Introduction to Fahr’s Syndrome
Fahr’s Syndrome is a rare neurological disorder that can leave both patients and caregivers grappling with its complexities. It’s characterized by abnormal calcium deposits in the brain, leading to a variety of symptoms that can affect movement, cognition, and mood. While this condition may not be widely known, understanding Fahr’s Syndrome is crucial for those impacted by it.
This blog post aims to delve into the science behind Fahr’s Syndrome—from its definitions and historical context to its underlying mechanisms and clinical features. Whether you’re seeking knowledge for personal reasons or simply curious about this intriguing condition, you’ll find valuable insights here. Join us as we explore the intricate world of Fahr’s Syndrome and uncover what makes it so unique in the field of neurology.

Fahr’s Syndrome Definition and Overview
Fahr’s Syndrome is a rare neurological disorder characterized by abnormal calcium deposits in the brain. These calcifications primarily affect specific areas, leading to various neurological and psychological symptoms.
This condition can manifest in both familial and sporadic forms. In familial cases, genetic mutations play a significant role, while sporadic instances may arise without any clear inherited pattern.
“What Causes Patent Ductus Arteriosus Syndrome in Newborns?”
Individuals with Fahr’s Syndrome often experience movement disorders, cognitive decline, and mood disturbances due to these calcifications disrupting normal brain function.
Despite its rarity, understanding Fahr’s Syndrome is crucial for accurate diagnosis and effective management of its associated challenges. It underscores the complexity of how mineral imbalances can significantly impact neurological health.
Historical Background and Nomenclature
Fahr’s Syndrome was first described in 1930 by the German psychiatrist Karl Friedrich Fahr. He identified a peculiar pattern of brain calcifications that were associated with neurological symptoms. This foundational observation laid the groundwork for understanding this rare condition.
The term “Fahr’s Syndrome” is derived from his name, reflecting its connection to these unique calcium deposits found primarily in certain brain regions. Over time, researchers have expanded on Fahr’s initial findings, uncovering various genetic and environmental factors contributing to the syndrome.
“Why Does Pearson Syndrome Affect Blood Cells?”
Notably, early literature often conflated Fahr’s Syndrome with other disorders characterized by similar calcifications. As research progressed, medical professionals began delineating it more clearly from related conditions like pseudohypoparathyroidism and other metabolic disturbances. Today, it stands recognized as a distinct entity within neurology and genetics.
Pathophysiology of Fahr’s Syndrome
Fahr’s Syndrome is characterized by abnormal calcium deposition in the brain. This process occurs primarily in specific regions, leading to neurological dysfunction.
Calcium buildup disrupts normal cellular functions and communication within the brain. As these deposits accumulate, they can interfere with neurotransmitter release and neuronal signaling.
“How Does Prader-Willi Syndrome Impact Growth?”
The areas most affected include the basal ganglia, thalamus, and cerebral cortex. Damage in these regions often correlates with various cognitive and motor symptoms observed in patients.
Neurological impacts may range from movement disorders to psychiatric manifestations. The severity of symptoms largely depends on the extent of calcification and its location within the brain.
Understanding this pathophysiology is vital for developing targeted treatment strategies that address both symptomatic relief and disease management.
Calcium Deposition in the Brain
Calcium deposition in the brain is a hallmark of Fahr’s Syndrome. This unusual accumulation primarily occurs in specific regions, such as the basal ganglia and thalamus. These areas are crucial for motor control and cognitive functions.
The process begins when calcium levels become dysregulated within neuronal cells. Factors influencing this dysregulation may include genetic mutations or metabolic imbalances. As excess calcium deposits accumulate, they can interfere with normal brain function.
“What Are The Signs of Parsonage-Turner Syndrome?”
While some individuals remain asymptomatic despite these calcifications, others experience significant neurological challenges. Symptoms often arise due to disrupted signaling pathways and impaired communication between neurons.
Research continues to explore the precise mechanisms behind calcium deposition in Fahr’s Syndrome. Understanding these processes may reveal potential targets for treatment and management strategies aimed at mitigating symptoms associated with this condition.
Affected Brain Regions
Fahr’s Syndrome is characterized by abnormal calcium deposits primarily in specific regions of the brain. These calcifications typically occur within the basal ganglia, a group of structures involved in coordinating movement and other functions.
“Why Does Patterson-Kelly Syndrome Cause Swallowing Issues?”
The putamen and globus pallidus are frequently affected areas. Calcifications here can disrupt normal signaling pathways, leading to various neurological symptoms.
