Dejerine–Roussy Syndrome, often overshadowed by its more common neurological counterparts, presents a unique set of challenges for those affected. This rare condition results from specific damage to the thalamus and can lead to a cocktail of symptoms that impact daily life in profound ways. Understanding this syndrome is crucial not only for patients but also for caregivers and healthcare professionals.
As we delve deeper into Dejerine–Roussy Syndrome, we’ll explore its causes, symptoms, diagnosis methods, treatment options, and what it truly means to live with this complex disorder. Whether you’re seeking knowledge for yourself or someone close to you, this guide aims to shed light on the neurological impact of Dejerine–Roussy Syndrome and pave the way toward better management strategies. Let’s uncover the intricacies behind this enigmatic condition together!
Understanding Dejerine–Roussy Syndrome
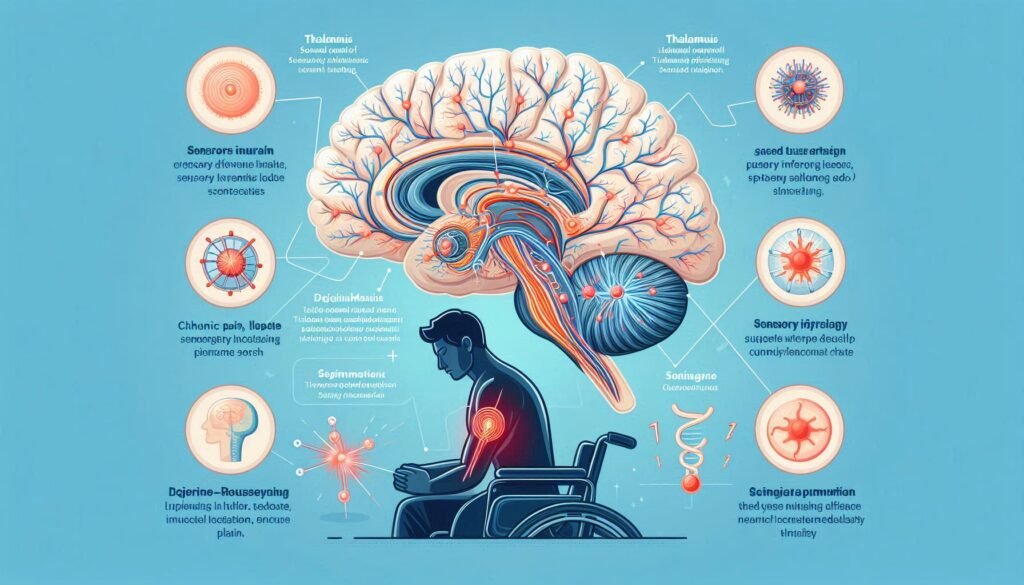
Dejerine–Roussy Syndrome is a neurological disorder characterized by a range of sensory and motor symptoms. This condition arises due to damage in the thalamus, an important brain region that processes sensory information.
Often referred to as central post-stroke pain syndrome, it can follow a stroke or other types of brain injury. The condition primarily affects how sensations are perceived, leading to unusual feelings such as numbness or burning pain.
“Why Does Gardner Syndrome Cause Multiple Tumors?”
First identified in the early 20th century by French neurologists Joseph Dejerine and André Roussy, its historical context adds depth to our understanding today. Those diagnosed with this syndrome often face significant challenges due to its complex interplay between physical sensation and emotional well-being. Understanding these aspects helps pave the way for better treatment options and support systems tailored for individuals affected by Dejerine–Roussy Syndrome.
Dejerine–Roussy Syndrome Definition and Alternate Names
Dejerine–Roussy Syndrome is a neurological disorder characterized by complex symptoms resulting from damage to the thalamus. This condition often arises following a stroke, particularly in the posterior circulation of the brain.
The syndrome is also known as central post-stroke pain (CPSP). This name highlights one of its most distressing aspects: chronic pain that occurs despite no direct injury to peripheral nerves.
“How Does Genitopatellar Syndrome Affect Development?”
Additionally, it may be referred to as thalamic pain syndrome due to its association with lesions in the thalamus. Understanding these alternative names can facilitate better communication among healthcare providers and patients alike.
Each term reflects different facets of this multifaceted disorder, underscoring its impact on both sensory processing and emotional well-being.
