Renal Fanconi Syndrome (RFS) is a rare but significant kidney disorder that can be perplexing for both patients and healthcare providers alike. This condition disrupts the kidneys’ ability to reabsorb essential nutrients, leading to a cascade of health issues. While it may not be as widely recognized as other renal disorders, understanding RFS is crucial for effective management and treatment.
From its historical roots linked to renowned physician Guido Fanconi to the complexities of its pathophysiology, Renal Fanconi Syndrome encompasses a diverse range of clinical presentations. Whether it’s caused by genetic factors or acquired through medications and underlying conditions, RFS poses unique challenges that require prompt diagnosis and tailored interventions.
Navigating life with Renal Fanconi Syndrome often involves recognizing key symptoms early on, undergoing specific laboratory tests, and implementing dietary adjustments that support kidney function. In this comprehensive guide, we will delve into every facet of RFS—from its causes to innovative research developments—providing you with valuable insights into living well with this complex disorder. Join us as we explore the intricate world of Renal Fanconi Syndrome together!
What is Renal Fanconi Syndrome? Understanding the Basics
Renal Fanconi Syndrome is a disorder that primarily affects the kidneys’ ability to reabsorb essential substances. This dysfunction leads to the loss of vital nutrients, such as glucose, amino acids, bicarbonate, and phosphate in urine.
Though classified as a tubular defect, RFS can result in severe metabolic imbalances. Patients often experience symptoms like growth retardation in children or bone issues due to mineral deficiencies.
“Why Does Nephrotic Syndrome Cause Protein Loss?”
This syndrome can arise from various causes. It may be inherited genetically or develop secondary to other conditions or medications. Understanding these nuances helps healthcare providers tailor treatment plans effectively.
Awareness of Renal Fanconi Syndrome is crucial for early diagnosis and intervention. Identifying this condition allows for better management strategies that improve patients’ quality of life while minimizing complications associated with nutrient loss.
Historical Context: Guido Fanconi and the Discovery of the Syndrome
Guido Fanconi, a Swiss pediatrician, made significant contributions to the field of medicine in the early 20th century. His work primarily focused on childhood diseases and genetic disorders.
In 1931, he first described what would later be known as Renal Fanconi Syndrome. His observations highlighted a set of symptoms associated with kidney dysfunction that particularly affected children. The syndrome emerged from his studies on metabolic conditions leading to renal tubular defects.
“How Does Nail-Patella Syndrome Affect Development?”
Fanconi’s meticulous research laid the groundwork for understanding this rare disorder’s impact on electrolyte balance and nutrient absorption. He identified key clinical features such as phosphaturia and aminoaciduria, which are critical in diagnosing RFS today.
His legacy continues through ongoing research into the causes and treatments of this complex condition, making him a pivotal figure in nephrology history.
Pathophysiology: How Renal Fanconi Syndrome Affects Kidney Function
Renal Fanconi Syndrome disrupts the kidney’s ability to reabsorb essential substances. This malfunction primarily occurs in the proximal tubules, where vital nutrients and electrolytes are normally absorbed back into the bloodstream.
In healthy kidneys, glucose, amino acids, bicarbonate, and phosphate are efficiently reabsorbed. However, in Fanconi Syndrome, these processes are impaired. As a result, patients often experience significant loss of these critical components through urine.
“What Causes Nasal Glioma Syndrome in Infants?”
This condition leads to various metabolic imbalances. For instance, renal phosphate wasting can cause rickets or osteomalacia due to poor bone mineralization. Similarly, bicarbonate loss results in acidosis—an elevated acidity level that can affect overall health.
The impact on kidney function is profound. Patients may develop chronic kidney disease if left untreated over time due to ongoing tubular damage and dysfunction associated with this syndrome. Understanding these mechanisms is crucial for effective management and treatment strategies.
Types of Renal Fanconi Syndrome: Primary vs Secondary Forms
Renal Fanconi Syndrome is categorized into two main types: primary and secondary forms.
