Felty’s Syndrome is an uncommon but significant condition that can greatly impact the lives of those affected. This complex autoimmune disorder, often linked with rheumatoid arthritis, poses unique challenges and complications for patients. Understanding Felty’s Syndrome is crucial not just for medical professionals but also for individuals navigating this diagnosis.
By shedding light on its symptoms, treatment options, and lifestyle considerations, we aim to empower patients and their families with knowledge about this intricate disease. Whether you are seeking information for yourself or a loved one, dive into our comprehensive exploration of Felty’s Syndrome and discover how it influences quality of life.
Understanding Felty’s Syndrome
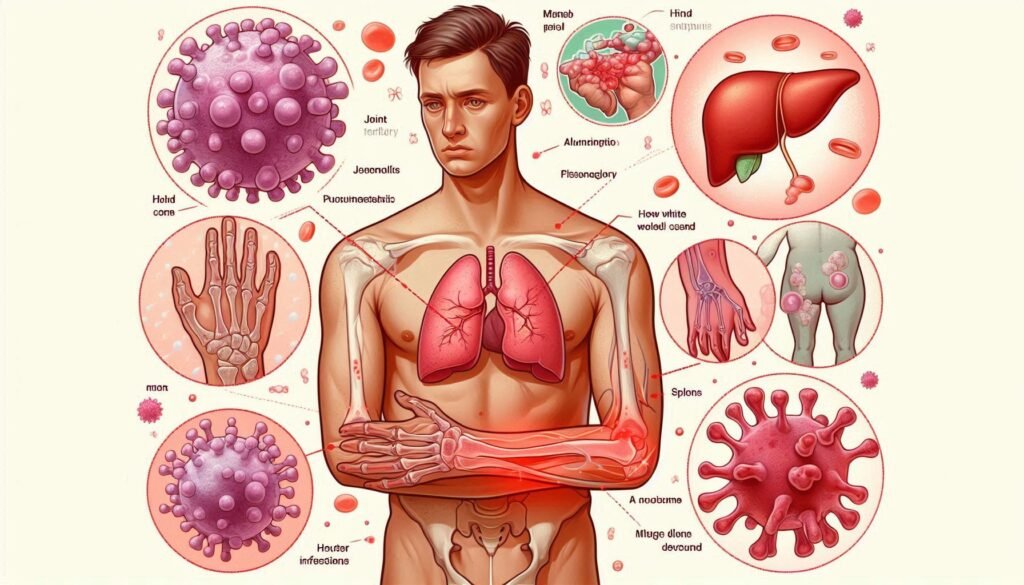
Felty’s Syndrome is a rare autoimmune disorder characterized by the triad of rheumatoid arthritis, neutropenia, and splenomegaly. This condition primarily affects individuals with longstanding rheumatoid arthritis, often leading to severe complications.
The syndrome was first described in the 1920s and has since been recognized as a significant manifestation of rheumatoid disease. Patients may experience frequent infections due to low white blood cell counts resulting from neutropenia.
“What Triggers Primary Raynaud’s Syndrome? Complete Guide”
Splenomegaly, or an enlarged spleen, is another hallmark of Felty’s Syndrome. This enlargement can lead to further immune dysfunction and complicate patient management.
Awareness of this syndrome is essential for early diagnosis and effective treatment strategies. Understanding its complexities helps patients better navigate their healthcare journeys while improving overall quality of life.
Felty’s Syndrome Definition and Overview
Felty’s Syndrome is a rare autoimmune disorder that typically occurs in individuals with rheumatoid arthritis. It is characterized by a triad of symptoms: neutropenia, splenomegaly, and recurrent infections.
Neutropenia refers to an abnormally low level of neutrophils, the white blood cells essential for fighting off infections. This condition significantly increases susceptibility to bacterial and fungal infections.
“How Does PTSD Affect Mental Health? Recovery Guide”
Splenomegaly indicates an enlarged spleen, which can lead to various complications including abdominal discomfort and further immune system dysfunction. The interplay between these symptoms creates unique challenges for those affected.
Patients may experience significant impacts on their daily lives due to the persistent health issues associated with Felty’s Syndrome. Understanding this complex condition is crucial for effective management and improved quality of life.
Historical Context and Discovery
Felty’s Syndrome was first described in the 1920s by Dr. George Felty, an American physician. He identified a unique combination of symptoms linked to rheumatoid arthritis (RA), splenomegaly, and neutropenia.
“What Is Qazi Syndrome? Understanding Rare Genetic Conditions”
Initially, it wasn’t well understood or widely recognized among medical professionals. The syndrome remained obscure for decades despite its impact on affected individuals’ health.
As research progressed through the mid-20th century, more physicians began documenting cases that aligned with Felty’s observations. Attention grew towards this rare condition as clinicians noticed its association with severe manifestations of RA.
This increased awareness led to further studies aimed at understanding the underlying mechanisms and clinical implications of Felty’s Syndrome. Today, it is acknowledged as a serious complication of rheumatoid arthritis requiring comprehensive management strategies tailored to each patient’s needs.
Epidemiology of Felty’s Syndrome
Felty’s Syndrome is a relatively rare condition, primarily affecting individuals with rheumatoid arthritis. Its prevalence remains unclear due to the limited number of studies specifically targeting this syndrome.
Research suggests that Felty’s Syndrome occurs in approximately 1% to 3% of patients diagnosed with rheumatoid arthritis. This indicates that while it is not common, those already living with RA should be aware of its potential development.
“Why Does Quebec Platelet Disorder Affect Blood Clotting?”
Demographic patterns indicate that Felty’s Syndrome tends to affect middle-aged women more frequently than men. Age and gender play significant roles in understanding who might be at risk for this condition.
Several risk factors have been identified as well, including long-standing rheumatoid arthritis and genetic predisposition. These insights into epidemiology can help clinicians monitor patients closely for signs and symptoms associated with Felty’s Syndrome.
Prevalence and Incidence
Felty’s Syndrome is relatively rare, with estimates suggesting it affects approximately 1-3% of individuals diagnosed with rheumatoid arthritis. This underscores its classification as an uncommon complication associated with this autoimmune disorder.
The incidence rates vary based on geographic location and population demographics. In some studies, the condition has shown a higher prevalence among older adults, particularly those in their 50s and 60s.
