Sandhoff Syndrome is a rare and complex genetic condition that affects the body’s ability to break down certain fats, leading to severe neurological consequences. For families grappling with this diagnosis, understanding the intricacies of Sandhoff Syndrome can be daunting yet crucial. With only a small number of cases reported globally, awareness remains low outside specialized medical circles.
This post aims to illuminate what Sandhoff Syndrome entails—from its historical roots and genetic foundations to clinical symptoms and potential treatments—providing readers with essential insights into this challenging disorder. Whether you are a healthcare professional, a caregiver, or simply curious about rare diseases, this comprehensive guide will deepen your understanding of Sandhoff Syndrome and its impact on those affected by it.
What is Sandhoff Syndrome? An Overview of This Genetic Condition
Sandhoff Syndrome is a type of lysosomal storage disorder that primarily affects the nervous system. It arises due to a deficiency in specific enzymes needed to break down GM2 gangliosides, which are fatty substances found in nerve cells. As these compounds accumulate, they lead to progressive damage within the brain and spinal cord.
This genetic condition is inherited in an autosomal recessive manner, meaning both parents must pass on a mutated gene for their child to be affected. The syndrome presents itself early in life and varies significantly among individuals.
“What Are The Signs of VACTERL Syndrome in Newborns?”
Symptoms can range from developmental delays and motor skill deficits to seizures and vision problems. While Sandhoff Syndrome shares similarities with other disorders like Tay-Sachs disease, it has distinct clinical features that necessitate precise diagnosis and management strategies tailored to each patient’s needs.
Historical Background: Konrad Sandhoff and the Discovery of the Syndrome
Konrad Sandhoff was a pivotal figure in the realm of genetics and biochemistry. His research during the mid-20th century laid the groundwork for understanding various lysosomal storage disorders.
In 1968, he made significant strides in identifying what would later be known as Sandhoff Syndrome. Through meticulous study, he discovered that certain genetic mutations could lead to harmful accumulations of GM2 gangliosides in cells.
“Why Does Van der Woude Syndrome Cause Cleft Lip?”
This groundbreaking work was instrumental not only for Sandhoff Syndrome but also for other related conditions like Tay-Sachs disease. The insights gained from his research helped propel advancements in biochemical analysis and genetic testing.
Sandhoff’s contributions have had lasting impacts on both clinical practice and scientific inquiry, paving paths toward better diagnostic methods and therapeutic strategies. His legacy continues to inspire researchers working on rare genetic disorders today.
Genetic Basis: The Role of HEXB Gene Mutations
Sandhoff Syndrome is primarily caused by mutations in the HEXB gene. This gene plays a crucial role in producing an enzyme called beta-hexosaminidase. This enzyme is essential for breaking down certain fatty substances in the body.
“How Does Variably Protean Syndrome Present?”
When mutations occur, the production of this enzyme is severely impaired or even halted. As a result, toxic levels of GM2 gangliosides accumulate within cells, particularly affecting neurons.
These genetic mutations can be inherited in an autosomal recessive manner. Both parents must carry one copy of the mutated gene for their child to be affected. Genetic testing can help identify carriers and provide insights into familial risk factors.
Understanding these genetic underpinnings highlights the significance of early diagnosis and potential interventions for those impacted by Sandhoff Syndrome.
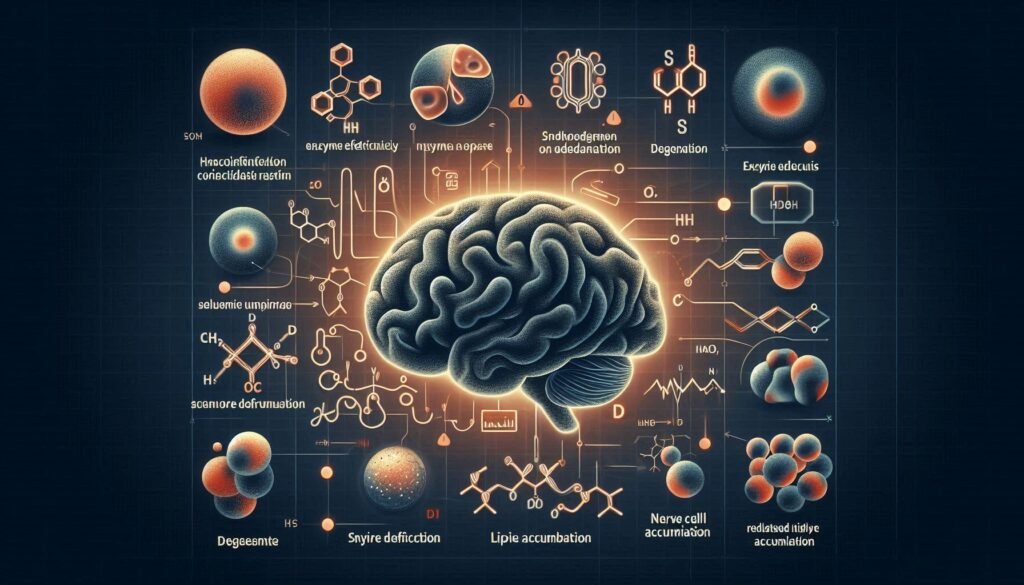
Biochemistry of Sandhoff Syndrome: GM2 Ganglioside Accumulation
Sandhoff Syndrome is characterized by the accumulation of GM2 gangliosides, a type of fatty substance crucial for nerve function. This buildup occurs due to a deficiency in hexosaminidase B (Hex-B), an enzyme responsible for breaking down these complex lipids within lysosomes.
