Scheie Syndrome is a rare genetic disorder that falls under the umbrella of mucopolysaccharidosis (MPS) I. While it may be the mildest form within this group, its impact on those affected can still be significant. Understanding this condition not only sheds light on its symptoms and challenges but also emphasizes the importance of early diagnosis and effective management strategies.
As we delve into the nuances of Scheie Syndrome, we’ll explore its historical roots, genetic foundations, clinical features, and treatment options. This knowledge is vital for patients, families, and healthcare providers alike in navigating the complexities associated with this condition. Whether you are seeking information for yourself or a loved one, join us as we uncover essential insights about Scheie Syndrome that could make a difference in daily life.
What is Scheie Syndrome? An Overview of This Rare Genetic Disorder
Scheie Syndrome is a lysosomal storage disorder characterized by the body’s inability to break down specific complex carbohydrates known as glycosaminoglycans (GAGs). This accumulation disrupts various bodily functions, particularly affecting connective tissues and organs.
This condition is classified within mucopolysaccharidosis I, which encompasses three forms: Hurler, Hunter, and Scheie. The latter represents the mildest variant. Individuals with Scheie Syndrome typically experience fewer severe symptoms compared to those affected by its more severe counterparts.
“What Is Abdominal Compartment Syndrome & Why Is It Emergency?”
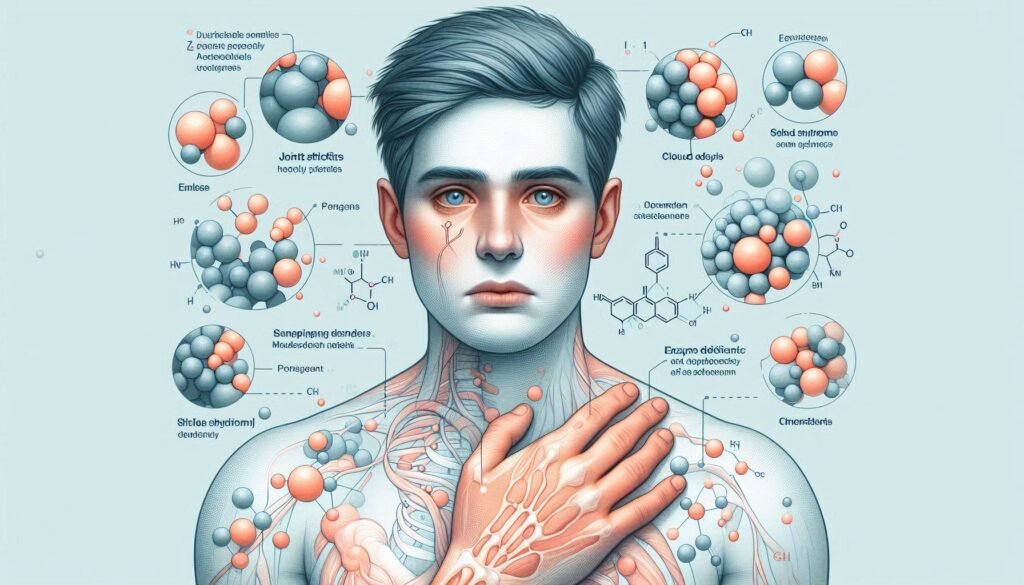
Symptoms can vary widely but often include joint stiffness, heart valve issues, and eye problems such as corneal clouding. Intellectual development usually remains unaffected, distinguishing it from other types of MPS disorders. Raising awareness about Scheie Syndrome promotes understanding and support for those living with this rare genetic condition.
Historical Background: Harold Scheie and the Discovery of the Syndrome
Harold Scheie was a prominent American ophthalmologist who made significant contributions to the understanding of genetic disorders. In the 1960s, he identified a previously unrecognized form of mucopolysaccharidosis I (MPS I). This condition would later be named Scheie Syndrome in his honor.
“Ablepharon Macrostomia Syndrome: What Causes These Facial Features?”