“How Does Quincke’s Edema Syndrome Cause Swelling?”
While more research is needed to ascertain exact figures globally, it’s clear that Felty’s Syndrome tends to occur more frequently in populations already burdened by rheumatoid arthritis. This highlights the importance of monitoring patients for potential complications like Felty’s as they navigate their treatment journey.
Awareness of these statistics can aid healthcare professionals in identifying at-risk individuals early on, facilitating timely intervention and management strategies tailored to improve patient outcomes.
Demographic Patterns
Demographic patterns of Felty’s Syndrome reveal important insights into its prevalence across various populations. This condition primarily affects individuals with rheumatoid arthritis, which is more common in women than men.
Age is another significant factor; most cases are diagnosed in middle-aged adults typically between the ages of 40 and 60. However, it can occur outside this range as well.
“What Causes Qigong-Induced Psychotic Syndrome?”
Geographically, Felty’s Syndrome appears to have a higher incidence in Caucasian populations compared to other ethnic groups. This may suggest genetic or environmental factors at play.
Understanding these demographic trends helps healthcare providers identify patients who might be at risk and tailor treatment plans accordingly. Awareness of such patterns aids not only in diagnosis but also in developing targeted prevention strategies for those affected by this complex syndrome.
Risk Factors
Felty’s Syndrome primarily affects individuals with rheumatoid arthritis. The presence of this autoimmune condition significantly raises the risk of developing Felty’s Syndrome.
Genetic predisposition plays a role as well. People with family histories of autoimmune diseases may have an increased likelihood of experiencing this syndrome.
Age is another contributing factor. Felty’s Syndrome typically arises in middle-aged adults, particularly those over 50.
Gender also influences risk; it occurs more frequently in women than men. This gender disparity highlights possible hormonal or genetic factors at play.
Environmental triggers, such as infections and exposure to certain chemicals, might contribute to disease onset too. These elements can further complicate the immune system’s response, leading to the manifestation of symptoms associated with Felty’s Syndrome.
Pathophysiology of Felty’s Syndrome
The pathophysiology of Felty’s Syndrome is complex and closely linked to rheumatoid arthritis. This syndrome typically develops in patients with long-standing RA, indicating a deeper immune dysfunction.
At the core of this condition lies immune system dysregulation. The body’s immune response becomes overactive, leading to the destruction of healthy tissue alongside inflammation.
Splenomegaly is another key feature. The spleen enlarges due to increased activity as it attempts to filter out abnormal blood cells and manage heightened immunological demands.
This combination can lead to significant complications for individuals affected by Felty’s Syndrome, impacting their overall health and well-being. Understanding these mechanisms is crucial for effective management and treatment strategies.
Relationship to Rheumatoid Arthritis
Felty’s Syndrome is closely related to rheumatoid arthritis (RA), often considered a severe manifestation of the disease. The majority of individuals with Felty’s Syndrome have a history of RA, which can complicate their clinical picture.
The autoimmune nature of both conditions means that inflammation affects not only joints but also other systems in the body. This chronic inflammation can lead to significant changes in immune function, resulting in symptoms beyond those typically associated with RA.
Neutropenia, a hallmark feature of Felty’s Syndrome, stems from this underlying autoimmune process. As the body fights against its own tissues, it inadvertently hampers the production and circulation of white blood cells necessary for fighting infections.
Understanding this relationship is crucial for effective management and treatment. Early detection and tailored interventions can greatly improve outcomes for patients affected by these interconnected disorders.
Immune System Dysfunction
Immune system dysfunction is a hallmark of Felty’s Syndrome. The condition significantly alters how the body’s immune response functions, leading to increased vulnerability to infections.
Patients often experience an imbalance in immune cell activity. This includes abnormalities in both T-cells and B-cells, which are crucial for mounting effective responses against pathogens. Such dysfunction can result in persistent inflammation and autoimmunity.
Neutropenia is another critical aspect related to immune dysregulation. With a lower number of neutrophils, individuals struggle more with bacterial infections, highlighting the importance of understanding this dynamic.
The interplay between rheumatoid arthritis and Felty’s further complicates matters. Chronic inflammation from arthritic conditions exacerbates immune challenges faced by patients. Addressing these issues early on can help manage symptoms effectively and improve overall health outcomes.
Splenomegaly Mechanism
Splenomegaly, or enlargement of the spleen, is a key feature of Felty’s Syndrome. This condition arises from an overactive immune response associated with rheumatoid arthritis.
In Felty’s Syndrome, the spleen becomes hyperplastic due to increased demand for immune cell production. As neutrophil levels drop in the bloodstream—thanks to autoimmune destruction—the body relies more on the spleen to generate these vital cells.
The enlarged spleen can also sequester blood cells, further contributing to anemia and thrombocytopenia. This sequestration happens because the blood flow through an enlarged organ slows down, leading to a backup and trapping of platelets and other cells.
Additionally, splenic dysfunction may impair normal filtration processes. Consequently, this can increase vulnerability to infections as your body struggles with both inflammation and reduced immunity. Understanding this mechanism sheds light on how Felty’s Syndrome complicates overall health management.
Clinical Manifestations of Felty’s Syndrome
Felty’s Syndrome primarily manifests through symptoms associated with rheumatoid arthritis. Patients often experience joint pain, swelling, and stiffness. These symptoms can lead to significant discomfort and mobility issues.
Another hallmark of Felty’s Syndrome is neutropenia, a condition characterized by an abnormally low level of neutrophils in the blood. This deficiency increases susceptibility to infections, complicating patient care.
Splenomegaly is also common in those affected by this syndrome. The spleen becomes enlarged due to immune system dysfunction and increased activity in filtering out abnormal cells. This enlargement may cause abdominal discomfort or a feeling of fullness even after eating small meals.
Understanding these clinical manifestations is essential for early diagnosis and effective management strategies tailored specifically for individuals living with Felty’s Syndrome.
Rheumatoid Arthritis Symptoms
Rheumatoid arthritis (RA) is a chronic inflammatory disorder that primarily affects the joints. Patients often experience joint pain, swelling, and stiffness, particularly in the morning or after periods of inactivity. This discomfort can hinder daily activities and reduce overall mobility.
