Reiter’s Syndrome, more commonly known as reactive arthritis, is a condition that can take many by surprise. Often triggered by infections, it brings along an array of symptoms that can impact daily life. Are you dealing with joint pain or discomfort following an infection? This may be more than just a temporary setback.
Understanding Reiter’s Syndrome is crucial for anyone who has experienced its effects or wants to learn about this complex condition. It’s important to delve into the basics and explore how it manifests in different individuals. With insights spanning from historical context to modern treatment options, this guide aims to provide clarity on what Reiter’s Syndrome truly entails.
Join us as we navigate through the intricacies of reactive arthritis—its causes, symptoms, diagnostic criteria, and effective management strategies. Whether you’re seeking knowledge for yourself or looking to support someone else affected by this syndrome, there’s something here for everyone interested in unraveling the mysteries of Reiter’s Syndrome.
What is Reiter’s Syndrome? Understanding the Basics of Reactive Arthritis
Reiter’s Syndrome is a type of reactive arthritis that typically arises following an infection. It primarily affects the joints, eyes, and urinary tract. Patients often experience inflammation as their immune system responds to these infections.
“How Does Yashiro Syndrome Present?”
While it can occur in anyone, Reiter’s Syndrome is more prevalent in young men. The most common triggers include sexually transmitted infections or gastrointestinal infections caused by bacteria like Chlamydia or Salmonella.
The condition manifests through joint pain and swelling that may appear weeks after the initial infection has cleared up. This delayed response can make diagnosis challenging but highlights the importance of understanding its connection to previous health issues.
Reiter’s Syndrome serves as a reminder of how interconnected our bodily systems are. Recognizing its symptoms early on could lead to timely treatment and better outcomes for those affected by this complex autoimmune response.
Historical Context: Hans Reiter and the Controversy Surrounding the Name
Reiter’s Syndrome is named after Hans Reiter, a German physician who described the condition in the 1910s. Initially recognized for his contributions to understanding reactive arthritis, Reiter’s work laid the foundation for future research.
However, naming this syndrome after him has stirred controversy. Hans Reiter was later linked to unethical practices during World War II and had affiliations with Nazi ideology. This association raised ethical concerns about honoring someone with such a tainted legacy.
“What Are The Signs of Y Chromosome Infertility Syndrome?”
As awareness of these historical implications grew, many in the medical community advocated for renaming the condition. Terms like “reactive arthritis” have gained preference as they focus on clinical characteristics rather than controversial figures.
This discussion highlights an essential aspect of medicine: how history interacts with modern practice and ethics. It encourages ongoing dialogue about terminology within healthcare fields while striving to maintain sensitivity toward those affected by these conditions.
Etiology: Triggers and Causes of Reiter’s Syndrome
Reiter’s Syndrome, also known as reactive arthritis, often arises following an infection. This connection is pivotal in understanding its etiology.
Common triggers include bacterial infections of the urogenital or gastrointestinal systems. Chlamydia trachomatis and Salmonella species are frequently implicated in these cases.
“Why Does Zaitsev Syndrome Affect Development?”
Other infections like Yersinia enterocolitica and Campylobacter jejuni can also lead to the onset of symptoms. Interestingly, not everyone who experiences these infections will develop Reiter’s Syndrome, suggesting a complex interplay between genetic predisposition and environmental factors.
Additionally, certain lifestyle choices may influence susceptibility. Stress levels and diet might play subtle roles in how the immune system responds post-infection.
Recognizing these potential triggers helps guide both prevention strategies and treatment approaches for those at risk of Reiter’s Syndrome.
Pathophysiology: How Reiter’s Syndrome Affects the Body
Reiter’s Syndrome, a form of reactive arthritis, involves an autoimmune response triggered by infections. This condition primarily affects the joints but can also impact other systems in the body.
When exposed to certain pathogens, such as Chlamydia or Salmonella, the immune system becomes hyperactive. It mistakenly targets healthy tissues alongside the invading microbes. This misdirected attack leads to inflammation and swelling in various joints.