Scheie’s research focused on the clinical features that distinguished this milder variant from other forms of MPS I. His meticulous observations helped define key symptoms such as joint stiffness and corneal clouding. These findings were crucial for early diagnosis and management strategies.
His work laid the foundation for further studies into enzyme deficiencies related to MPS disorders. By linking specific genetic mutations to observable traits, Scheie paved the way for advancements in treatment options available today. His legacy continues to influence how we understand and manage Scheie Syndrome within the broader spectrum of mucopolysaccharidoses.
Genetic Basis: The Role of IDUA Gene Mutations
Scheie Syndrome is primarily caused by mutations in the IDUA gene. This gene encodes an enzyme called alpha-L-iduronidase, which plays a crucial role in breaking down glycosaminoglycans (GAGs) in the body.
“How Does Alström Syndrome Affect Multiple Organs? Complete Guide”
When mutations occur in the IDUA gene, this enzyme’s activity decreases significantly. As a result, GAGs accumulate within cells and tissues. The buildup of these complex sugars leads to various health issues associated with Scheie Syndrome.
Different types of mutations may lead to varying levels of enzyme deficiency. Some individuals may exhibit milder symptoms due to residual enzymatic function, while others could experience more pronounced effects from severe deficiencies.
Understanding these genetic underpinnings helps guide both diagnosis and treatment strategies for those affected by Scheie Syndrome. Genetic testing can reveal specific IDUA mutations, aiding families and healthcare providers in managing this rare condition effectively.
Biochemistry of Scheie Syndrome: GAG Accumulation and Its Effects
Scheie Syndrome results from the accumulation of glycosaminoglycans (GAGs) in various tissues. These complex carbohydrates play crucial roles in cellular functions and structural integrity.
“What Causes Angelman Syndrome? Understanding ‘Happy Puppet’ Disorder”
In individuals with Scheie Syndrome, defective enzyme activity leads to an inability to break down specific GAGs such as dermatan sulfate and heparan sulfate. This buildup occurs primarily within lysosomes, affecting multiple organ systems over time.
The excessive accumulation disrupts normal cellular processes. As a result, patients may experience stiffness in joints, corneal clouding, and heart valve issues. The severity of symptoms can vary widely among affected individuals despite similar genetic mutations.
Understanding the biochemistry behind GAG accumulation is essential for developing targeted therapies. Efforts are underway to alleviate these biochemical imbalances and improve patient outcomes through innovative treatments.
Prevalence and Demographics: Who is Affected by Scheie Syndrome?
Scheie Syndrome is a rare form of Mucopolysaccharidosis I (MPS I). Its prevalence is estimated to be about 1 in 300,000 live births. This makes it one of the less common genetic disorders within the MPS spectrum.
“What Is Antiphospholipid Syndrome & Why Does It Cause Blood Clots?”
The syndrome predominantly affects individuals from diverse ethnic backgrounds. While it appears globally, certain populations may exhibit higher frequencies due to founder effects or isolated communities.
Both males and females are affected equally. However, symptoms can vary widely among individuals, even within the same family. Age at diagnosis also differs significantly; some children are diagnosed early in life while others may not show signs until adulthood.
Awareness and understanding of Scheie Syndrome remain limited among healthcare providers. Increased recognition can lead to earlier diagnoses and better management strategies for those impacted by this condition.
Clinical Features: Recognizing the Signs and Symptoms
Scheie Syndrome manifests through a variety of clinical features that vary from person to person. Individuals may experience skeletal abnormalities, including joint stiffness and decreased range of motion. This can lead to discomfort and mobility challenges.
“How Does Apert Syndrome Affect Skull Development? Complete Guide”
Facial characteristics often become more pronounced with age. Patients might develop a broad forehead, prominent brow ridges, and a flattened nasal bridge. Hearing loss is also common, affecting communication abilities.