In addition to physical symptoms, RA may cause fatigue and malaise. Many individuals report feeling unusually tired even with adequate rest.
As the condition progresses, joint deformities may occur due to prolonged inflammation. Affected areas typically include hands, wrists, and knees but can extend to other parts of the body.
Systemic involvement is also possible; patients might develop symptoms like fever or weight loss as their immune system reacts abnormally. Recognizing these signs early on is crucial for effective management and treatment options tailored to individual needs.
Neutropenia
Neutropenia is a condition characterized by an abnormally low level of neutrophils, which are critical white blood cells responsible for fighting off infections. In Felty’s Syndrome, this reduction can significantly impair the body’s ability to respond to bacterial and fungal pathogens.
Patients with neutropenia may experience frequent infections that can range from mild to severe. Symptoms often include fever, chills, or signs of localized infection like redness and swelling.
The severity of neutropenia varies among individuals with Felty’s Syndrome. Some may maintain enough neutrophils to fend off common infections, while others might struggle even with minor ailments.
Monitoring neutrophil levels through regular blood tests is essential for managing the risks associated with this condition. Early detection allows healthcare providers to develop effective strategies aimed at preventing complications and improving overall health outcomes.
Splenomegaly
Splenomegaly, or spleen enlargement, is a common feature of Felty’s Syndrome. The spleen plays an essential role in filtering blood and producing immune cells. When it becomes enlarged, this function can be compromised.
In the context of Felty’s Syndrome, splenomegaly often arises due to increased immune activity and the accumulation of white blood cells. This swelling may lead to discomfort in the abdomen and can sometimes be felt as a mass beneath the rib cage.
The condition also contributes to neutropenia by sequestering more white blood cells than usual. As a result, patients might experience fatigue and greater susceptibility to infections.
Monitoring splenic size through regular imaging studies is crucial for managing symptoms effectively. Understanding this aspect helps healthcare providers tailor treatment strategies that address both splenomegaly and its implications for overall health.
Felty’s Syndrome Diagnosis
Diagnosing Felty’s syndrome involves a multifaceted approach. Clinicians begin with a thorough medical history and physical examination, focusing on symptoms of rheumatoid arthritis, neutropenia, and splenomegaly.
Diagnostic criteria play a crucial role in confirming the condition. Typically, patients must exhibit longstanding rheumatoid arthritis alongside significant leukopenia to meet these criteria.
Laboratory tests are essential for identifying low white blood cell counts. A complete blood count (CBC) will often show this decrease in neutrophils.
Imaging studies can provide insight into organ enlargement as well. Ultrasound or CT scans may reveal splenomegaly, enhancing diagnostic accuracy.
Together, these evaluations help differentiate Felty’s syndrome from other conditions with overlapping features.
Diagnostic Criteria
Diagnosing Felty’s Syndrome involves a combination of clinical evaluation and laboratory tests. The primary criteria include the presence of rheumatoid arthritis, neutropenia, and splenomegaly.
Patients must exhibit symptoms consistent with rheumatoid arthritis. This typically includes joint pain, stiffness, and swelling lasting longer than six weeks.
Neutropenia is characterized by an abnormally low count of neutrophils in the blood. A complete blood count (CBC) will help identify this condition.
Additionally, splenomegaly indicates that the spleen has enlarged significantly. Imaging techniques such as ultrasound or CT scans can confirm its size.
Healthcare providers also consider other autoimmune disorders to rule out similar symptoms. Accurate diagnosis is crucial for effective management and treatment strategies tailored to individual needs.
Laboratory Tests
Laboratory tests play a crucial role in diagnosing Felty’s Syndrome. They help to confirm the presence of neutropenia and assess overall health.
Complete blood count (CBC) is often the first test conducted. It effectively identifies low white blood cell counts, particularly neutrophils. The results provide insight into immune function and potential complications.
Additionally, rheumatoid factor (RF) and anti-citrullinated protein antibodies (anti-CCP) are tested to evaluate for rheumatoid arthritis. Elevated levels of these markers can indicate an underlying autoimmune process.
Liver function tests may also be included to rule out other causes of symptoms or abnormalities in blood work. These assessments guide healthcare providers toward accurate diagnoses and tailored treatment plans for those affected by Felty’s Syndrome. Regular monitoring through lab tests ensures that changes in the condition are detected promptly.
Imaging Studies
Imaging studies play a vital role in diagnosing Felty’s Syndrome. These tests help visualize internal structures and assess the extent of complications associated with the condition.
Ultrasound is often used to evaluate splenomegaly, which is an enlarged spleen commonly seen in patients. This non-invasive technique provides real-time images, allowing physicians to measure spleen size accurately.
Computed Tomography (CT) scans can also be beneficial. They offer detailed cross-sectional images of the abdomen and chest, helping identify any other underlying issues or abnormalities that may not be visible through ultrasound alone.
Magnetic Resonance Imaging (MRI) might be employed when there are concerns about joint involvement or soft tissue changes related to rheumatoid arthritis manifestations. It provides high-resolution images without exposure to radiation.
These imaging modalities collectively enhance diagnostic accuracy, guiding healthcare providers in formulating effective treatment plans for individuals affected by Felty’s Syndrome.
Differential Diagnosis of Felty’s Syndrome
Differential diagnosis is crucial in identifying Felty’s Syndrome accurately. Clinicians must consider various conditions that present with similar symptoms, particularly neutropenia.
One condition to rule out is Large Granular Lymphocyte Syndrome (LGL), which can also cause low white blood cell counts. It involves abnormal lymphocytes and may require specific treatments distinct from those for Felty’s.
Other causes of neutropenia include bone marrow disorders or hypersplenism. Investigating these potential culprits ensures appropriate management strategies are employed without delay.
Systemic Lupus Erythematosus (SLE) presents another challenge due to overlapping features like joint pain and fatigue. Distinguishing SLE requires a thorough assessment of autoimmune markers and clinical history.
Accurate differential diagnosis forms the backbone of effective treatment plans, making it essential for improved patient outcomes in those suspected of having Felty’s Syndrome.
Large Granular Lymphocyte Syndrome
Large Granular Lymphocyte (LGL) Syndrome is a hematological condition characterized by an increase in large granular lymphocytes. These are a type of white blood cell involved in the immune response.
