehensive imaging forms a cornerstone in both diagnosis and treatment planning for individuals affected by Shapiro Syndrome.
Differential Diagnosis: Distinguishing Shapiro Syndrome from Similar Conditions
Differentiating Shapiro Syndrome from other disorders can be challenging due to overlapping symptoms. Conditions like hypothalamic dysfunction, autonomic dysregulation, and certain neurological disorders may present with similar signs.
Hypothalamic dysfunction often leads to temperature regulation issues but usually involves additional endocrine abnormalities. This makes it distinct from the periodic hypothermia seen in Shapiro Syndrome.
Autonomic dysregulation is another contender. Patients might experience episodes of sweating or temperature fluctuation but lack the characteristic triphasic pattern that defines Shapiro’s condition.
Moreover, conditions such as familial cold autoinflammatory syndrome also mimic features of Shapiro Syndrome. However, they do not exhibit the same neurological implications or specific symptom cycles.
Thorough clinical evaluation and a comprehensive patient history are crucial for arriving at an accurate diagnosis. Identifying these distinctions ensures patients receive appropriate treatment tailored to their unique health needs.
Treatment Approaches: Managing Symptoms of Shapiro Syndrome
Managing symptoms of Shapiro Syndrome requires a multifaceted approach. Since the disorder presents with periodic hypothermia and hyperhidrosis, patients often benefit from tailored treatment strategies.
Medications can play a crucial role. Antipyretics may help mitigate fever-like episodes, while beta-blockers might assist in managing excessive sweating. Each patient’s response to medication varies, necessitating careful monitoring and adjustments.
Non-pharmacological methods are equally important. Patients are encouraged to maintain an even temperature through appropriate clothing choices and environmental controls. Staying well-hydrated is vital during episodes of hypothermia or sweating.
Supportive therapies also contribute significantly to quality of life. Occupational therapy can help individuals adapt their daily activities, while counseling services provide emotional support for the challenges posed by this rare disorder.
Regular follow-ups with healthcare professionals ensure that management plans remain effective as symptoms evolve over time.
Pharmacological Interventions: Medications Used in Shapiro Syndrome
Pharmacological interventions for Shapiro Syndrome primarily aim to manage its core symptoms, particularly periodic hypothermia and hyperhidrosis.
Medications like beta-blockers may be prescribed to help alleviate excessive sweating. These can reduce the frequency and intensity of hyperhidrosis episodes.
On the other hand, antipyretics might be utilized in managing temperature regulation issues during hypothermic events. They assist in stabilizing body temperature when fluctuations occur.
Some clinicians may consider using selective serotonin reuptake inhibitors (SSRIs), as they have shown potential benefits in mood stabilization and anxiety reduction related to this condition.
It’s crucial for patients to work closely with their healthcare providers. Individual responses to medications can vary significantly, necessitating tailored treatment plans that address specific needs. Regular monitoring is essential for optimal results while minimizing side effects.
Non-Pharmacological Strategies: Lifestyle Modifications and Coping Techniques
Living with Shapiro Syndrome often requires more than just medication. Lifestyle modifications play a crucial role in managing symptoms effectively.
Adopting a balanced diet is vital. Foods rich in omega-3 fatty acids can help enhance overall well-being. Staying hydrated also supports body temperature regulation.
Regular exercise, tailored to individual capabilities, can improve circulation and strengthen the immune system. Gentle activities like yoga or swimming are beneficial without being overly strenuous.
Creating a comfortable environment helps minimize triggers for hypothermia or hyperhidrosis. Layering clothing allows individuals to adapt to sudden temperature changes easily.
Coping techniques such as mindfulness and relaxation exercises reduce stress levels, which may exacerbate symptoms. Support groups offer emotional assistance and valuable information from others facing similar challenges.
Incorporating these strategies fosters resilience and empowers individuals living with this rare disorder.
Prognosis and Long-term Outlook for Shapiro Syndrome Patients
The prognosis for Shapiro Syndrome varies among individuals. While some patients experience infrequent episodes of hypothermia and hyperhidrosis, others may contend with more severe symptoms that disrupt their daily lives.
Long-term outlook often depends on the effectiveness of management strategies. Early intervention can lead to better symptom control and improved quality of life. Many patients learn to recognize triggers, allowing them to adapt their lifestyles accordingly.
Regular follow-ups with healthcare providers are crucial for monitoring progression and adjusting treatment plans as necessary. Psychological support also plays a vital role in enhancing overall well-being.
Research into Shapiro Syndrome remains ongoing, offering hope for advancements in understanding this condition. With continued exploration, there is potential for new therapies that could further improve patient outcomes and experiences over time.
Quality of Life: Living with Periodic Hypothermia and Hyperhidrosis
Living with Shapiro Syndrome can significantly impact an individual’s quality of life. The unpredictable nature of periodic hypothermia and hyperhidrosis poses unique challenges.
Patients may experience sudden drops in body temperature, leading to discomfort and anxiety. These episodes often disrupt daily activities, making it difficult to maintain a routine.
On the other hand, excessive sweating can create social embarrassment and affect self-esteem. Individuals might find themselves avoiding certain situations or environments due to fear of an episode.
Support from friends, family, and healthcare professionals is crucial for managing these symptoms effectively. Emotional well-being plays a vital role in coping strategies.
Education about the condition empowers patients to advocate for their needs. Joining support groups provides a sense of community where experiences can be shared openly.
Finding ways to adapt lifestyle habits is essential for enhancing comfort levels during both hypothermic and hyperhidrosis episodes.