Vision issues are prevalent due to corneal clouding or retinal problems. These impairments can significantly impact daily life activities.
Growth patterns may be slower than average during childhood but generally do not result in severe short stature as seen in other forms of mucopolysaccharidosis.
Respiratory complications sometimes arise, requiring careful monitoring throughout life. Awareness of these signs is essential for timely diagnosis and management strategies tailored to individual needs.
Diagnostic Criteria: How Scheie Syndrome is Identified
Diagnosing Scheie Syndrome involves a combination of clinical evaluation and specific laboratory tests. Healthcare professionals look for characteristic symptoms, including vision problems, joint stiffness, and distinct facial features.
“What Causes Alport Syndrome? Understanding Hereditary Kidney Disease”
A thorough patient history is essential. Physicians gather information about family health backgrounds to assess genetic links.
Laboratory tests play a vital role too. Enzyme assays measure the activity of alpha-L-iduronidase in blood or skin samples. Low enzyme levels typically indicate MPS I disorders like Scheie Syndrome.
Genetic testing can confirm suspicions by identifying mutations in the IDUA gene responsible for this condition. This method provides definitive evidence and helps differentiate Scheie from other mucopolysaccharidoses.
Imaging studies may also assist in diagnosis, revealing skeletal abnormalities common in affected individuals. Through these combined approaches, healthcare providers can accurately identify and manage Scheie Syndrome effectively.
Laboratory Tests: Enzyme Assays and Genetic Testing
Laboratory tests play a crucial role in diagnosing Scheie Syndrome. Two primary types of tests are commonly utilized: enzyme assays and genetic testing.
“Allan-Herndon-Dudley Syndrome: How Does It Impact Brain Development?”
Enzyme assays measure the activity level of iduronidase, an enzyme that is often deficient in individuals with this condition. A low activity level confirms the suspicion of mucopolysaccharidosis I (MPS I), which includes Scheie Syndrome as its mildest form.
Genetic testing provides further insights by identifying mutations in the IDUA gene responsible for producing iduronidase. This test can confirm a diagnosis even when enzyme levels appear normal or borderline.
Both approaches help healthcare providers develop an accurate understanding of the disorder’s presence and severity, guiding treatment options effectively. Early detection through these laboratory methods enhances patient care and management.
Imaging Studies: The Role of MRI and X-rays in Diagnosis
Imaging studies play a crucial role in diagnosing Scheie Syndrome and monitoring its progression. MRI and X-rays are two primary tools utilized by healthcare professionals.
MRI scans provide detailed images of soft tissues, making them invaluable for assessing organ involvement. They can reveal changes in the brain, spinal cord, and joints that may not be visible through other imaging methods.
X-rays focus on bone structure. In patients with Scheie Syndrome, they can help identify skeletal abnormalities common to mucopolysaccharidosis disorders. These include joint stiffness or deformities due to GAG accumulation.
Both imaging techniques assist in establishing a comprehensive view of the patient’s condition. This aids clinicians in creating personalized treatment plans tailored to individual needs while keeping track of any evolving symptoms over time.
Differential Diagnosis: Distinguishing from Other MPS Disorders
Differentiating Scheie Syndrome from other mucopolysaccharidosis (MPS) disorders is essential for accurate diagnosis and management. Each type of MPS presents distinct clinical features, necessitating a careful evaluation.
For instance, MPS I includes three subtypes: Hurler syndrome, Hurler-Scheie syndrome, and Scheie syndrome. While all share certain symptoms like skeletal abnormalities and organ enlargement, the severity varies significantly. Patients with Hurler syndrome exhibit more pronounced cognitive impairment than those with Scheie.
Additionally, conditions like MPS II (Hunter syndrome) involve different genetic mutations that lead to unique manifestations such as hearing loss or behavioral issues.
Clinical similarities can also occur between Scheie syndrome and other lysosomal storage diseases. Genetic testing plays a crucial role in differentiating these disorders by identifying specific enzymatic deficiencies or gene mutations associated with each condition.