Primary Renal Fanconi Syndrome, often inherited, typically arises due to genetic mutations. This form can appear in childhood or early adulthood and may be associated with specific disorders like cystinosis or galactosemia. The dysfunction occurs as a result of faulty transport mechanisms in the kidney’s tubules.
Secondary Renal Fanconi Syndrome develops due to external factors rather than genetic issues. Various conditions such as multiple myeloma, certain viral infections, or prolonged exposure to toxins can trigger this syndrome. Medications like tenofovir and outdated antibiotics also play a role.
“Why Does Neurocutaneous Melanosis Syndrome Occur?”
Understanding these distinctions is crucial for effective diagnosis and treatment planning. Each type presents unique challenges that require tailored approaches from healthcare providers.
Genetic Factors: Inherited Causes of Renal Fanconi Syndrome
Genetic factors play a crucial role in the development of Renal Fanconi Syndrome (RFS). Some forms of this kidney disorder are inherited, often following an autosomal recessive pattern. This means both parents must pass on the defective gene for their child to develop RFS.
Several genetic mutations have been identified as contributing to primary Renal Fanconi Syndrome. Notable conditions include cystinosis, which causes cystine accumulation and subsequent damage to renal tubular cells. Another example is tyrosinemia type 1, arising from deficiencies in specific enzymes essential for amino acid metabolism.
“How Does Sleep Apnea Syndrome Affect Your Health?”
Patients with these inherited forms may experience symptoms early in life due to significant metabolic disruptions. Genetic testing can help diagnose these conditions, guiding families through informed decision-making regarding treatment options and management strategies tailored specifically for them.
Acquired Causes: Medications and Conditions That Can Lead to RFS
Acquired causes of Renal Fanconi Syndrome (RFS) can arise from various medications and underlying health conditions. Certain drugs, particularly those used in chemotherapy or long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), have been linked to kidney damage.
Antibiotics like tetracycline and certain antivirals can also disrupt renal function. It’s vital for healthcare providers to monitor patients on these treatments closely.
“What Causes Oculocerebrorenal Syndrome? Expert Guide”
Additionally, diseases such as multiple myeloma or cystinosis may contribute to the development of RFS. These conditions alter how kidneys process waste and electrolytes, leading to functional impairment.
Infections, such as viral hepatitis or cytomegalovirus, are other potential triggers that could lead to this syndrome. Awareness of these factors is essential for timely diagnosis and management in affected individuals.
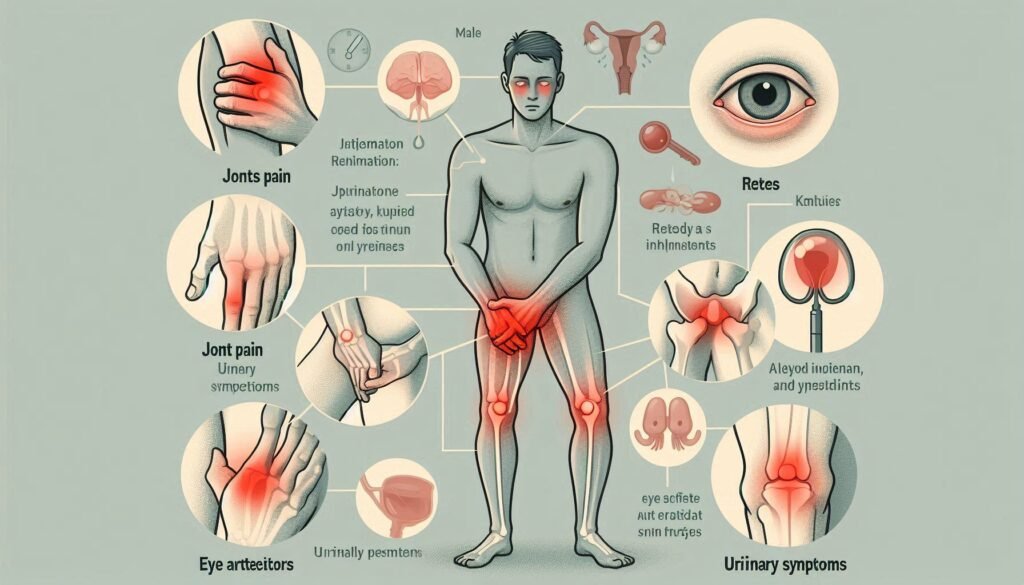
Clinical Presentation: Key Signs and Symptoms to Recognize
Renal Fanconi Syndrome (RFS) can manifest through a variety of signs and symptoms. Early recognition is crucial for effective management.