Additionally, involvement of the cerebral cortex may occur, impacting cognitive functions and emotional regulation. Other regions like the thalamus might also exhibit changes but to a lesser extent.
Understanding which areas are impacted helps clinicians assess potential functional impairments in patients with Fahr’s Syndrome. Each region plays a vital role in motor control and cognitive processes, making these findings crucial for effective diagnosis and treatment planning.
Neurological Impacts of Fahr’s Syndrome
Fahr’s Syndrome leads to significant neurological impacts due to abnormal calcium deposits in the brain. These calcifications predominantly affect areas involved in motor control, cognition, and emotional regulation.
Patients often experience a range of symptoms that can include cognitive decline, memory loss, and difficulties with concentration. These cognitive impairments may progress over time, impacting daily functioning.
“How Does Pelizaeus-Merzbacher Syndrome Affect Myelin?”
Movement disorders are also common. Individuals might exhibit tremors, rigidity, or difficulty coordinating movements. Such challenges can hinder basic activities like walking or writing.
Additionally, Fahr’s Syndrome may lead to psychiatric issues such as anxiety and depression. The interplay between neurological deficits and mental health can create complex challenges for patients and caregivers alike.
Understanding these neurological impacts is crucial for effective management strategies tailored to individual needs.
Fahr’s Syndrome Causes and Risk Factors
Fahr’s Syndrome is often linked to genetic factors. Mutations in specific genes can lead to abnormal calcium metabolism, resulting in calcifications within the brain. These hereditary patterns are sometimes seen in families, suggesting a potential autosomal dominant inheritance.
Sporadic cases of Fahr’s Syndrome also occur without any family history. Environmental influences and acquired conditions may contribute to these instances.
Certain medical conditions further elevate the risk of developing Fahr’s Syndrome. Disorders such as hyperparathyroidism or metabolic disorders involving calcium imbalance can predispose individuals to brain calcifications.
Understanding these causes and risk factors is essential for early detection and intervention, allowing for more effective management strategies tailored to individual needs.
Genetic Factors
Genetic factors play a significant role in Fahr’s Syndrome, influencing its occurrence and progression. This condition is often linked to mutations in specific genes that affect calcium metabolism and deposition in the brain.
One of the primary genetic contributors identified is SLC20A2. Mutations here lead to abnormal phosphate regulation, resulting in calcifications within neural tissues. Other related genes include PDGFB and XPR1, which are also implicated but less frequently.
Familial cases suggest an autosomal dominant inheritance pattern, meaning that a single mutated gene from an affected parent can be sufficient for transmission to offspring. However, not all individuals with genetic predispositions develop symptoms; environmental interactions may influence this variability.
Understanding these genetic underpinnings helps researchers explore potential therapeutic avenues and offers insight into risk assessment for families impacted by Fahr’s Syndrome.
Sporadic Cases
Sporadic cases of Fahr’s Syndrome occur without a known family history or genetic predisposition. These instances are intriguing because they can arise in individuals who appear otherwise healthy, with no identifiable risk factors.
The mechanisms behind sporadic occurrences remain largely unclear. Researchers speculate that environmental influences or unique biological changes may play a role.
Some studies suggest that metabolic imbalances could contribute to the development of these calcifications in the brain, but further investigation is needed to fully understand these connections.
Interestingly, sporadic cases can present similar symptoms as hereditary ones, complicating diagnosis and treatment. This unpredictability highlights the need for thorough clinical evaluation when addressing potential Fahr’s Syndrome in patients lacking familial links.
Associated Medical Conditions
Fahr’s Syndrome can occur alongside various medical conditions that complicate its diagnosis and management. One notable association is with primary hyperparathyroidism, where elevated calcium levels may contribute to calcifications in the brain.
Additionally, certain metabolic disorders like mitochondrial diseases have been linked to Fahr’s Syndrome. These conditions affect energy production at the cellular level and can manifest as neurological symptoms.
Other associated medical issues include kidney dysfunctions, which often disrupt mineral balance in the body. This imbalance could further exacerbate calcium deposits within the brain.
In some cases, patients might also experience endocrine abnormalities, such as thyroid or adrenal gland disorders. These disruptions play a significant role in overall health and must be monitored closely for optimal care.