Treatment Options: Managing Scheie Syndrome Symptoms
Managing symptoms of Scheie Syndrome involves a multifaceted approach tailored to the individual’s needs. Treatment primarily focuses on alleviating specific issues that arise due to the disorder.
Enzyme replacement therapy (ERT) is one promising option. This treatment provides patients with the deficient enzyme, helping reduce glycosaminoglycan (GAG) accumulation in tissues and organs. While ERT can improve mobility and overall health, it may not address all manifestations of the syndrome.
Physical therapy plays a crucial role as well. Tailored exercise programs enhance joint function and minimize stiffness, promoting better quality of life.
Regular monitoring by a multidisciplinary team is essential for addressing complications related to organ systems such as heart or respiratory functions. Psychosocial support also contributes significantly to patient wellness by offering emotional guidance for both individuals and families navigating this rare condition.
Enzyme Replacement Therapy: Benefits and Limitations
Enzyme Replacement Therapy (ERT) is a cornerstone treatment for Scheie Syndrome. It involves administering synthetic enzymes to compensate for the deficiency caused by IDUA gene mutations.
One of the major benefits of ERT is its ability to reduce some symptoms associated with GAG accumulation. Patients often experience improvements in mobility and respiratory function after starting therapy. This can significantly enhance quality of life.
However, ERT has limitations. It does not reverse existing damage caused by accumulated GAGs, particularly in organs already affected before treatment initiation. Additionally, continuous infusion or regular injections may be required, which can be inconvenient and costly over time.
Patients might also experience side effects like allergic reactions or infusion-related reactions during ERT sessions. Regular monitoring is essential to manage any adverse effects effectively while maximizing benefits from this therapeutic approach.
Supportive Care: Addressing Specific Organ System Involvement
Supportive care is essential for individuals with Scheie Syndrome, especially as the disorder may affect various organ systems. Tailored interventions can significantly enhance quality of life.
Cardiac monitoring is crucial since heart involvement can occur. Regular echocardiograms help assess any structural changes or valve issues early on.
Respiratory support may be necessary due to airway obstructions and pulmonary complications. Encouraging regular check-ups ensures timely management of these risks.
Skeletal health also requires attention. Physical therapy can improve mobility and reduce discomfort from joint stiffness or pain, which are common in this condition.
Additionally, vision and hearing assessments are important given potential sensory deficits associated with Scheie Syndrome. Early intervention services can provide specialized support tailored to individual needs.
Nutritional counseling might also play a role in managing symptoms effectively, ensuring that patients maintain a balanced diet suited to their unique challenges.
Complications: Potential Long-term Effects of Scheie Syndrome
Scheie Syndrome, while the mildest form of Mucopolysaccharidosis I (MPS I), can lead to various long-term complications. Individuals may experience progressive skeletal deformities due to glycosaminoglycan accumulation. This can impact mobility and overall physical health.
Cardiovascular issues are also a concern. Some patients develop heart valve abnormalities that necessitate ongoing monitoring and potential intervention.
Additionally, ocular problems such as corneal clouding are common, affecting vision over time. Hearing loss might occur because of middle ear infections or structural changes in the ear.
Cognitive function typically remains intact; however, some individuals report challenges related to attention and executive functioning due to chronic illness management demands.
Regular follow-ups with healthcare providers help ensure these complications are identified early, allowing for timely interventions and supportive care tailored to individual needs.
Prognosis: Life Expectancy and Quality of Life
The prognosis for individuals with Scheie Syndrome varies widely. Most affected individuals lead relatively normal lives, especially when diagnosed early and receiving appropriate care. Many manage to maintain a good quality of life into adulthood.
However, some challenges persist. Joint stiffness and pain can impact mobility over time. Hearing loss may also develop, which can affect communication and social interactions.
Regular monitoring of organ function is crucial since complications can arise in the heart or respiratory system as patients age. With advancements in treatment options, including enzyme replacement therapy, many experience improved symptoms.