“How Does Zaspopathy Syndrome Impact Health?”
The typical areas affected include knees, ankles, and feet. However, Reiter’s can also manifest in tendons and ligaments surrounding these joints. Inflammation may extend beyond musculoskeletal issues; it can involve the eyes and urinary tract too.
The interplay between genetic predisposition and environmental factors contributes significantly to symptoms severity. Understanding this pathophysiology is crucial for effective management strategies tailored to individual needs.
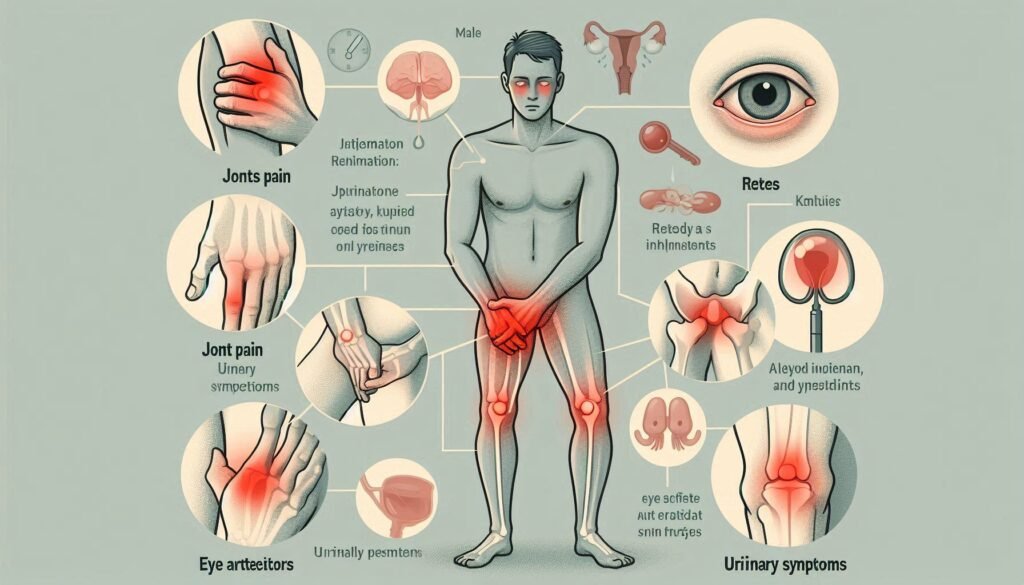
Clinical Triad: Arthritis, Urethritis, and Conjunctivitis in Reiter’s Syndrome
Reiter’s Syndrome is characterized by a distinct clinical triad: arthritis, urethritis, and conjunctivitis. Each component plays a critical role in diagnosis.
Arthritis often manifests as inflammation in the joints, particularly affecting the knees, ankles, and feet. Patients may experience pain and stiffness that can severely impact mobility.
Urethritis presents with urinary symptoms like burning sensations or increased frequency of urination. This often follows a genitourinary infection but can vary among individuals.
“What Causes Zellweger Syndrome? Metabolic Guide”
Conjunctivitis typically leads to redness and irritation of the eyes. Some patients report sensitivity to light or discharge, which can be uncomfortable.
The simultaneous occurrence of these three symptoms is crucial for clinicians assessing Reiter’s Syndrome. Recognizing this triad aids in timely intervention and treatment strategies tailored to individual needs.
Additional Symptoms: Other Manifestations of Reiter’s Syndrome
Reiter’s Syndrome, while primarily recognized for its classic triad of arthritis, urethritis, and conjunctivitis, can also present a variety of additional symptoms. These manifestations are often overlooked but play an essential role in the overall clinical picture.
Patients may experience skin rashes or lesions. Psoriasis-like patches and painful ulcers can develop on various parts of the body. This adds another layer to the complexity of diagnosis.
“Why Does Zamzam Syndrome Affect Growth?”
Mouth sores are not uncommon either. These can lead to discomfort during eating and speaking, impacting daily life significantly.