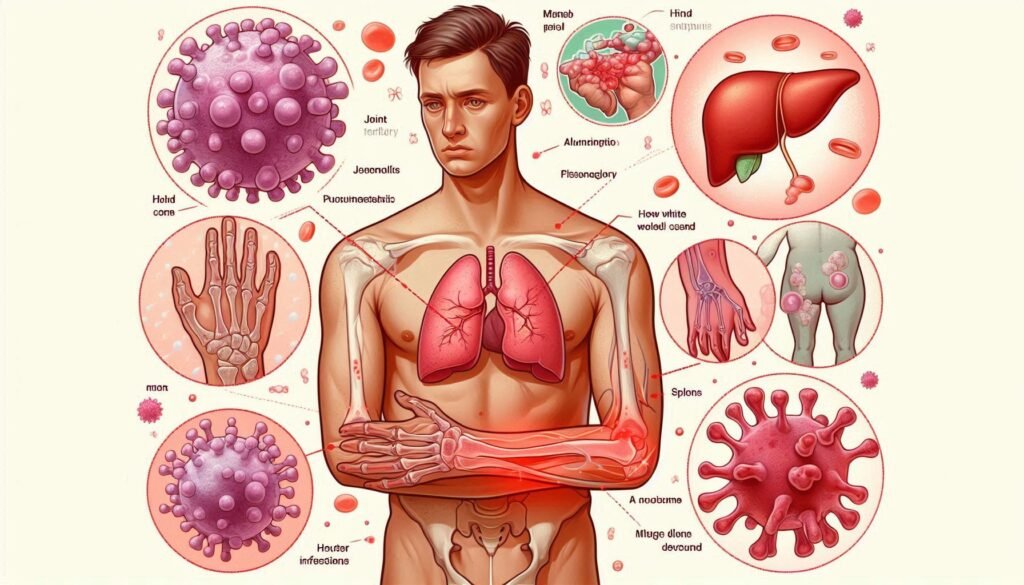
Fahr’s Syndrome Signs and Symptoms
Fahr’s Syndrome presents a range of symptoms primarily affecting neurological function. Patients may experience cognitive impairments, making it difficult to concentrate or remember information. This decline in mental clarity can significantly impact daily life.
Psychiatric manifestations are also common, with many individuals reporting mood swings, anxiety, and depression. These psychological changes often complicate the clinical picture.
Movement disorders characterize Fahr’s Syndrome as well. Patients might struggle with coordination and balance, leading to tremors or abnormal gait patterns. These motor issues stem from calcifications in specific brain regions that disrupt normal functioning.
Recognizing these signs early is crucial for effective management and intervention strategies tailored to each individual’s needs. Understanding the full spectrum of symptoms helps provide better care options for those affected by this rare condition.
Neurological Symptoms
Neurological symptoms of Fahr’s Syndrome can significantly impact a patient’s daily life. Patients may experience cognitive decline, including memory issues and difficulty concentrating.
Severe cases often lead to speech disturbances. Individuals might struggle with finding words or forming coherent sentences, which can be frustrating for both the patient and their loved ones.
Motor skills are also affected. This may manifest as muscle stiffness, tremors, or uncoordinated movements. These challenges can hinder basic tasks like writing or buttoning a shirt.
In addition to these physical symptoms, some patients report seizures that vary in frequency and intensity. Such episodes require careful monitoring and management by healthcare professionals.
The presence of headaches is common among those with this condition. The nature and severity of these headaches can differ widely from person to person.
Psychiatric Manifestations
Fahr’s Syndrome is not just a neurological disorder; it also has significant psychiatric implications. Patients may experience a range of mood disorders, including depression and anxiety. These feelings can stem from the challenges of coping with their physical symptoms.
Cognitive impairment is another common manifestation. Individuals may struggle with memory, attention, and problem-solving abilities. This cognitive decline can lead to frustration and isolation.
Additionally, personality changes might occur in some patients. Affected individuals could display increased irritability or emotional lability. Such shifts often complicate relationships with family members and friends.
The interplay between neurological symptoms and psychiatric manifestations makes diagnosis challenging. Mental health support becomes crucial in managing these aspects effectively for those living with Fahr’s Syndrome. Addressing both sides ensures comprehensive care tailored to individual needs.
Movement Disorders
Movement disorders in Fahr’s Syndrome can significantly impact daily life. Patients often experience tremors, which are involuntary shaking movements that may affect one or more parts of the body.
Another common issue is dystonia. This condition leads to abnormal muscle contractions, resulting in twisting and repetitive movements. The rigidity often associated with this disorder can make it challenging for individuals to maintain normal posture.