Pediatric Shapiro Syndrome: Special Considerations in Children
Pediatric Shapiro Syndrome presents unique challenges for young patients and their families. Children with this rare disorder often experience the same triphasic symptoms as adults, including episodes of hypothermia followed by hyperhidrosis.
Diagnosing Shapiro Syndrome in children can be particularly difficult. Symptoms may overlap with other conditions, leading to delays in proper treatment. Early recognition is essential to mitigate potential complications.
Management strategies should also be tailored for children. Parents and caregivers play a crucial role in monitoring symptoms and ensuring appropriate interventions are applied promptly.
Therapeutic approaches may include lifestyle modifications that help regulate temperature fluctuations while also addressing any psychological impacts related to living with such a rare condition.
Creating supportive environments both at home and school is vital, allowing affected children to engage fully without feeling overwhelmed or isolated due to their health condition.
Genetic Aspects: Current Understanding and Research Directions
Genetic research into Shapiro Syndrome is still in its infancy. However, some studies suggest a potential hereditary component. Researchers are investigating specific genes that may influence the disorder’s onset and severity.
Genome sequencing techniques have identified candidate genes associated with temperature regulation and autonomic functions. These findings could offer insights into the genetic basis of this rare condition.
Current studies also explore gene-environment interactions. Understanding how external factors may trigger symptoms can lead to more personalized treatment approaches.
Ongoing research aims to map out the full genetic landscape of Shapiro Syndrome. This includes examining family histories and conducting large-scale genomic analyses to identify common mutations or polymorphisms among affected individuals.
As knowledge expands, future directions may involve targeted therapies based on genetic profiles, paving the way for innovative management strategies tailored specifically for those diagnosed with Shapiro Syndrome.
Shapiro Syndrome and Autonomic Dysfunction: Exploring the Connection
Shapiro Syndrome is often intertwined with autonomic dysfunction. This connection reveals how the body’s regulatory systems can be affected by this rare disorder.
Patients frequently experience fluctuations in temperature regulation, a hallmark of Shapiro Syndrome. These episodes are not just limited to hypothermia but also involve sudden occurrences of hyperhidrosis. The body’s inability to maintain stable temperatures points to underlying autonomic nervous system disturbances.
The hypothalamus plays a pivotal role here, as it regulates various autonomic functions including temperature control and sweating response. When it’s compromised, patients may face unpredictable and uncomfortable symptoms.
Understanding this relationship helps healthcare providers develop better management strategies for individuals living with Shapiro Syndrome. Addressing autonomic dysfunction could lead to improved quality of life and symptom relief for those affected by the condition.
Psychological Impact: Mental Health Considerations for Patients
Living with Shapiro Syndrome can be an emotional roller coaster. The unpredictability of periodic hypothermia and hyperhidrosis creates unique stressors for patients.
Many individuals experience anxiety relating to their symptoms. Fear of sudden temperature drops in social situations can lead to avoidance behaviors, impacting relationships and daily life.
Moreover, the physical manifestations of the disorder may result in feelings of embarrassment or isolation. This makes mental health support crucial for those affected.
Therapies such as cognitive-behavioral therapy (CBT) have shown promise in helping patients develop coping strategies. Support groups also provide a sense of community, allowing individuals to share experiences and resources.
Addressing mental health is vital not only for well-being but also for managing overall health effectively. Integrating psychological care into treatment plans offers a holistic approach to living with Shapiro Syndrome.
Research Frontiers: Ongoing Studies and Future Prospects
Research into Shapiro Syndrome is gaining momentum, shedding light on this rare condition. Scientists are focusing on the neurological underpinnings that lead to periodic hypothermia and hyperhidrosis.
Current studies aim to unravel genetic markers associated with the syndrome. Understanding these could pave the way for targeted therapies in future treatment protocols.
Additionally, researchers are exploring how environmental factors may trigger episodes in susceptible individuals. This knowledge can help devise preventive strategies.
Clinical trials investigating new pharmacological interventions are also underway. These aim to improve patient outcomes by alleviating symptoms more effectively than existing medications.
Furthermore, interdisciplinary approaches combining neurology and psychology offer a promising avenue for comprehensive care. By addressing both physical and mental health aspects, patients might experience improved quality of life as research progresses.
Patient Experiences: Personal Stories and Case Studies
Patient experiences shed light on the real-life challenges faced by those living with Shapiro Syndrome. These stories often highlight a complex journey filled with both physical and emotional hurdles. Many individuals report feeling isolated due to their condition, as periodic hypothermia and hyperhidrosis can be difficult for others to understand.
One patient shared that initial symptoms were misattributed to stress or anxiety, which led to frustration in seeking appropriate care. For them, the turning point came when they found a specialist familiar with Shapiro Syndrome who could validate their experiences and guide them toward effective management strategies.
Another individual described how support groups became vital in coping with this rare disorder. Sharing personal anecdotes allowed them to connect with others facing similar battles, fostering a sense of community often lacking in day-to-day life.
Case studies illustrate varying symptom severity among patients, reinforcing the need for tailored treatment approaches. Some have successfully managed symptoms through lifestyle modifications like temperature regulation techniques or wearing moisture-wicking clothing.
These personal narratives emphasize resilience and adaptability despite the unpredictability of Shapiro Syndrome. They inspire hope and provide insights into navigating daily life while managing this rare disorder effectively. Understanding these lived experiences helps medical professionals better address patient needs, ultimately improving quality of life for those affected by Shapiro Syndrome.