Historical Context and Discovery
Dejerine–Roussy Syndrome was first identified in the early 20th century. French neurologists Joseph Jules Dejerine and André Roussy were instrumental in its discovery. Their work focused on patients who exhibited unusual sensory disturbances following a thalamic stroke.
“What Triggers Guillain-Barré Syndrome? Recovery Guide”
The syndrome emerged from observations made during autopsies, revealing lesions in the thalamus associated with specific symptoms. This highlighted the importance of this brain region in processing sensory information.
As research progressed, medical professionals began to connect these findings with clinical manifestations seen in living patients. The understanding of how thalamic damage could lead to pain and sensory anomalies expanded significantly during this period.
This historical context laid the groundwork for further exploration into neurological disorders linked to vascular events, paving the way for modern approaches to diagnosis and treatment.
Causes of Dejerine–Roussy Syndrome
Dejerine–Roussy Syndrome primarily stems from lesions in the thalamus, a crucial brain region that processes sensory information. These lesions disrupt normal sensory pathways, leading to characteristic symptoms.
One of the most common causes is stroke. When an ischemic or hemorrhagic event affects blood flow to the thalamus, it can result in lasting damage and subsequent pain syndromes.
“Why Does Ganser Syndrome Cause False Answers?”
Other potential causes include traumatic brain injuries and multiple sclerosis. In rare instances, infections or tumors affecting the thalamic area may contribute to developing this syndrome.
Understanding these underlying factors is vital for effective management and treatment planning for individuals diagnosed with Dejerine–Roussy Syndrome.
Thalamic Lesions
Thalamic lesions are often central to understanding Dejerine–Roussy Syndrome. These lesions occur in the thalamus, a crucial brain region that acts as a relay station for sensory and motor signals.
When damage occurs here, it disrupts normal communication pathways between the body and the brain. This can lead to various neurological symptoms characteristic of the syndrome.
“How Does Gaucher’s Syndrome Affect Metabolism?”
The location and extent of these lesions significantly influence the severity and type of symptoms experienced. Patients may encounter a range of issues from pain to sensory disturbances.
Research indicates that stroke is one common cause leading to thalamic lesions. However, other factors like tumors or infections can also play a role.
Understanding how these lesions affect overall brain function is vital for developing effective treatment strategies for those affected by this complex condition.
Stroke as a Primary Cause
Stroke is the most prevalent cause of Dejerine–Roussy Syndrome. It often leads to significant damage in specific brain areas, particularly the thalamus. This region plays a crucial role in processing sensory information.
When a stroke occurs, blood flow to the brain is disrupted. The resulting ischemia can cause neuronal death and lead to various neurological deficits. Patients may experience different severity levels depending on how extensive the damage is.
“What Is Gerstmann Syndrome? Brain Function Guide”
The pain associated with this syndrome typically arises after a stroke event, manifesting as central post-stroke pain (CPSP). Those affected might also encounter altered sensations like burning or tingling.
Understanding that strokes are primary triggers helps healthcare providers tailor rehabilitation plans effectively. Early intervention remains vital for managing symptoms and improving quality of life for individuals facing this challenging condition.
Other Potential Causes
Dejerine–Roussy Syndrome can arise from various less common factors. Beyond strokes, other potential causes warrant attention.
Traumatic brain injuries may contribute to the development of this syndrome. Damage to critical areas of the brain can disrupt sensory pathways and lead to symptoms typical of Dejerine–Roussy.
“Why Does Harlequin Syndrome Affect Sweating? Expert Guide”
Multiple sclerosis is another condition linked with thalamic lesions. The demyelination process in MS can directly affect how sensory information is processed, resulting in pain and disturbances.
Tumors or structural abnormalities within the thalamus might also play a role. These growths can exert pressure on surrounding neural tissue, leading to dysfunction similar to what’s seen in stroke patients.
Additionally, infectious processes like encephalitis have been reported as triggers for neurological syndromes. Inflammation caused by infections could disrupt normal brain function significantly.
Dejerine–Roussy Syndrome Symptoms and Clinical Manifestations
Dejerine–Roussy Syndrome primarily manifests through central post-stroke pain. This debilitating condition often follows a stroke, leading to intense and chronic pain sensations that can be challenging to manage.