“What Causes Valentine Syndrome? Heart Condition Guide”
When Hex-B is deficient, GM2 gangliosides cannot be adequately processed. As they accumulate, they disrupt cellular functions and lead to significant neurological impairment. The brain and spinal cord are particularly affected because neurons rely heavily on proper lipid metabolism.
This biochemical dysfunction not only contributes to the degeneration of neural tissues but also exacerbates other symptoms associated with Sandhoff Syndrome. Understanding this process is vital for developing potential treatments aimed at halting or reversing the effects of this storage disorder.
Types of Sandhoff Syndrome: Infantile, Juvenile, and Adult-Onset Forms
Sandhoff Syndrome presents in three main forms: infantile, juvenile, and adult-onset. Each type varies significantly in terms of onset age and symptom severity.
The infantile form typically manifests within the first few months of life. Affected infants may show developmental delays, loss of motor skills, and noticeable neurological decline. These children often experience a rapid progression of symptoms.
“Why Does Vanishing White Matter Syndrome Progress?”
Juvenile Sandhoff Syndrome usually appears between ages 2 to 4 years. Children with this form might initially develop normally but later exhibit behavioral changes and cognitive decline. Neurological complications become more pronounced as they grow older.
Adult-onset Sandhoff Syndrome is the rarest variant and can emerge in late adolescence or early adulthood. Symptoms are often milder compared to the earlier forms but include progressive weakness, movement difficulties, and psychiatric issues as individuals age. Understanding these distinctions aids in timely diagnosis and management strategies for affected families.
Prevalence and Demographics: Who is Affected by Sandhoff Syndrome?
Sandhoff Syndrome is a rare genetic disorder primarily affecting specific populations. It is most commonly found in individuals of Ashkenazi Jewish descent, where the carrier frequency can be as high as 1 in 27.
Globally, cases are scarce. Estimates suggest that Sandhoff Syndrome occurs in approximately 1 in 300,000 births. This low prevalence makes awareness crucial for early diagnosis and intervention.
“How Does VATER Syndrome Affect Multiple Systems?”
The condition affects males and females equally; however, its presentation varies significantly across different age groups. The infantile form typically manifests earlier and has a more severe clinical course compared to juvenile or adult-onset forms.
Genetic counseling plays an essential role for families with a history of the syndrome. Understanding risk factors helps identify carriers within communities at higher risk, paving the way for informed reproductive choices and management strategies.
Clinical Features: Recognizing the Signs and Symptoms
Recognizing the signs and symptoms of Sandhoff Syndrome is crucial for early diagnosis. The clinical features often vary based on the onset type—infantile, juvenile, or adult.
In infants, developmental delays are prominent. They may show a lack of muscle tone and difficulty with motor skills. As the condition progresses, hearing loss and vision problems typically emerge.
Juvenile forms present different challenges. Children might experience seizures along with cognitive decline. Behavioral changes can also occur as neurological function deteriorates.
Adult-onset patients may exhibit milder symptoms initially but can develop mood disturbances or progressive weakness over time.
Regardless of age at onset, all types share common characteristics such as movement disorders and speech difficulties as they progress. Awareness of these clinical manifestations aids in prompt medical intervention for affected individuals.
Neurological Manifestations: Central Nervous System Involvement
Neurological manifestations are prominent in individuals with Sandhoff Syndrome. The central nervous system (CNS) is profoundly affected, leading to various symptoms that can significantly impact daily life.