This syndrome can manifest as either reactive or neoplastic, with underlying causes ranging from autoimmune diseases to malignancies. Patients may experience symptoms such as fatigue, recurrent infections, and splenomegaly.
The connection between Felty’s Syndrome and LGL Syndrome lies primarily in neutropenia. Both conditions involve low neutrophil counts, which heightens infection risk. Differentiating between these syndromes is crucial for effective management.
Diagnosis typically involves blood tests that reveal elevated levels of atypical lymphocytes alongside decreased neutrophils. Treatment strategies vary based on the underlying cause but often include immunosuppressive therapies or monitoring over time for changes in symptoms or blood cell counts.
Other Causes of Neutropenia
Neutropenia, a condition characterized by low levels of neutrophils, can arise from various causes beyond Felty’s Syndrome. Understanding these alternatives is crucial for accurate diagnosis and treatment.
One common cause is bone marrow disorders, such as aplastic anemia or leukemia. These conditions interfere with the production of blood cells, leading to decreased neutrophil levels.
Infections can also trigger neutropenia. Viral infections like HIV or hepatitis may directly impact bone marrow function. In some cases, certain medications used to treat infections might inadvertently lower neutrophil counts.
Autoimmune diseases present another potential cause. Conditions like systemic lupus erythematosus (SLE) can prompt the immune system to attack its own cells, including those that produce neutrophils.
Nutritional deficiencies play an essential role too. A lack of vitamin B12 or folate can impair cell division in the bone marrow and contribute to low neutrophil counts.
Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE) is an autoimmune disease that can mimic Felty’s Syndrome. It affects multiple systems in the body, leading to a range of symptoms.
Patients with SLE often experience fatigue, joint pain, and skin rashes. The condition can also cause inflammation in organs like the kidneys and heart.
Differentiating between SLE and Felty’s Syndrome is crucial for proper treatment. Both may exhibit neutropenia; however, their underlying mechanisms differ significantly.
In SLE, autoantibodies play a central role in tissue damage. This dysfunction leads to systemic inflammation rather than primarily affecting rheumatoid arthritis as seen in Felty’s.
Awareness of these distinctions ensures patients receive appropriate care tailored to their specific needs. Accurate diagnosis allows healthcare providers to develop effective management strategies that enhance quality of life for those affected by either condition.
Treatment Approaches for Felty’s Syndrome
Managing Felty’s Syndrome requires a multifaceted treatment approach tailored to individual needs. Primarily, controlling rheumatoid arthritis is crucial. This often involves using disease-modifying antirheumatic drugs (DMARDs) to reduce inflammation and joint damage.
Addressing neutropenia is another important aspect of treatment. Medications that stimulate white blood cell production can help mitigate infection risks associated with low neutrophil counts.
For some patients, splenectomy may be considered. Removing the spleen can improve blood cell counts and alleviate symptoms related to splenomegaly. However, this decision should be made carefully alongside healthcare providers due to potential complications.
Regular monitoring and follow-up appointments are essential for adjusting treatments as the condition evolves over time. Individualized care enhances overall health outcomes while managing symptoms effectively.
Management of Rheumatoid Arthritis
Managing rheumatoid arthritis (RA) is crucial for individuals with Felty’s Syndrome. The goal is to reduce inflammation and alleviate pain. Various treatment options are available.
Disease-modifying antirheumatic drugs (DMARDs) play a central role in this management strategy. They help slow disease progression and prevent joint damage. Common DMARDs include methotrexate, sulfasalazine, and leflunomide.
Biologic therapies also show promise, targeting specific pathways involved in the inflammatory process. Options such as tumor necrosis factor (TNF) inhibitors can offer significant relief for some patients.
Regular follow-ups with healthcare providers ensure that treatments remain effective. Monitoring side effects or adjusting dosages may be necessary over time.
Physical therapy can enhance mobility while strengthening muscles around affected joints. Additionally, lifestyle changes that incorporate exercise can improve overall well-being and support joint health during the journey of managing RA within Felty’s Syndrome context.
Addressing Neutropenia
Addressing neutropenia in Felty’s Syndrome is crucial for managing the patient’s overall health. Neutropenia, characterized by a low level of neutrophils, increases vulnerability to infections.
The first step involves regular monitoring of blood counts to assess neutrophil levels accurately. This helps identify fluctuations that may require intervention.
For some patients, treatment with granulocyte colony-stimulating factors (G-CSFs) can stimulate bone marrow production of neutrophils. These medications are often tailored to individual needs based on their response and side effects.
Patients should also adopt preventive measures against infections, such as practicing good hygiene and staying up-to-date with vaccinations. In severe cases where risk is high, doctors might consider temporary antibiotic prophylaxis.
Education about recognizing signs of infection empowers individuals to seek prompt medical attention when necessary. Addressing these aspects effectively can significantly enhance quality of life for those affected by Felty’s Syndrome.
Splenectomy Considerations
Splenectomy, the surgical removal of the spleen, can be an important consideration for patients with Felty’s Syndrome. This procedure may help alleviate some symptoms associated with splenomegaly and improve neutrophil counts.
Patients should discuss potential benefits and risks with their healthcare provider before deciding on this option. While many experience a reduction in infections post-splenectomy, they also face a heightened risk of septic complications due to the spleen’s role in immune response.
Post-operative care is crucial. Vaccinations against common pathogens are often recommended prior to surgery or shortly thereafter, as these can help mitigate infection risks.
Monitoring for signs of infection remains vital after splenectomy. Patients should remain vigilant about any unusual symptoms and maintain regular follow-ups with their medical team to ensure proper management of their health condition following surgery.
Medications for Felty’s Syndrome
Managing Felty’s Syndrome often involves a combination of targeted medications. Disease-Modifying Antirheumatic Drugs (DMARDs) are frequently prescribed to control the underlying rheumatoid arthritis, reducing inflammation and preventing joint damage.
Biologic agents have emerged as vital treatments. They target specific components of the immune system, thereby providing more precise management for those with severe symptoms or inadequate responses to traditional therapies.
Granulocyte colony-stimulating factors may be utilized for patients experiencing neutropenia. These medications stimulate bone marrow production of white blood cells, helping combat infections associated with low neutrophil counts.