Sensory disturbances are also common, with patients experiencing altered sensations such as tingling or numbness in various parts of the body. These symptoms can significantly impact daily activities.
Motor impairments frequently accompany these sensory issues, affecting coordination and strength. Individuals may struggle with basic movements, which can lead to frustration and decreased independence.
Additionally, emotional and psychological effects cannot be overlooked. Many patients grapple with anxiety or depression linked to their physical limitations. The interplay of these symptoms creates a complex clinical picture requiring comprehensive management strategies tailored for each individual’s needs.
Central Post-Stroke Pain
Central post-stroke pain (CPSP) is a challenging condition that can arise after a stroke, particularly in individuals with Dejerine–Roussy Syndrome. The pain originates from damage to the brain’s thalamus, which plays a crucial role in processing sensory information.
Patients often report sensations of burning, tingling, or sharp pains that may affect one side of the body. These symptoms can be debilitating and significantly impair daily activities. The unpredictability of the pain adds another layer of complexity for those living with CPSP.
Management strategies focus on alleviating discomfort through various methods. This includes medication options like anticonvulsants and antidepressants tailored to address nerve-related pain signals. Additionally, physical therapy can help improve mobility and reduce sensitivity over time.
Understanding how central post-stroke pain manifests is essential for effective treatment and support for affected individuals. Each case varies widely based on individual experiences and underlying factors related to their stroke type.
Sensory Disturbances
Sensory disturbances are a hallmark of Dejerine–Roussy Syndrome. Individuals often experience altered sensations, such as numbness or tingling in various body parts. This can lead to profound discomfort and distress.
Affected patients may report an inability to feel touch, temperature changes, or pain normally. These disruptions stem from damage to the thalamus, which plays a critical role in processing sensory information.
The condition can also produce phenomena like allodynia—where normal stimuli become painful. For example, light touches may evoke sharp discomfort instead of relief.
Such symptoms not only impact daily activities but also contribute to emotional struggles. The unpredictability of these sensory experiences can make navigating life challenging for those affected by this syndrome. Understanding these disturbances is crucial for developing appropriate coping strategies and treatment plans tailored to individual needs.
Motor Impairments due to Dejerine–Roussy Syndrome
Motor impairments in Dejerine–Roussy Syndrome can significantly affect daily functioning. Patients often experience weakness or paralysis on one side of the body, known as hemiparesis. This occurs due to disruptions in the brain’s communication pathways following thalamic damage.
Coordination issues are also common. Individuals may struggle with fine motor skills, making tasks like buttoning a shirt or writing difficult. These challenges stem from altered sensory feedback and proprioception, impacting overall movement control.
Additionally, muscle tone abnormalities can develop, leading to stiffness or spasticity in affected limbs. This further complicates mobility and contributes to discomfort during movement.
Rehabilitation plays a crucial role in addressing these motor difficulties. Personalized therapy programs can help enhance strength and coordination over time. Engaging healthcare professionals focused on tailored rehabilitation strategies is essential for improving quality of life amidst these challenges.
Emotional and Psychological Effects
Dejerine–Roussy Syndrome can profoundly impact emotional and psychological well-being. Individuals may experience a range of feelings, including anxiety and depression. The constant pain and sensory disturbances often lead to frustration, creating a cycle of emotional distress.
Social isolation is another concern. Patients might withdraw from activities they once enjoyed due to fear or discomfort, which can exacerbate feelings of loneliness. This disconnection not only affects mental health but also hampers overall recovery.
Coping with chronic pain further complicates emotional stability. Many find it hard to express their experiences, leading to misunderstandings in relationships with family and friends.
Therapeutic interventions are essential for addressing these issues. Psychotherapy can provide tools for managing emotions effectively while building support networks helps individuals feel less alone in their struggles. Emotional resilience plays a critical role in the journey toward better health amidst Dejerine–Roussy Syndrome challenges.
Diagnosis of Dejerine–Roussy Syndrome
Diagnosing Dejerine–Roussy Syndrome involves a thorough clinical evaluation. Physicians assess the patient’s medical history and perform a detailed neurological examination. This process helps identify specific symptoms related to the syndrome.
Neuroimaging techniques play a vital role in diagnosis. MRI scans are particularly useful for visualizing thalamic lesions, which are characteristic of this condition. These imaging results assist doctors in confirming their suspicions based on clinical findings.