Patients often experience developmental delays and cognitive decline. These issues arise due to the accumulation of GM2 gangliosides within nerve cells. This buildup disrupts normal cellular function.
Motor skills may also deteriorate over time, resulting in muscle weakness or paralysis. Seizures are another troubling symptom linked to CNS involvement, affecting a person’s overall stability and quality of life.
Behavioral changes can occur as well. Children may show increased irritability or social withdrawal as the condition progresses. Regular monitoring by healthcare professionals is essential for managing these symptoms effectively and ensuring timely interventions when needed.
Diagnostic Criteria: How Sandhoff Syndrome is Identified
Diagnosing Sandhoff Syndrome involves a combination of clinical assessment and laboratory testing. Physicians typically start with a comprehensive evaluation of the patient’s medical history and symptoms.
Key indicators include neurological decline, developmental delays, and specific physical signs like cherry-red spots in the eyes. These observations can guide clinicians toward further diagnostic measures.
Laboratory tests play a crucial role in confirming the diagnosis. Enzyme activity assays are performed to measure Hexosaminidase A and B levels. A significant reduction suggests Sandhoff Syndrome.
In addition to enzyme assays, genetic testing is vital for identifying mutations in the HEXB gene. This helps confirm the diagnosis and clarifies potential inheritance patterns within families.
Imaging studies such as MRI may also be employed to assess brain structure changes over time, providing additional insight into disease progression during monitoring sessions.
Laboratory Tests: Enzyme Assays and Genetic Testing
Laboratory tests play a crucial role in diagnosing Sandhoff Syndrome. Enzyme assays are commonly used to detect deficiencies in specific enzymes involved in lipid metabolism. In this case, the focus is on hexosaminidase B (HexB), which is essential for breaking down GM2 gangliosides.
By measuring enzyme activity levels in blood or tissue samples, healthcare providers can determine whether a patient has Sandhoff Syndrome or another related disorder. Low HexB activity indicates a potential diagnosis.
Genetic testing complements enzyme assays by identifying mutations in the HEXB gene responsible for the condition. This test provides definitive confirmation of Sandhoff Syndrome and helps inform family planning decisions for affected families.
Both laboratory methods are significant not only for diagnosis but also for understanding an individual’s specific mutation profile, paving the way for personalized treatment options and ongoing research into targeted therapies.
Imaging Studies: The Role of MRI in Diagnosis and Monitoring
Magnetic Resonance Imaging (MRI) plays a crucial role in the diagnosis and management of Sandhoff Syndrome. This non-invasive imaging technique offers detailed insights into brain structure and function.
In patients with Sandhoff Syndrome, MRI can reveal characteristic changes in brain morphology. These changes often manifest as atrophy or abnormal signaling patterns that correlate with disease progression.
Doctors utilize MRI not just for initial diagnosis but also for monitoring disease advancement over time. Regular scans help track neurological deterioration, providing essential information to tailor treatment strategies effectively.
Additionally, advanced MRI techniques such as diffusion tensor imaging (DTI) may offer deeper insights into white matter integrity. By assessing these aspects, healthcare providers can better understand the impact of the disorder on cognitive functions and overall quality of life.
Differential Diagnosis: Distinguishing from Other Lysosomal Storage Disorders
Differential diagnosis is crucial when identifying Sandhoff Syndrome. This genetic condition shares symptoms with other lysosomal storage disorders, making accurate recognition challenging.
Conditions like Tay-Sachs disease and GM1 gangliosidosis present similar neurological features. For instance, both can cause progressive weakness and cognitive decline. However, distinguishing factors exist in the specific enzyme deficiencies involved.
Clinicians often rely on detailed patient history and physical examinations to differentiate these disorders. Genetic testing plays a pivotal role as well, pinpointing mutations in the HEXB gene unique to Sandhoff Syndrome.
Enzyme assays can help confirm diagnoses by measuring activity levels of hexosaminidase A and B enzymes. These tests provide essential insights into metabolic function that aids differentiation from closely related conditions.
Swift identification ensures appropriate management plans are put in place for affected individuals. Timely intervention can significantly impact patient care strategies moving forward.
Treatment Options: Current Approaches to Managing Sandhoff Syndrome
Treatment options for Sandhoff Syndrome primarily focus on managing symptoms, as there is currently no cure. Supportive care plays a crucial role in enhancing the quality of life for affected individuals.