Each medication comes with its own set of potential side effects and benefits. Careful monitoring by healthcare professionals is essential to optimize treatment strategies tailored to individual patient needs in managing this complex syndrome effectively.
Disease-Modifying Antirheumatic Drugs (DMARDs)
Disease-Modifying Antirheumatic Drugs, commonly known as DMARDs, play a crucial role in managing Felty’s Syndrome. These medications target the underlying inflammation associated with rheumatoid arthritis, which is often linked to this syndrome.
DMARDs can slow disease progression and prevent joint damage. They work by modifying the immune response that contributes to the inflammatory processes in the body.
Commonly prescribed DMARDs include methotrexate, sulfasalazine, and leflunomide. Each of these has unique mechanisms of action but shares a common goal: reducing symptoms and improving overall function.
While effective for many patients, monitoring is essential due to potential side effects. Regular check-ups help ensure safety while maximizing therapeutic benefits. As part of a comprehensive treatment plan, DMARDs are vital for enhancing quality of life in those affected by Felty’s Syndrome.
Biologic Agents
Biologic agents play a pivotal role in the treatment of Felty’s Syndrome, especially for patients with severe rheumatoid arthritis. These medications target specific components of the immune system, helping to reduce inflammation and slow disease progression.
Common biologics used include tumor necrosis factor (TNF) inhibitors and interleukin-6 (IL-6) blockers. They work by modulating the immune response, addressing both joint symptoms and systemic manifestations associated with Felty’s Syndrome.
Patients often see improvement in their overall wellbeing when incorporating biologic therapy into their regimen. However, it’s essential to monitor for potential side effects such as increased infection risk due to immune suppression.
Collaboration between healthcare providers and patients is vital. Regular assessments can help tailor treatments effectively while managing any adverse reactions that may arise during therapy.
Granulocyte Colony-Stimulating Factors
Granulocyte Colony-Stimulating Factors (G-CSF) play a crucial role in managing neutropenia associated with Felty’s Syndrome. These factors stimulate the bone marrow to produce more white blood cells, particularly neutrophils.
In patients experiencing low neutrophil counts, G-CSF can be administered to enhance immune response. This treatment not only helps reduce infection risk but also aids in improving overall health outcomes.
Commonly prescribed forms of G-CSF include filgrastim and pegfilgrastim, each varying slightly in their dosing schedules and effects. While generally well-tolerated, some individuals may experience side effects such as bone pain or mild fever.
Monitoring is essential during treatment to assess efficacy and any potential adverse reactions. Regular consultations with healthcare providers help ensure that the therapy remains safe and beneficial for those living with Felty’s Syndrome.
Felty’s Syndrome Complications
Felty’s Syndrome can lead to several significant complications that impact a patient’s health. One of the most concerning is the increased risk of infections. Neutropenia, characterized by low levels of neutrophils, compromises the immune system’s ability to fight off pathogens effectively.
Cardiovascular complications also pose a substantial threat. Studies suggest that patients with Felty’s Syndrome are at higher risk for heart disease, possibly due to chronic inflammation and other related factors.
Additionally, there’s an elevated chance of developing secondary malignancies. The long-term effects of immunosuppressive treatments combined with systemic inflammation may contribute to this heightened risk.
Managing these complications requires vigilance and proactive healthcare measures. Regular check-ups and tailored treatment plans are essential for maintaining overall well-being in individuals living with Felty’s Syndrome.
Increased Infection Risk
Individuals with Felty’s Syndrome face a heightened risk of infections. This vulnerability largely stems from neutropenia, characterized by low levels of neutrophils, the white blood cells crucial for fighting off bacteria and fungi.
When these immune defenses weaken, even minor infections can escalate into serious health issues. Common pathogens that would typically be contained may lead to severe complications in affected individuals.
Additionally, splenomegaly—an enlarged spleen often associated with Felty’s—can further compromise immunity. The spleen plays a vital role in filtering blood and mounting immune responses; its dysfunction exacerbates infection risks.
Preventative measures are essential for managing this heightened susceptibility. Regular monitoring and timely vaccinations become critical components of care for those living with Felty’s Syndrome.
Cardiovascular Complications
Cardiovascular complications are a significant concern for individuals with Felty’s Syndrome. The interplay between rheumatoid arthritis and cardiovascular health can lead to increased risks of heart disease.
Chronic inflammation associated with the condition contributes to vascular damage. This persistent inflammation can accelerate atherosclerosis, the hardening of arteries that may result in heart attacks or strokes.
Moreover, patients often experience changes in lipid profiles and elevated blood pressure. These factors further heighten cardiovascular risk.
Regular monitoring of heart health is essential for those diagnosed with Felty’s Syndrome. Engaging healthcare providers about symptoms like chest pain or shortness of breath is crucial for early intervention.
Adopting lifestyle modifications such as balanced nutrition and regular exercise can also play a role in managing these potential complications effectively.
Secondary Malignancies
Patients with Felty’s Syndrome face an elevated risk of developing secondary malignancies. This connection is particularly concerning due to the underlying immune dysfunction associated with the condition.
The presence of neutropenia, a hallmark symptom of Felty’s Syndrome, compromises the body’s ability to fight infections and may also reduce its capacity to detect and eliminate cancerous cells. Consequently, individuals are more vulnerable to various forms of cancer.
Research indicates that those diagnosed with rheumatoid arthritis—often linked to Felty’s—may experience higher rates of lymphoproliferative disorders. Regular monitoring for these complications is essential in managing health outcomes effectively.
Understanding this increased risk helps inform treatment strategies, enabling healthcare providers to implement early detection methods tailored for patients facing this dual challenge. Maintaining open communication between patients and their medical teams can help address concerns surrounding potential malignancies proactively.
Felty’s Syndrome Prognosis and Outcomes
The prognosis for individuals with Felty’s Syndrome varies widely. It largely depends on the severity of their rheumatoid arthritis and associated complications. Early intervention plays a crucial role in improving outcomes.
Factors that influence prognosis include age, overall health, and how well patients manage their symptoms. Those who respond favorably to treatment often experience better quality of life measures.
Quality of life considerations are essential for patients navigating this condition. Issues like fatigue, pain management, and emotional well-being can significantly impact daily living. Supportive care from healthcare providers is vital.