Differential diagnosis is essential as other conditions may present similar symptoms, such as neuropathic pain or stroke-related complications. Healthcare providers must rule out these alternatives to ensure an accurate diagnosis of Dejerine–Roussy Syndrome.
Timely and precise identification can lead to better management strategies tailored specifically for affected individuals, underscoring the importance of expertise in neurology during this process.
Clinical Evaluation
Clinical evaluation is a critical step in diagnosing Dejerine–Roussy Syndrome. It begins with a thorough patient history, focusing on symptoms and their onset. This information helps healthcare providers understand the impact of the syndrome on daily life.
Neurological examinations are essential during this process. Doctors assess sensory responses, motor functions, and pain levels to gauge the extent of neurological impairment. Observing how patients respond to stimuli can reveal underlying thalamic lesions.
Additionally, clinicians often seek input from family members to gain further insights into changes in behavior or cognition that may have occurred post-stroke. The combination of objective assessments and subjective reports provides a comprehensive view of the patient’s condition.
This multifaceted approach aids in distinguishing Dejerine–Roussy Syndrome from other disorders that present similar symptoms, ensuring an accurate diagnosis and tailored treatment plan.
Neuroimaging Techniques
Neuroimaging techniques play a critical role in diagnosing Dejerine–Roussy Syndrome. These advanced methods allow physicians to visualize the brain’s structure and activity, helping to identify specific abnormalities.
Magnetic Resonance Imaging (MRI) is commonly employed. It provides detailed images of the thalamus, where lesions often occur in this syndrome. This imaging helps clinicians confirm damage associated with prior strokes or other neurological conditions.
Computed Tomography (CT) scans are also useful, particularly in emergency settings. They can quickly detect acute changes that may indicate stroke-related injuries.
Functional MRI (fMRI) adds another layer by assessing brain activity through blood flow changes. This technique can help evaluate how different areas of the brain respond during sensory tasks.
Together, these neuroimaging modalities offer valuable insights into the complexities of Dejerine–Roussy Syndrome and aid in effective treatment planning.
Differential Diagnosis of Dejerine–Roussy Syndrome
Differential diagnosis is crucial for accurately identifying Dejerine–Roussy Syndrome. This condition can easily be mistaken for other neurological disorders due to overlapping symptoms.
Conditions such as complex regional pain syndrome (CRPS) should be considered. CRPS involves severe pain and sensory abnormalities, resembling the central post-stroke pain seen in Dejerine–Roussy Syndrome.
Multiple sclerosis (MS) may also present similar sensory disturbances. Physicians must differentiate between these two conditions based on clinical history and symptom progression.
Additionally, peripheral neuropathy could mimic some aspects of Dejerine–Roussy Syndrome. A thorough patient evaluation is essential to pinpoint the true cause of symptoms.
Accurate differential diagnosis ensures appropriate treatment strategies are implemented, fostering better health outcomes for those affected by this challenging syndrome.
Dejerine–Roussy Syndrome Treatment Approaches
Managing Dejerine–Roussy Syndrome can be complex, as it often involves a combination of treatment approaches. Pain management is essential for improving the quality of life. Patients may benefit from various strategies, including medication and alternative therapies.
Pharmacological interventions typically include analgesics and anticonvulsants to help alleviate pain symptoms. Doctors sometimes prescribe antidepressants that can also reduce chronic pain perception.
Non-pharmacological therapies are increasingly recognized for their benefits. Physical therapy helps in restoring motor function and strengthening muscles. Occupational therapy focuses on daily activities to enhance independence.
Neurostimulation techniques, such as transcutaneous electrical nerve stimulation (TENS) or spinal cord stimulation, show promise in managing neuropathic pain effectively. Each treatment plan should be tailored to individual patient needs for optimum results in coping with the syndrome’s challenges.
Pain Management Strategies
Pain management for Dejerine–Roussy Syndrome requires a multifaceted approach. Effective strategies often blend medication and alternative therapies.
Medications like anticonvulsants and antidepressants can alleviate central post-stroke pain. These drugs help modify pain perception, providing some relief to patients struggling with discomfort.
Physical therapy plays a crucial role as well. Tailored exercise programs enhance mobility while reducing stiffness in affected areas. Techniques such as stretching and strength training contribute positively to overall function.