Physical therapy can help maintain mobility and prevent contractures. Speech therapy may assist with communication challenges that arise as the disease progresses. Occupational therapy often focuses on adapting daily activities to improve independence.
Medications are prescribed to alleviate specific symptoms, such as seizures or muscle spasms. Nutritional support becomes essential, particularly in later stages when swallowing difficulties may occur.
Research into more advanced therapies continues to evolve. Gene therapy aims to correct the underlying genetic mutations, while enzyme replacement strategies seek to provide missing enzymes needed for metabolic processes. These experimental approaches offer hope but remain under investigation and not yet widely available in clinical practice.
Supportive Care: Addressing Specific Symptoms and Complications
Supportive care plays a crucial role in managing Sandhoff Syndrome. Each patient experiences unique challenges, making individualized care essential.
Physical therapy can enhance mobility and strength. It helps address muscle weakness and coordination issues common in affected individuals. Regular sessions may improve overall function.
Speech therapy is vital for communication difficulties. Many patients struggle with verbal expression or swallowing. A speech therapist can offer tailored strategies to facilitate better interaction.
Nutritional support also requires attention. Dietary adjustments are necessary to manage feeding problems or weight loss due to difficulty eating.
Psychological support benefits both patients and families coping with the emotional toll of the condition. Counseling provides tools for dealing with stress, anxiety, and grief.
Respite care services allow caregivers much-needed breaks while ensuring that their loved ones receive quality supervision and assistance during difficult times. Such arrangements foster a supportive environment conducive to well-being.
Experimental Therapies: Gene Therapy and Enzyme Replacement Research
Research into experimental therapies for Sandhoff Syndrome is progressing, particularly in gene therapy and enzyme replacement strategies.
Gene therapy aims to correct the underlying genetic defect by delivering a functional copy of the HEXB gene. This approach has shown promise in animal models, demonstrating the potential to restore deficient enzyme activity and improve neurological function.
Enzyme replacement therapy (ERT) involves administering synthetic or recombinant forms of the missing enzyme, beta-hexosaminidase. Early studies suggest that ERT might help alleviate some symptoms by reducing GM2 ganglioside accumulation in cells.
These innovative treatments are still largely in clinical trial phases. However, they offer hope for affected individuals and families seeking more effective management options as research continues to evolve.
Pediatric Considerations: Managing Sandhoff Syndrome in Children
Managing Sandhoff Syndrome in children requires a comprehensive and compassionate approach. Early diagnosis is crucial, as it allows for timely interventions that can improve quality of life. Care teams often include pediatricians, neurologists, genetic counselors, and therapists who work together to address the complex needs of affected children.
Children with Sandhoff Syndrome may experience developmental delays and neurological issues. Tailored educational plans and therapies are vital to support their learning and daily functioning. Occupational therapy can help enhance motor skills, while speech therapy supports communication abilities.
Family support plays an essential role in managing the condition. Connecting families with support groups provides emotional resources and access to shared experiences from others facing similar challenges. These connections foster a sense of community among caregivers navigating this rare disorder.
As research progresses into potential treatments—such as gene therapy or enzyme replacement—the hope for improved management strategies continues to grow. Each child’s journey is unique, making personalized care plans necessary for addressing individual symptoms effectively.
With ongoing advancements in science and medicine coupled with strong family involvement, there’s room for optimism in caring for children impacted by Sandhoff Syndrome. The focus remains on enhancing their lives through informed strategies that promote well-being at every stage of development.
Prognosis: Life Expectancy and Quality of Life for Different Forms
The prognosis for individuals with Sandhoff Syndrome varies significantly based on the age of onset and the specific form of the disorder.
Infantile Sandhoff Syndrome presents challenges early in life, leading to severe neurological decline. Most affected infants do not survive beyond their early years, often succumbing to complications associated with progressive neurodegeneration.
Juvenile forms may allow for a longer lifespan but still result in significant disability as symptoms progress. Many children diagnosed during this stage can live into late childhood or adolescence but face increasing limitations due to motor and cognitive impairments.
Adult-onset cases tend to have a more insidious progression and can lead to varying levels of functional independence well into adulthood. However, these individuals may experience debilitating symptoms that severely impact their quality of life over time.
Despite advancements in understanding and managing Sandhoff Syndrome, it remains a challenging condition with serious implications for patients and families alike. Ongoing research offers hope through potential therapies aimed at slowing disease progression or alleviating symptoms, providing some optimism for those affected by this rare lysosomal storage disorder.