Regular follow-ups help monitor disease progression and adjust treatments accordingly. This proactive approach enhances long-term outlooks for many individuals facing Felty’s Syndrome challenges.
Long-term Outlook
The long-term outlook for individuals with Felty’s Syndrome varies widely. It largely depends on the severity of rheumatoid arthritis and associated complications. Many patients experience chronic symptoms, which can significantly impact their quality of life.
Management strategies play a critical role in shaping outcomes. Early diagnosis and appropriate treatment can help mitigate some risks associated with the syndrome. Regular monitoring is essential to address any emerging issues promptly.
Patients may face challenges such as increased susceptibility to infections due to neutropenia. This requires ongoing vigilance and proactive health measures.
While some individuals lead relatively normal lives, others might struggle more profoundly with physical limitations or systemic complications over time. Understanding personal trajectories is crucial for effective management and support throughout the journey of living with Felty’s Syndrome.
Factors Affecting Prognosis
The prognosis for Felty’s Syndrome can vary significantly among individuals. Several key factors play a role in determining outcomes.
First, the duration and severity of rheumatoid arthritis prior to diagnosis are crucial. Individuals with long-standing or severe forms may face more challenges.
Age also influences prognosis; younger patients often experience better outcomes compared to older adults who may have additional health complications.
Another important factor is the presence of comorbid conditions. Patients with concurrent diseases, such as cardiovascular issues or diabetes, tend to have worse prognoses due to increased complexity in managing their health.
Adherence to treatment plans can greatly affect an individual’s quality of life and overall outcome. Consistent management strategies tailored by healthcare providers lead to improved results over time.
Quality of Life Considerations
Living with Felty’s Syndrome can significantly affect one’s quality of life. The combination of rheumatoid arthritis, neutropenia, and splenomegaly may lead to chronic pain and fatigue. This persistent discomfort often hinders daily activities.
Social interactions can also suffer as individuals may feel isolated due to their health conditions. Fear of infections from neutropenia can deter them from participating in community events or gatherings.
Mental health is another crucial aspect impacted by the syndrome. Anxiety and depression are common among patients coping with ongoing symptoms and lifestyle restrictions.
Regular follow-ups with healthcare providers are essential for managing these challenges effectively. Support groups offer a sense of community, helping individuals share experiences and strategies for coping with the condition more positively.
Making informed decisions about treatment options enhances autonomy over one’s health journey, ultimately improving overall well-being.
Living with Felty’s Syndrome
Living with Felty’s Syndrome requires a proactive approach to health and well-being. Patients often face unique challenges due to the combination of rheumatoid arthritis, neutropenia, and splenomegaly.
Adopting lifestyle modifications is crucial. Regular exercise can help maintain mobility and manage pain levels. It’s essential to choose low-impact activities that suit individual capabilities.
Infection prevention strategies are paramount for those with neutropenia. This includes practicing good hygiene, staying away from sick individuals, and ensuring vaccinations are up-to-date.
Nutritional considerations also play a role in managing this syndrome. A balanced diet rich in vitamins and minerals supports overall immune function while addressing any deficiencies related to chronic illness.
Connecting with support groups offers emotional relief too. Sharing experiences with others facing similar struggles can provide coping mechanisms and enhance resilience during difficult times.
Lifestyle Modifications
Making lifestyle modifications can significantly improve the quality of life for individuals with Felty’s Syndrome. Focusing on a balanced diet is essential. Incorporating anti-inflammatory foods, such as fruits, vegetables, whole grains, and healthy fats can help manage symptoms.
Regular exercise also plays a vital role in overall well-being. Low-impact activities like swimming or walking enhance physical fitness without putting excessive strain on joints.
Stress management techniques are equally important. Practices like yoga or meditation can reduce stress levels and promote relaxation.
Staying hydrated supports general health and aids bodily functions. Drinking plenty of water should become part of daily habits.
Maintaining regular check-ups with healthcare providers ensures timely monitoring and intervention when needed. These proactive measures contribute to improved management of Felty’s Syndrome symptoms while fostering resilience in daily life.
Infection Prevention Strategies
Infection prevention is crucial for individuals living with Felty’s Syndrome due to their increased vulnerability. A proactive approach can significantly reduce the risk of infections.
Regular hand hygiene is essential. Washing hands thoroughly with soap and water or using an alcohol-based sanitizer can help eliminate harmful pathogens.
Vaccinations should be up-to-date, including flu shots and pneumonia vaccines. These immunizations provide a vital defense against common infections.
Avoiding crowded places during peak illness seasons also helps minimize exposure to viruses and bacteria.
Wearing masks in such environments adds another layer of protection, especially when around those who are sick.
Maintaining a clean home environment reduces the presence of germs. Routine disinfection of frequently touched surfaces plays a key role in this effort.
Consult healthcare providers about individualized strategies tailored to specific health needs for optimal safety measures against potential infections associated with Felty’s Syndrome.
Nutritional Considerations
Nutritional considerations play a vital role in managing Felty’s Syndrome. A well-balanced diet can help mitigate symptoms and improve overall health.
It’s essential to focus on nutrient-rich foods. Incorporating plenty of fruits, vegetables, whole grains, and lean proteins supports immune function and reduces inflammation.
Omega-3 fatty acids found in fish like salmon or flaxseeds may also provide anti-inflammatory benefits. Staying hydrated is equally important; adequate water intake helps maintain bodily functions.
Patients should be cautious with processed foods high in sugar and unhealthy fats, as these can exacerbate inflammatory responses.
Some individuals might experience dietary restrictions due to associated conditions like rheumatoid arthritis. Consult with healthcare providers or nutritionists for personalized advice tailored to individual needs.
Maintaining a healthy weight through proper nutrition can alleviate stress on joints while enhancing energy levels throughout the day.
Research and Clinical Trials
Research into Felty’s Syndrome is crucial for understanding its complexities and improving patient outcomes. Current studies focus on the underlying mechanisms that link this condition to rheumatoid arthritis, particularly how immune dysregulation contributes to symptoms.
Ongoing clinical trials aim to evaluate new treatment options, exploring medications that target specific pathways involved in both autoimmune responses and hematological abnormalities. These trials are essential for developing targeted therapies that could offer better management strategies.