Cognitive-behavioral therapy is another valuable tool. This psychological approach helps individuals develop coping mechanisms for their chronic pain experience, improving emotional resilience.
Complementary methods like acupuncture or massage therapy may offer additional benefits. These therapies promote relaxation and improve blood circulation, potentially easing tension associated with the syndrome’s symptoms.
Pharmacological Interventions
Pharmacological interventions play a crucial role in managing symptoms associated with Dejerine–Roussy Syndrome. Medications are often tailored to address specific issues such as pain, sensory disturbances, and mood disorders.
Anticonvulsants like gabapentin and pregabalin are commonly prescribed for neuropathic pain relief. These medications can help modulate nerve signals that contribute to discomfort.
Opioids may be considered for severe cases but require careful monitoring due to their addictive nature. Non-steroidal anti-inflammatory drugs (NSAIDs) can also offer some relief from pain without the same risks.
Additionally, antidepressants such as amitriptyline or duloxetine have shown efficacy in alleviating chronic pain while improving emotional well-being. Their dual action makes them particularly useful for patients suffering from both physical and psychological symptoms.
It’s essential for healthcare providers to regularly evaluate treatment effectiveness and make adjustments based on individual patient responses.
Non-pharmacological Therapies
Non-pharmacological therapies offer valuable options for managing Dejerine–Roussy Syndrome symptoms. These approaches prioritize holistic care and focus on enhancing the quality of life.
Physical therapy plays a crucial role in rehabilitation. Tailored exercises can help improve mobility and strengthen muscles affected by motor impairments. Occupational therapy also aids individuals in adapting daily activities, promoting independence.
Additionally, cognitive-behavioral therapy (CBT) targets emotional challenges linked to chronic pain. It equips patients with coping strategies and promotes resilience against psychological distress.
Mindfulness practices, such as meditation or yoga, can significantly reduce stress levels. They cultivate awareness of body sensations and enhance emotional regulation.
Support groups provide a platform for sharing experiences and fostering connections among those facing similar challenges. This sense of community can be invaluable in navigating the complexities of living with Dejerine–Roussy Syndrome.
Neurostimulation Techniques
Neurostimulation techniques have emerged as promising interventions for managing the symptoms of Dejerine–Roussy Syndrome. These methods aim to modulate neural activity, helping alleviate chronic pain and sensory disturbances.
Transcranial magnetic stimulation (TMS) is one such technique. It uses magnetic fields to stimulate nerve cells in the brain. TMS can help improve mood and reduce pain perception, offering a non-invasive option for patients.
Another promising approach is spinal cord stimulation (SCS). This method involves implanting a device that sends electrical impulses to the spinal cord. Patients often report significant reductions in pain intensity after SCS treatment.
Peripheral nerve stimulation (PNS) targets specific nerves associated with pain pathways. By delivering small bursts of electricity, PNS can disrupt abnormal signals, providing relief from discomfort.
These neurostimulation options represent exciting advancements in treating Dejerine–Roussy Syndrome and enhancing patient quality of life.
Living with Dejerine–Roussy Syndrome
Living with Dejerine–Roussy Syndrome can present unique challenges. Coping strategies often become essential for managing daily life. Many find support groups beneficial, as sharing experiences fosters understanding and connection.
Lifestyle adjustments play a crucial role in maintaining well-being. Adopting a balanced diet and engaging in gentle exercises can enhance physical health. Mindfulness practices, such as meditation or yoga, may alleviate stress levels.
Establishing routines helps create stability amidst uncertainty. Incorporating relaxation techniques into daily activities promotes emotional resilience.
Furthermore, open communication with healthcare providers is vital for tailoring treatment plans to individual needs. Managing symptoms effectively enhances quality of life significantly.
Building a supportive network of family and friends provides encouragement during tough times. Open discussions about feelings can foster deeper connections while addressing the psychological aspects of living with this syndrome.
Coping Strategies
Coping with Dejerine–Roussy Syndrome can be challenging, but various strategies can help enhance daily living. Mindfulness practices, such as meditation and deep-breathing exercises, are effective for reducing stress and managing pain perception.
Participating in support groups connects patients with others who understand their experiences. Sharing stories fosters a sense of community and provides emotional relief.