Some individuals report gastrointestinal issues such as diarrhea or abdominal pain. This symptomatology further emphasizes that Reiter’s Syndrome affects more than just joints.
Furthermore, fatigue is frequently reported among patients. It can be debilitating and affect quality of life profoundly, revealing how multifaceted this condition truly is.
Diagnostic Criteria: How Reiter’s Syndrome is Identified
Identifying Reiter’s Syndrome involves a combination of clinical evaluation and patient history. Physicians typically look for the presence of the classic triad: arthritis, urethritis, and conjunctivitis. The symptoms usually develop sequentially after an infection.
A thorough medical history can reveal recent infections, especially those related to the genitourinary or gastrointestinal systems. This context is vital in establishing a connection between prior illnesses and current symptoms.
Physical examinations focus on joint swelling or tenderness along with any signs of inflammation in the eyes or urinary tract.
Healthcare providers also consider additional criteria such as HLA-B27 antigen testing. A positive result may suggest a predisposition to this condition but isn’t definitive alone.
Careful assessment helps differentiate Reiter’s from other forms of reactive arthritis, paving the way for accurate diagnosis and treatment planning.
Laboratory Tests: Blood Work and Other Diagnostic Tools
Laboratory tests play a crucial role in diagnosing Reiter’s syndrome. Blood work is often the first step, helping to identify inflammation markers and autoimmune responses. Common tests include erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), which indicate the presence of inflammation.
Additionally, rheumatologic blood panels can help detect specific antibodies associated with reactive arthritis, including HLA-B27 antigen testing. This antigen is present in many individuals with Reiter’s syndrome, although not exclusively.
Urinalysis may also be conducted to check for signs of urethritis or urinary tract infections that could trigger symptoms.
In some cases, synovial fluid analysis from affected joints provides valuable insights into inflammatory processes at play. These comprehensive testing methods collectively aid healthcare providers in confirming a diagnosis and guiding effective treatment strategies tailored to each patient’s needs.
Imaging Studies: X-rays, MRI, and Ultrasound in Diagnosis
Imaging studies play a vital role in diagnosing Reiter’s Syndrome. X-rays are often the first step. They can reveal joint damage and inflammation, helping to assess the condition’s severity.
MRI offers a more detailed view of soft tissues and bones. It can detect early signs of arthritis that might not be visible on X-rays. This tool is especially useful for evaluating spinal involvement or other atypical presentations.
Ultrasound is another valuable diagnostic method. It allows real-time visualization of joints and surrounding structures, highlighting areas of swelling or fluid accumulation.
These imaging techniques complement clinical findings and laboratory results, providing a comprehensive understanding of how Reiter’s Syndrome affects an individual. By using these tools effectively, healthcare providers can tailor treatment strategies based on specific needs and circumstances.
Differential Diagnosis: Distinguishing from Other Arthritic Conditions
Differential diagnosis is crucial for identifying Reiter’s Syndrome. This condition often mimics other forms of arthritis, making accurate assessment essential.
Rheumatoid arthritis (RA) is one alternative that shares symptoms like joint pain and swelling. However, RA typically involves symmetrical joint involvement and specific blood markers not seen in Reiter’s Syndrome.
Another contender is psoriatic arthritis. It can also cause inflammation of the joints but is usually associated with skin lesions. A thorough examination can help distinguish between these conditions.
Gout presents a different challenge as well, characterized by sudden attacks of severe pain in joints due to uric acid crystals. Unlike Reiter’s, gout does not generally involve urethritis or conjunctivitis.
Ankylosing spondylitis may show similar spinal symptoms but tends to have distinct patterns on imaging studies. Understanding these differences helps ensure appropriate treatment and management strategies are applied effectively.
Treatment Approaches: Managing Symptoms and Reducing Inflammation
Effective management of Reiter’s Syndrome involves a multifaceted approach. The primary goal is to alleviate symptoms and reduce inflammation in affected joints.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are often the first line of treatment. They help relieve pain and decrease swelling, allowing for improved mobility.