Patients often experience excessive thirst and increased urination. This is due to the kidneys’ inability to concentrate urine properly. As a result, dehydration can become an issue.
Another common symptom includes metabolic acidosis, which may lead to fatigue and weakness. This occurs when the body fails to eliminate acids efficiently.
Bone pain or deformities might also arise because of impaired phosphate reabsorption. Patients may notice growth delays in children as well.
Additionally, some individuals develop proteinuria, leading to swelling in various parts of the body. Recognizing these symptoms early on can help guide appropriate testing and treatment strategies for those affected by RFS.
Diagnostic Criteria: How Renal Fanconi Syndrome is Identified
Diagnosis of Renal Fanconi Syndrome (RFS) requires careful evaluation. Healthcare providers start with a comprehensive patient history and physical examination. Recognizing key signs is crucial.
Laboratory tests play an essential role in identifying RFS. Clinicians analyze urine for specific abnormalities, such as glucosuria, phosphaturia, and aminoaciduria. These findings indicate that the kidneys are not reabsorbing these substances effectively.
Blood tests complement urine analysis by revealing metabolic imbalances like acidosis or electrolyte disturbances. This information helps distinguish RFS from other renal conditions.
Imaging studies may also assist in ruling out structural abnormalities within the kidneys. Ultrasound or CT scans can provide valuable insights into kidney anatomy and function.
A multidisciplinary approach ensures accurate diagnosis tailored to each patient’s unique situation, paving the way for effective management strategies.
Laboratory Tests: Urine and Blood Analysis in Diagnosis
Laboratory tests play a crucial role in diagnosing Renal Fanconi Syndrome. These tests primarily focus on urine and blood analysis to evaluate kidney function.
A 24-hour urine collection is often conducted to measure the levels of various substances such as glucose, amino acids, phosphate, and bicarbonate. Elevated levels of these components can indicate tubular dysfunction characteristic of RFS.
Blood tests are equally important. They help assess electrolyte balance and renal function by measuring creatinine and blood urea nitrogen (BUN) levels. Abnormalities in these markers can signal an issue with kidney performance.
Additionally, serum electrolytes like sodium, potassium, and calcium provide insight into metabolic imbalances that may arise due to the disorder. Identifying these abnormalities aids healthcare providers in confirming a diagnosis while guiding further treatment strategies for affected individuals.
Imaging Studies: The Role of Radiological Investigations
Imaging studies play a vital role in diagnosing Renal Fanconi Syndrome. These investigations help visualize kidney structure and function, offering insights that lab tests alone cannot provide.
Ultrasound is often the first step. It allows doctors to assess kidney size and detect any anatomical abnormalities. This non-invasive method provides real-time images, making it a preferred choice for initial evaluations.
CT scans can offer deeper insights into renal architecture. They generate detailed cross-sectional images of the kidneys, which may reveal cysts or tumors that could contribute to symptoms.
MRI has emerged as another valuable tool. Its ability to highlight soft tissue differences helps identify underlying issues affecting kidney performance without exposing patients to radiation.
Together, these imaging techniques enhance diagnostic accuracy, enabling healthcare providers to develop targeted treatment plans for those affected by this complex disorder.