Implementing structured routines assists in creating predictability, which may alleviate feelings of anxiety. Setting realistic goals each day encourages a sense of accomplishment despite the challenges posed by the syndrome.
Engaging in light physical activity promotes both mental well-being and physical health. Simple stretching or gentle yoga can improve mobility while also serving to distract from discomfort.
Seeking therapy can be beneficial for navigating the emotional aspects associated with this condition. Professional guidance offers tools for coping with grief, frustration, or depression that may arise during the journey.
Lifestyle Adjustments
Living with Dejerine–Roussy Syndrome often requires significant lifestyle adjustments. These changes can help manage symptoms and improve overall well-being.
One crucial adjustment is the incorporation of a structured daily routine. Having consistent activities can provide a sense of normalcy and stability, which may alleviate anxiety related to unpredictable symptoms.
Diet plays an essential role as well. A balanced diet rich in anti-inflammatory foods might help mitigate some discomfort associated with this syndrome. Hydration should not be overlooked; staying properly hydrated can aid in maintaining energy levels.
Adaptive devices also enhance quality of life for individuals facing mobility challenges or sensory issues. Simple tools like grip aids or specialized utensils allow for greater independence during daily tasks.
Engaging in low-impact exercises such as yoga or swimming promotes physical health while offering mental relaxation—a vital component when coping with chronic pain and emotional fluctuations.
Dejerine–Roussy Syndrome Prognosis and Long-term Outlook
The prognosis for individuals with Dejerine–Roussy Syndrome varies widely. Factors such as the extent of brain damage and individual health play a crucial role in recovery.
Many patients experience fluctuating symptoms, particularly persistent pain. Understanding these patterns can aid in managing expectations and developing coping strategies.
Chronic pain often requires multidisciplinary approaches to treatment. Engaging healthcare providers skilled in pain management can significantly improve quality of life.
Rehabilitation also focuses on enhancing functional independence. Physical therapy tailored to individual needs fosters neuroplasticity, allowing some patients to regain lost skills over time.
Emotional wellbeing is equally important, as psychological effects may linger long after other symptoms have stabilized. Support groups or counseling can provide valuable resources for emotional resilience amidst ongoing challenges associated with this syndrome.
Recovery Patterns
Recovery patterns in Dejerine–Roussy Syndrome can vary significantly among individuals. Some patients experience gradual improvements over time, while others may face persistent challenges.
Early intervention plays a crucial role in influencing recovery outcomes. Engaging with rehabilitation services soon after diagnosis can enhance the likelihood of regaining lost functions and alleviating symptoms.
Neuroplasticity is another important factor. The brain’s ability to reorganize itself allows for compensation for damaged areas, enabling some patients to adapt and improve their quality of life.
However, many people report fluctuations in their symptoms. Pain may worsen during stressful periods or after physical exertion, highlighting the need for ongoing management strategies tailored to individual experiences.
Regular assessments are essential to track progress and adjust treatment plans effectively. Each patient’s journey is unique as they navigate through this complex syndrome.
Chronic Pain Management
Chronic pain management for Dejerine–Roussy Syndrome is a multifaceted approach. Patients often experience persistent discomfort due to thalamic damage, leading to complex challenges.
One effective strategy involves the use of medications tailored to individual needs. Antidepressants and anticonvulsants are commonly prescribed. They can help alleviate neuropathic pain signals.
Physical therapy also plays an essential role in managing symptoms. Targeted exercises can enhance mobility and reduce stiffness while providing patients with coping techniques.
Mindfulness practices like meditation or yoga have gained popularity as complementary therapies. These methods encourage relaxation and emotional resilience, helping individuals deal with pain more effectively.
Additionally, support groups offer invaluable resources for sharing experiences and strategies among peers facing similar struggles. Building connections fosters a sense of community that may ease feelings of isolation often associated with chronic conditions.
Quality of Life Considerations
Quality of life for individuals with Dejerine–Roussy Syndrome can be significantly impacted by the condition’s symptoms. Chronic pain, sensory disturbances, and emotional challenges often lead to a diminished sense of well-being.
Social interactions may also suffer due to these limitations. Individuals might withdraw from activities they once enjoyed or find it difficult to engage with others. This isolation can exacerbate feelings of anxiety and depression.