For more severe cases, disease-modifying antirheumatic drugs (DMARDs) may be employed. These medications target the underlying processes driving inflammation, offering longer-term relief.
Biologic therapies have emerged as an option for patients who do not respond adequately to conventional treatments. They specifically block inflammatory pathways contributing to the condition’s progression.
Physical therapy plays a vital role too. Tailored exercises can enhance flexibility and strengthen surrounding muscles, providing support to inflamed joints while promoting overall well-being.
Regular follow-ups with healthcare providers ensure that treatment remains effective and adjustments can be made as needed. Each patient’s journey is unique, requiring personalized strategies for optimal outcomes.
Medications: NSAIDs, DMARDs, and Biologics in Reiter’s Syndrome
Reiter’s Syndrome often requires a multi-faceted approach to treatment, particularly regarding medication. Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly the first line of defense. They help reduce pain and inflammation effectively.
For those with more severe symptoms or persistent flare-ups, disease-modifying antirheumatic drugs (DMARDs) may be prescribed. These medications work by altering the immune system’s response, helping to prevent joint damage over time.
Biologics represent another advanced category of treatment for Reiter’s Syndrome. Targeting specific pathways in the inflammatory process, these medications can offer significant relief for patients who do not respond well to traditional therapies.
Each patient’s experience is unique; therefore, medical guidance is essential when considering these options. Regular monitoring ensures that treatments remain effective while minimizing potential side effects associated with long-term use.
Prognosis: Long-term Outlook and Recurrence Rates
The prognosis for Reiter’s Syndrome varies significantly among individuals. Many patients experience an initial episode that resolves within a few months, while others may face recurrent symptoms over the years.
Recurrence rates can be influenced by several factors, including underlying health conditions and lifestyle choices. Some studies suggest that up to 50% of individuals may have recurring arthritis after their first flare-up.
Long-term complications are possible but not guaranteed. Chronic joint pain or stiffness may develop in some cases, leading to significant lifestyle changes. Early diagnosis and treatment are crucial in managing these symptoms effectively.
Emotional well-being often intertwines with physical health in those affected. Support from healthcare professionals and communities can play a vital role in enhancing quality of life as patients navigate this chronic condition. Regular monitoring and proactive management strategies remain essential for maintaining functionality over time.
Complications: Potential Long-term Effects of Reiter’s Syndrome
Reiter’s syndrome can lead to several long-term complications that affect various body systems. One notable concern is persistent arthritis, which may evolve into chronic joint pain and stiffness. This can significantly hinder mobility and daily activities.
Additionally, some individuals may experience eye problems beyond conjunctivitis. Uveitis or iritis could develop, leading to vision impairment if not addressed promptly.
Skin issues are also possible; psoriasis-like lesions might appear in conjunction with the condition. These skin manifestations often require specialized treatment.
Moreover, Reiter’s syndrome has been associated with an increased risk of cardiovascular disease. Inflammation plays a critical role here, potentially affecting heart health over time.
Kidney involvement is another complication that may arise in certain cases, requiring careful monitoring and management by healthcare professionals. Understanding these potential effects helps patients prepare for their journey ahead.
Living with Reiter’s Syndrome: Lifestyle Adjustments and Self-Care
Living with Reiter’s Syndrome requires proactive lifestyle adjustments. Managing stress is crucial, as it can exacerbate symptoms. Incorporating relaxation techniques such as meditation or yoga can offer significant relief.
Physical activity plays a vital role in maintaining joint health. Low-impact exercises like swimming or cycling help strengthen muscles without straining the joints. Regular movement also promotes flexibility and reduces stiffness.
Dietary choices impact inflammation levels. A diet rich in omega-3 fatty acids, fruits, and vegetables may alleviate symptoms. Staying hydrated is equally important for overall health.
Self-care routines are essential too. Prioritizing sleep and establishing a consistent schedule can improve energy levels and mood. Developing a support network of friends, family, or online communities fosters connection while sharing experiences helps combat feelings of isolation.