Treatment Approaches: Managing Symptoms and Underlying Causes
Treatment for Renal Fanconi Syndrome focuses on alleviating symptoms and addressing underlying causes. A multidisciplinary approach is often necessary, involving nephrologists, dietitians, and other healthcare professionals.
Managing electrolyte imbalances is crucial. Patients frequently require supplements to replenish levels of potassium, bicarbonate, or phosphate that the kidneys fail to retain effectively.
Medications may also play a role in treatment. Specific drugs can correct metabolic issues or address complications arising from the syndrome. For instance, some patients benefit from medications that help manage blood pressure or control diabetes if these conditions coexist with RFS.
Dietary modifications are essential as well. A low-protein diet might be recommended to reduce kidney workload while ensuring adequate caloric intake through healthy fats and carbohydrates.
Regular monitoring of kidney function and overall health helps tailor treatments specifically to each patient’s needs, promoting better outcomes over time.
Electrolyte Replacement: Correcting Metabolic Imbalances
Electrolyte replacement is crucial for individuals with Renal Fanconi Syndrome. This condition often leads to significant imbalances in essential minerals like sodium, potassium, and bicarbonate.
Due to kidney dysfunction, the body struggles to maintain normal electrolyte levels. As a result, patients can experience symptoms such as muscle weakness, fatigue, and irregular heart rhythms.
To address these imbalances, healthcare providers typically recommend tailored electrolyte supplementation. This may involve oral supplements or intravenous (IV) fluids for more severe cases.
Regular monitoring of blood tests helps track the effectiveness of treatment plans. Adjustments might be necessary based on individual responses and changing needs over time.
Dietary modifications can also play a role in managing electrolytes. Incorporating foods rich in specific minerals aids recovery while ensuring nutritional needs are met without additional strain on the kidneys.
Medications: Specific Treatments for Different Types of RFS
Medications play a crucial role in managing Renal Fanconi Syndrome, especially when addressing specific types. For primary forms, treatment often includes medications that can effectively manage symptoms and metabolic imbalances.
In cases of cystinosis-related RFS, cysteamine is commonly prescribed. This medication helps reduce cystine accumulation in the kidneys and is essential for preserving kidney function over time.
For secondary forms caused by conditions like multiple myeloma, treating the underlying disease is vital. Chemotherapy or targeted therapies may alleviate renal complications associated with these disorders.
Additionally, phosphate binders are sometimes used to prevent hypophosphatemia. These help regulate phosphate levels and minimize bone health issues resulting from RFS.
Regular follow-ups with healthcare providers ensure that treatments remain effective and adjusted as necessary based on individual patient needs. Each case requires tailored medication strategies for optimal management of this complex syndrome.
Nutritional Management: Dietary Considerations for Patients
Nutritional management is crucial for patients with Renal Fanconi Syndrome. This condition can lead to significant nutrient losses, particularly electrolytes and vitamins.
A well-balanced diet focused on replenishing these nutrients is essential. Patients should aim for foods rich in potassium, sodium, calcium, and phosphorus. These minerals help counteract deficiencies caused by the syndrome.
Limiting processed foods is also recommended. Such items often contain high levels of sugars and unhealthy fats that can exacerbate metabolic issues. Instead, whole foods like fruits, vegetables, lean proteins, and whole grains should form the basis of their meals.
Hydration plays a key role as well. Drinking adequate fluids helps support kidney function while preventing dehydration from excessive urination associated with RFS.
Consulting a registered dietitian experienced in renal health can provide personalized dietary plans tailored to individual needs and preferences.
Complications: Potential Long-term Effects of Renal Fanconi Syndrome
Renal Fanconi Syndrome can lead to various long-term complications that significantly impact a patient’s quality of life. One major concern is renal failure, which may develop if the underlying issues are not managed appropriately.
Patients often experience metabolic acidosis due to impaired bicarbonate reabsorption. This condition can affect overall health and may require ongoing treatment.
Bone health is also compromised, as the kidneys struggle to maintain phosphate balance. This imbalance increases the risk of rickets in children and osteomalacia in adults.