Support networks play a crucial role in maintaining quality of life. Family members, friends, and support groups can provide much-needed encouragement and understanding.
Additionally, focusing on holistic approaches such as mindfulness practices or gentle physical activity may improve overall well-being. These strategies help manage symptoms while fostering a sense of accomplishment and connection with others.
Adapting daily routines to accommodate individual needs is essential for enhancing quality of life amidst the challenges posed by this syndrome.
Research and Advancements
Current research on Dejerine–Roussy Syndrome is focused on understanding its complex mechanisms. Scientists are exploring how thalamic lesions contribute to the neurological symptoms experienced by patients.
Emerging treatments aim to alleviate chronic pain and improve sensory functions. Some studies investigate novel pharmacological approaches that target specific pathways involved in pain perception.
Neuroplasticity has become a crucial area of interest. Researchers are looking at rehabilitation methods that harness the brain’s ability to reorganize itself after injury. This can potentially lead to improved recovery outcomes for those affected by this syndrome.
Additionally, ongoing trials assess various neurostimulation techniques, such as transcranial magnetic stimulation (TMS). These innovations may offer new hope for managing symptoms while enhancing overall quality of life for individuals living with Dejerine–Roussy Syndrome.
Current Studies
Current studies on Dejerine–Roussy Syndrome are focusing on understanding its underlying mechanisms. Researchers are examining the specific thalamic lesions that contribute to symptoms. This research aims to clarify how injury impacts sensory processing.
Clinical trials are exploring new pharmacological interventions targeting pain relief and symptom management. These include assessing medications that modulate neurotransmitter levels in the brain, potentially improving quality of life for patients.
Additionally, some studies investigate neuroplasticity—the brain’s ability to reorganize itself after an injury. By fostering rehabilitation techniques designed around this concept, researchers hope to enhance recovery rates and functional outcomes.
Efforts also extend into genetics, looking for biomarkers that could help identify those at risk for developing the syndrome post-stroke or other neurological events. Understanding these factors may pave the way for earlier interventions and personalized treatment plans tailored specifically for individuals with Dejerine–Roussy Syndrome.
Emerging Treatments
Emerging treatments for Dejerine–Roussy Syndrome are gaining traction in the medical community. Researchers are exploring innovative approaches to manage symptoms effectively.
One promising area is gene therapy, which aims to target specific pathways involved in pain perception and sensory processing. This could potentially reduce the chronic pain experienced by many patients.
Another exciting development involves neuromodulation techniques. These methods use electrical impulses to alter nerve activity, offering relief from persistent discomfort without heavy reliance on medications.
Additionally, advances in virtual reality (VR) rehabilitation show potential benefits. VR can create immersive environments for physical and cognitive exercises, aiding recovery while engaging patients more fully during therapy sessions.
Ongoing studies into plant-based compounds suggest they may provide alternative avenues for pain management. As research progresses, these emerging treatments hold promise for improving quality of life for individuals living with Dejerine–Roussy Syndrome.
Neuroplasticity and Rehabilitation
Neuroplasticity refers to the brain’s remarkable ability to reorganize itself by forming new neural connections throughout life. This adaptability plays a crucial role in rehabilitation for individuals living with Dejerine–Roussy Syndrome. Understanding how neuroplasticity works can empower patients and caregivers alike.
Rehabilitation programs often focus on harnessing this capacity for change. Techniques such as repetitive task practice and constraint-induced movement therapy aim to stimulate areas of the brain affected by thalamic lesions. These approaches encourage the brain to rewire itself, promoting better function in daily activities.
Emerging research shows promise in combining traditional therapies with innovative practices like virtual reality and robotics. These technologies create engaging environments that challenge patients physically and cognitively, fostering greater recovery potential.
As studies continue exploring neuroplasticity’s impact on recovery from Dejerine–Roussy Syndrome, it becomes clear that each patient’s journey is unique. Personalized rehabilitation plans tailored to individual needs may lead not only to symptom relief but also improvements in overall quality of life.
Staying informed about advancements in neuroplasticity can inspire hope among those affected by this complex syndrome, highlighting that progress is possible even amid challenges. Embracing these insights encourages ongoing engagement with treatment options while paving a path toward more fulfilling lives despite the hurdles posed by Dejerine–Roussy Syndrome.