Psychosocial aspects are vital too. Emotional support from family and communities plays a significant role in enhancing overall well-being for those living with this condition. Each individual’s journey is unique, shaped by their specific health needs and the resources available to them throughout life.
Living with Scheie Syndrome: Daily Challenges and Coping Strategies
Living with Scheie Syndrome presents various daily challenges. Individuals may experience stiffness in joints, vision problems, and hearing loss. These symptoms can make routine activities difficult.
Mobility issues require adaptive strategies. Simple tasks like walking or climbing stairs might need assistive devices, such as canes or walkers. Planning for these needs helps maintain independence.
Regular medical check-ups are essential. Monitoring heart health and joint function is crucial to prevent complications. A multidisciplinary team approach involving physicians, physical therapists, and occupational therapists enhances care.
Emotional well-being is equally important. Connecting with support groups provides a sense of community and shared experiences. Engaging in recreational activities tailored to abilities fosters joy and connection.
Family involvement plays a key role too. Open communication about the condition helps everyone understand the unique challenges faced by those living with Scheie Syndrome. This nurturing environment promotes resilience in navigating everyday life.
Genetic Counseling: Implications for Family Planning
Genetic counseling plays a crucial role for families affected by Scheie Syndrome. This process helps individuals understand the genetic aspects of the disorder.
When parents are carriers of mutations in the IDUA gene, they may benefit from tailored guidance. A genetic counselor can provide insights into inheritance patterns and recurrence risks for future children.
During counseling sessions, families can explore options such as prenatal testing. This allows them to make informed decisions about family planning based on their unique circumstances.
Counselors also offer emotional support, helping families navigate complex feelings that arise with a rare diagnosis. They connect families with resources and support groups that foster understanding and resilience.
Genetic counseling empowers families by equipping them with knowledge. It paves the way for proactive choices regarding health and well-being in future generations.
Research Developments: Current Studies and Future Treatments
Research on Scheie Syndrome is advancing rapidly. Scientists are exploring gene therapy as a potential treatment to correct the underlying genetic defect. By targeting the IDUA gene, they aim to restore normal enzyme function.
Clinical trials are also investigating new enzyme replacement therapies (ERT). These therapies focus on enhancing the delivery and efficacy of enzymes that help break down accumulated GAGs in affected individuals.
Researchers are studying biomarkers for better disease monitoring. Identifying specific markers could lead to improved diagnostic tools and treatment strategies tailored to individual needs.
Additionally, collaboration among institutions worldwide is fostering innovation in therapeutic approaches. New findings are shared across platforms, accelerating progress towards effective treatments.
These developments offer hope for those living with Scheie Syndrome and their families, emphasizing a future where symptoms can be managed more effectively or potentially reversed altogether.
Pediatric Considerations: Managing Scheie Syndrome in Children
Managing Scheie Syndrome in children requires a tailored approach that considers their unique needs. Early diagnosis plays a critical role in optimizing care and improving outcomes for young patients. Parents should be vigilant about recognizing any signs or symptoms, such as developmental delays or joint stiffness, which may indicate the onset of the disorder.
Regular check-ups with a multidisciplinary team—including geneticists, pediatricians, and physical therapists—can help monitor growth and manage complications effectively. These healthcare providers can offer guidance on appropriate therapies to address specific symptoms like joint pain or respiratory issues.
Education is key. Families often benefit from support groups where they can connect with others navigating similar challenges. Sharing experiences can provide emotional relief and practical advice on daily living strategies.
It’s also essential to consider educational accommodations at school to ensure that children receive the necessary support. Implementing an Individualized Education Program (IEP) can facilitate this process by addressing learning differences resulting from Scheie Syndrome.
With ongoing research into better treatment options, staying informed about the latest developments is crucial for families affected by this condition. As knowledge expands around Scheie Syndrome management, so too does hope for improved quality of life for children living with it today.