Additionally, electrolyte imbalances are common, potentially leading to dangerous conditions like hypokalemia or hyperkalemia. These fluctuations demand careful monitoring and management.
Affected individuals may face growth delays or developmental challenges during childhood years. Regular check-ups become crucial for early intervention and support throughout their lives.
Prognosis: Long-term Outlook for Individuals with RFS
The long-term outlook for individuals with Renal Fanconi Syndrome (RFS) varies significantly based on its underlying causes. For those with primary forms, especially genetic conditions, prognosis can be more complex. Patients may face chronic kidney disease over time.
Secondary RFS, often linked to medications or other medical conditions, might improve once the triggering factor is addressed. Early intervention plays a crucial role in managing symptoms and slowing progression.
Monitoring is essential for maintaining kidney function and overall health. Regular check-ups allow healthcare providers to adjust treatment plans as needed.
Many patients lead fulfilling lives despite having RFS. With appropriate management of electrolyte imbalances and nutritional needs, they can mitigate some complications associated with this disorder. Ongoing research continues to shed light on better treatments and supportive therapies that enhance quality of life for those affected by Renal Fanconi Syndrome.
Pediatric Renal Fanconi Syndrome: Special Considerations in Children
Pediatric Renal Fanconi Syndrome presents unique challenges that differ from adult cases. Children often exhibit symptoms like growth retardation and developmental delays due to the loss of essential nutrients.
Diagnosis in young patients can be tricky. Clinicians must rely heavily on a combination of urine tests and family history, as symptoms may overlap with other conditions.
Treatment requires a tailored approach. Children need careful monitoring for electrolyte imbalances and nutritional deficiencies. Specific dietary adjustments play a crucial role in their management plan.
Educating caregivers is vital. Parents should understand how to recognize warning signs early, ensuring timely interventions.
Additionally, ongoing research is critical for understanding RFS in pediatric populations better. New insights could lead to improved therapies aimed at minimizing long-term complications associated with this syndrome.
Living with RFS: Daily Challenges and Coping Strategies
Living with Renal Fanconi Syndrome (RFS) presents daily challenges that can impact various aspects of life. Patients often experience fatigue, muscle weakness, and frequent urination. These symptoms can disrupt routines and affect social interactions.
Managing dietary restrictions is crucial for maintaining health. Individuals may need to limit certain nutrients like phosphorus or potassium while ensuring adequate hydration. This requires careful planning during meals and snacks.
Emotional support plays a vital role in coping with RFS. Connecting with friends, family, or support groups can help alleviate feelings of isolation. Sharing experiences often leads to practical advice on managing the condition.
Regular communication with healthcare providers is essential for monitoring progress and adjusting treatment plans as needed. Keeping track of medications and follow-up appointments helps in staying organized.
Incorporating gentle physical activity into daily life can improve overall well-being. Activities such as walking or yoga enhance mood while supporting kidney function management.
Research Developments: Current Studies and Future Directions
Research into Renal Fanconi Syndrome (RFS) is continually evolving, shedding light on this complex kidney disorder. Current studies are focusing on understanding the underlying mechanisms that contribute to both primary and secondary forms of RFS. An emphasis is being placed on genetic research, which aims to identify specific mutations responsible for inherited cases. This knowledge could lead to more targeted therapies and improved outcomes for affected individuals.
Advancements in imaging techniques also hold promise for early diagnosis and better monitoring of the disease’s progression. Researchers are exploring novel biomarkers in blood and urine tests that could enhance diagnostic accuracy.
Clinical trials are underway testing new medications aimed at addressing the metabolic imbalances often associated with RFS. These treatments may not only alleviate symptoms but also protect kidney function over time.
As our understanding deepens, there’s hope for developing personalized medicine approaches tailored to individual patients based on their unique genetic profiles and health needs. The future looks promising as scientists continue their quest to unravel the complexities of Renal Fanconi Syndrome, paving the way toward better management strategies and potential cures.