Emerging therapies also include innovative biologic agents designed to address inflammation more effectively while minimizing side effects. As research progresses, there is hope for breakthroughs that could enhance quality of life for those living with Felty’s Syndrome.
Participation in these clinical studies can provide patients access to cutting-edge treatments while contributing valuable data toward future medical advancements.
Current Research Focus
Current research on Felty’s Syndrome is delving into the intricate relationship between this condition and rheumatoid arthritis. Scientists are investigating biomarkers that could help in early diagnosis and treatment strategies.
Another area of focus is immune dysfunction. Researchers aim to understand how the immune system malfunctions in Felty’s Syndrome, particularly regarding neutrophil production and functionality.
Clinical trials are also exploring novel therapies designed to enhance quality of life for those affected. This includes various biologic agents that target specific pathways involved in inflammation and immune response.
Additionally, studies are looking into genetic predispositions linked to Felty’s Syndrome. Understanding these factors may lead to personalized treatment approaches tailored for individuals based on their unique genetic makeup.
The ongoing efforts promise to shed light on effective management strategies, improving outcomes for patients living with this complex syndrome.
Ongoing Clinical Studies
Ongoing clinical studies on Felty’s Syndrome are crucial for advancing our understanding of this complex condition. Researchers are exploring various aspects, from its pathophysiology to innovative treatment approaches.
Many trials focus on evaluating the effectiveness of new biologic agents and disease-modifying antirheumatic drugs (DMARDs). These medications aim to improve symptoms and reduce the frequency of flare-ups in patients suffering from both rheumatoid arthritis and Felty’s Syndrome.
Additionally, some studies investigate the role of granulocyte colony-stimulating factors. This could potentially enhance neutrophil production, addressing one of the syndrome’s primary complications: neutropenia.
Patient registries also play an essential part in ongoing research efforts. They help collect data that can lead to better treatment strategies tailored to individual needs based on demographics and response patterns. Insights gained from these studies may pave the way for more effective management options in the future.
Emerging Therapies
Emerging therapies for Felty’s Syndrome are gaining attention in the medical community. Researchers are exploring innovative treatments that target the underlying immune dysfunction.
One promising area involves biologic agents, which specifically inhibit pathways involved in inflammation. These medications could provide relief from both rheumatoid arthritis symptoms and associated complications like neutropenia.
Another exciting development is gene therapy. This approach aims to correct genetic defects influencing the immune system, potentially offering a long-term solution rather than symptomatic treatment.
Additionally, ongoing studies focus on combination therapies that integrate traditional drugs with novel agents. Such strategies may enhance efficacy while minimizing side effects associated with conventional treatments.
Researchers continue to investigate new immunomodulatory drugs as well. These could play a significant role in modulating the immune response more effectively for individuals suffering from Felty’s Syndrome.
The landscape of treatment options is evolving rapidly, providing hope for better management of this complex condition.
Genetic Aspects
Genetic aspects play a significant role in understanding Felty’s Syndrome. Research indicates that certain genetic factors may predispose individuals to this condition, particularly among those with rheumatoid arthritis.
Family history is another critical consideration. Individuals with relatives who have autoimmune disorders may face a higher risk of developing Felty’s Syndrome themselves. This familial link highlights the importance of assessing genetic backgrounds during diagnosis.
Moreover, genetic testing can provide insights into potential vulnerabilities. Identifying specific gene mutations associated with immune dysfunction could pave the way for targeted therapies and personalized treatment plans.
By exploring these genetic components, healthcare providers can better understand how to manage and treat patients effectively while considering their unique biological makeup. Advances in genetics continue to illuminate pathways toward improved care for those affected by this rare syndrome.
Genetic Predisposition
Genetic predisposition plays a significant role in Felty’s Syndrome. Individuals with a family history of autoimmune diseases are more likely to develop this condition. The interplay between genetics and environmental factors can lead to immune system dysfunction.
Certain genes associated with rheumatoid arthritis may also contribute to the risk of developing Felty’s Syndrome. Variations in these genes can influence how the body reacts to inflammation, potentially resulting in neutropenia and splenomegaly.
Researchers are exploring specific genetic markers linked to Felty’s Syndrome. Understanding these markers could help identify at-risk individuals early on, providing opportunities for proactive management and interventions tailored to their unique genetic profile.
Additionally, familial clustering has been observed in some cases, highlighting the importance of considering family medical histories when assessing potential risks for this syndrome.
Family History Considerations
Family history plays a crucial role in understanding the risk of developing Felty’s Syndrome. Research suggests that individuals with close relatives who have rheumatoid arthritis or autoimmune disorders may be at a heightened risk for this condition.
Genetic factors can influence immune system function, increasing susceptibility to both rheumatoid arthritis and its complications. If there is a pattern of autoimmune diseases within a family, it’s important for members to discuss these concerns with healthcare providers.
Understanding one’s family medical history helps inform screening and preventive measures. Those with relatives affected by related conditions might benefit from early monitoring or genetic counseling. This proactive approach can lead to better management options should symptoms arise down the line.
Being aware of such familial links empowers patients in their health journey, fostering informed discussions about possible genetic predispositions and lifestyle adjustments necessary for overall well-being.
Genetic Testing
Genetic testing plays a crucial role in understanding Felty’s Syndrome. This condition has links to genetic predispositions, which can influence its development and severity. Identifying specific genetic markers may help assess an individual’s risk.
Testing often involves blood samples analyzed for mutations or variants associated with autoimmune diseases. Genetic counselors may assist patients in interpreting results, providing insights into the familial patterns of disease.
Additionally, knowing one’s genetic makeup can guide treatment decisions. It allows healthcare providers to tailor therapies based on unique biological responses observed in individuals with certain genetic profiles.
As research progresses, the potential for personalized medicine continues to expand. More targeted interventions could improve outcomes and enhance quality of life for those affected by Felty’s Syndrome.
Immunological Features
Immunological features play a crucial role in understanding Felty’s Syndrome. This condition is often accompanied by specific autoantibodies that can be detected in the bloodstream, particularly rheumatoid factor and anti-citrullinated protein antibodies. These markers indicate an ongoing autoimmune response.
T-cell abnormalities also emerge as significant characteristics of Felty’s Syndrome. Patients frequently exhibit altered T-cell populations, which contribute to immune dysregulation. This imbalance may lead to decreased effectiveness in fighting infections.