Monitoring symptoms closely allows for timely intervention when flare-ups occur, ensuring better management of this condition day by day.
Dietary Considerations: Nutrition and Its Impact on Symptoms
Diet plays a crucial role in managing Reiter’s Syndrome symptoms. Certain foods can help reduce inflammation, while others may exacerbate discomfort.
Incorporating omega-3 fatty acids found in fish like salmon and sardines can be beneficial. These healthy fats promote joint health and may alleviate pain.
Fruits and vegetables are also vital for their antioxidants, which combat oxidative stress in the body. Berries, leafy greens, and citrus fruits are excellent choices.
On the flip side, some individuals may find that processed foods or those high in sugars worsen their symptoms. Gluten sensitivity can also play a part; thus, monitoring your diet for reactions is wise.
Hydration is essential too—staying well-hydrated supports overall bodily functions and helps maintain joint lubrication. Making these dietary adjustments could lead to noticeable improvements over time.
Exercise and Physical Therapy: Maintaining Joint Health
Regular exercise is vital for individuals with Reiter’s Syndrome. It helps maintain joint flexibility and muscle strength, which can alleviate pain and improve mobility.
Physical therapy plays a critical role in managing symptoms. A trained therapist can design personalized programs that focus on stretching, strengthening, and low-impact aerobic activities. This tailored approach enhances overall function while minimizing stress on affected joints.
Low-impact exercises such as swimming or cycling are particularly beneficial. They provide cardiovascular benefits without putting excessive strain on inflamed joints.
Incorporating daily routines like walking or gentle yoga can also aid in maintaining physical health. Consistency is key; even short sessions can lead to significant improvements over time.
Staying active not only supports physical well-being but also boosts mental health. Engaging in regular movement fosters a sense of control over the condition, empowering patients to manage their symptoms more effectively.
Psychological Impact: Mental Health Support for Patients
Living with Reiter’s Syndrome can take a toll on mental health. The chronic pain and unpredictable flare-ups often lead to feelings of frustration, anxiety, or depression.
Patients may experience social isolation as activities they once enjoyed become difficult. This shift can strain relationships with friends and family, further compounding emotional distress.
Mental health support is crucial for those affected by this condition. Therapy options like cognitive-behavioral therapy (CBT) can help individuals develop coping strategies. Support groups also provide a platform for sharing experiences and building connections with others facing similar challenges.
Encouraging open conversations about mental well-being is vital. It fosters an environment where patients feel safe discussing their struggles without fear of judgment. Integrating mental health care into treatment plans ensures a holistic approach to managing Reiter’s Syndrome effectively.
Research Developments: Current Studies and Future Treatments
Research developments in Reiter’s Syndrome, also known as reactive arthritis, are ongoing and aim to improve the understanding of this complex condition. Studies currently focus on identifying specific triggers and genetic factors that may predispose individuals to develop this syndrome after infection.
One promising area of research involves the role of microbiomes in triggering inflammatory responses. Scientists are exploring how gut health can influence autoimmune conditions like Reiter’s Syndrome. By examining the relationship between bacteria in our bodies and joint inflammation, researchers hope to uncover new treatment pathways.
In addition to studying underlying causes, clinical trials are assessing novel medications aimed at managing symptoms more effectively. Biologics have shown potential for those who do not respond well to traditional treatments such as NSAIDs or DMARDs. These targeted therapies could offer relief by specifically addressing inflammatory processes without broad immunosuppression.
Furthermore, there’s a growing interest in personalized medicine approaches that consider individual patient profiles when determining treatment plans. This could lead to tailored therapies based on genetic makeup or specific disease manifestations.
As research continues, the future looks promising for those affected by Reiter’s Syndrome. Advances might not only enhance symptom management but also provide insights into prevention strategies, improving quality of life for patients globally. Ongoing studies will be pivotal in shaping effective therapeutic options moving forward.