Furthermore, B-cell dysfunction is commonly observed. The impaired production of immunoglobulins can result in increased vulnerability to pathogens. As a whole, these immunological features highlight the complexity of Felty’s Syndrome and underscore the need for comprehensive management strategies tailored to each patient’s unique immune profile.
Autoantibodies in Felty’s Syndrome
Autoantibodies play a crucial role in Felty’s Syndrome, often serving as biomarkers for the disease. These proteins are produced when the immune system mistakenly targets the body’s own tissues. In Felty’s Syndrome, the presence of specific autoantibodies can indicate an ongoing autoimmune process linked to rheumatoid arthritis.
Rheumatoid factor (RF) is one of the most commonly detected autoantibodies in patients with this condition. Additionally, anti-citrullinated protein antibodies (ACPAs) may also be present, further complicating the clinical picture. The detection of these autoantibodies helps physicians understand disease severity and tailor treatment plans accordingly.
Understanding these immunological features enhances our grasp of Felty’s Syndrome progression and its relationship to other autoimmune disorders. It opens avenues for potential targeted therapies that could improve patient outcomes and quality of life significantly. Researchers continue to explore how these antibodies contribute to systemic symptoms experienced by individuals with Felty’s Syndrome.
T-cell Abnormalities
T-cell abnormalities play a significant role in the pathophysiology of Felty’s Syndrome. These immune cells are crucial for orchestrating responses against infections and regulating other immune functions. In individuals with Felty’s, the T-cells often exhibit dysregulation.
Research indicates that there may be a shift in the balance between different T-cell subtypes. This can lead to an impaired immune response, contributing to increased susceptibility to infections. Elevated levels of certain T-helper cell types have been observed, which can further exacerbate inflammation.
Additionally, some studies suggest that these abnormal T-cells may influence the autoimmune processes characteristic of rheumatoid arthritis. Their presence complicates treatment strategies as they affect how well patients respond to therapies aimed at modulating the immune system.
Understanding these abnormalities is essential for developing targeted interventions. It opens avenues for personalized treatments tailored specifically to address these immunological challenges faced by those living with Felty’s Syndrome.
B-cell Dysfunction
B-cell dysfunction is a significant aspect of Felty’s Syndrome. B-cells, part of the immune system, are responsible for producing antibodies that help combat infections and diseases. In patients with Felty’s Syndrome, these cells often exhibit abnormalities.
This dysfunction can lead to impaired antibody production. As a result, individuals may struggle to fight off infections effectively. The presence of autoantibodies further complicates the picture by contributing to autoimmune reactions.
Additionally, deregulated B-cells can escalate inflammation in the body. This can exacerbate symptoms related to rheumatoid arthritis and worsen overall health outcomes.
Understanding B-cell behavior is crucial for developing targeted therapies focused on restoring their normal function. Addressing this dysfunction could pave the way for better management strategies for those affected by Felty’s Syndrome.
Hematological Management
Hematological management in Felty’s Syndrome focuses on addressing blood-related complications, particularly neutropenia. This condition significantly increases the risk of infections due to a low white blood cell count.
Treatment strategies for neutropenia often include monitoring and supportive care. Patients might need regular blood tests to check their levels. In some cases, medications like granulocyte colony-stimulating factors can help stimulate bone marrow production of neutrophils.
Anemia is another concern in Felty’s Syndrome. It may occur due to chronic inflammation or as a side effect of treatments for rheumatoid arthritis. Managing anemia involves iron supplementation and sometimes erythropoiesis-stimulating agents.
Thrombocytopenia can also arise in these patients, necessitating careful evaluation of platelet counts and potential interventions if bleeding risks increase. A comprehensive approach ensures optimal health while managing hematological issues associated with this syndrome.
Neutropenia Treatment Strategies
Neutropenia treatment strategies focus on addressing the underlying causes while managing symptoms. The first step often involves identifying and treating any infections, as individuals with neutropenia are at higher risk.
Granulocyte Colony-Stimulating Factors (G-CSF), such as filgrastim, are commonly used to stimulate bone marrow production of white blood cells. This can help increase neutrophil counts and promote better immune function.
In cases where medications or autoimmune disorders induce neutropenia, adjusting or changing treatments may be necessary. Doctors might consider immunosuppressants or corticosteroids based on each patient’s unique circumstances.
For some patients, prophylactic antibiotics are recommended to prevent infections during periods of severe neutropenia. Monitoring blood counts regularly ensures early detection of drops in white cell levels and timely intervention when needed.
Lifestyle changes play a crucial role too. Patients should adopt practices that minimize infection risks while boosting overall health.
Anemia in Felty’s Syndrome
Anemia is a common complication associated with Felty’s Syndrome, impacting many patients. This condition occurs when the body lacks enough healthy red blood cells to carry adequate oxygen to tissues.
In Felty’s Syndrome, anemia can arise from several factors. Chronic inflammation due to rheumatoid arthritis plays a significant role. Inflammatory cytokines can suppress erythropoiesis, the process of producing red blood cells in the bone marrow.
Additionally, nutritional deficiencies may contribute to this issue. Iron deficiency is particularly prevalent and can worsen symptoms like fatigue and weakness.
Monitoring hemoglobin levels regularly is crucial for effective management. Treatment options may involve dietary adjustments or supplementation if necessary. Addressing underlying causes often helps improve overall health outcomes in individuals facing this challenge.
Thrombocytopenia Considerations
Thrombocytopenia, or low platelet count, is a significant concern for individuals with Felty’s Syndrome. This condition can lead to increased bruising and bleeding risks. Understanding the implications of thrombocytopenia is vital for managing overall health.
Patients should be aware that certain medications can exacerbate this issue. It’s essential to work closely with healthcare professionals when it comes to treatments that may affect platelet levels. Regular monitoring of blood counts helps detect any changes early on.
Dietary adjustments can also play a role in managing thrombocytopenia. Incorporating foods rich in vitamins K and C may support better platelet function. Staying hydrated is equally important as dehydration can further complicate symptoms.
Addressing thrombocytopenia requires a comprehensive approach tailored to each patient’s needs. By focusing on prevention strategies and regular check-ups, individuals with Felty’s Syndrome can enhance their quality of life while effectively managing their condition.