Additionally, bradykinesia may occur, characterized by slowed movement. This symptom complicates tasks such as walking or performing fine motor skills.
Coordination problems are also prevalent, making balance difficult and increasing the risk of falls. These movement-related issues require careful management to enhance mobility and quality of life for those affected by Fahr’s Syndrome.
Fahr’s Syndrome Diagnosis
Diagnosing Fahr’s Syndrome involves a combination of advanced imaging techniques and thorough clinical evaluations. Neuroimaging, particularly computed tomography (CT) scans and magnetic resonance imaging (MRI), plays a crucial role in identifying brain calcifications characteristic of the syndrome.
These images help doctors visualize abnormal calcium deposits in specific regions of the brain. A careful analysis can distinguish Fahr’s from other conditions that may present similarly.
Alongside neuroimaging, healthcare professionals conduct comprehensive clinical assessments to evaluate neurological functions and symptoms reported by patients. This multifaceted approach ensures an accurate diagnosis.
In certain cases, genetic testing may be recommended to identify hereditary patterns associated with Fahr’s Syndrome. Identifying mutations can provide valuable insights into individual prognosis and guide treatment strategies effectively.
Neuroimaging Techniques (CT, MRI)
Neuroimaging techniques are crucial in diagnosing Fahr’s Syndrome. Computed Tomography (CT) scans provide a quick overview of brain structure. This method highlights the presence of calcium deposits, which are characteristic of this disorder.
Magnetic Resonance Imaging (MRI) offers greater detail than CT. It captures subtle changes in brain tissue and can reveal calcifications that may be missed on a CT scan. MRI is particularly effective at visualizing affected areas, such as the basal ganglia and cortex.
These imaging tools help neurologists assess the extent of calcification and correlate it with clinical symptoms. Early detection through neuroimaging can guide treatment decisions and improve patient outcomes significantly. They play an essential role in differentiating Fahr’s Syndrome from other neurological conditions that present similar symptoms.
Clinical Evaluation
Clinical evaluation of Fahr’s Syndrome is a crucial step in diagnosis. Healthcare providers begin with a comprehensive medical history, focusing on neurological and psychiatric symptoms.
A detailed physical examination follows. This assesses motor skills, coordination, and cognitive function. Observing patient behavior can provide additional insights into possible underlying issues.
Doctors often inquire about family history to identify potential genetic links. Understanding the patient’s background helps clarify if symptoms are related to Fahr’s or other disorders.
Standardized assessment tools may also be utilized during this process. These tools help quantify symptom severity and monitor changes over time.
In some cases, referrals to specialists such as neurologists or psychiatrists are necessary for further assessment. Collaboration between multiple healthcare experts ensures a thorough understanding of each patient’s unique condition.
Genetic Testing
Genetic testing plays a crucial role in diagnosing Fahr’s Syndrome. By analyzing an individual’s DNA, healthcare professionals can identify specific mutations associated with the condition.
This type of testing is particularly beneficial for families with a history of the syndrome. It allows for early detection and intervention, which can significantly improve quality of life.
The tests often focus on genes linked to calcium metabolism and regulation. Discovering these genetic factors helps establish whether someone is at risk or already affected by the disorder.
In addition, genetic counseling accompanies testing to guide affected individuals and their families through potential implications. Understanding results empowers families to make informed decisions regarding health management and family planning options.
As research progresses, expanding genetic databases may uncover new mutations related to Fahr’s Syndrome, enhancing diagnosis accuracy further.
Differential Diagnosis of Fahr’s Syndrome
Differential diagnosis of Fahr’s Syndrome is essential for accurate treatment and management. Several conditions may present similar symptoms or neuroimaging findings.
Other calcification disorders, such as pseudohypoparathyroidism, should be considered first. These can involve abnormal calcium deposits but vary in their underlying mechanisms.
Neurodegenerative diseases like Alzheimer’s or Parkinson’s disease must also be ruled out. Although they primarily affect cognitive function and movement, overlapping symptoms may lead to confusion in diagnosis.
Metabolic disorders represent another category that requires careful evaluation. Conditions affecting calcium metabolism, such as hyperparathyroidism, can mimic the neurological presentation seen in Fahr’s Syndrome.
A thorough clinical assessment combined with advanced imaging techniques aids healthcare providers in distinguishing between these complex conditions effectively.
Other Calcification Disorders
Calcification disorders encompass a range of conditions characterized by abnormal calcium deposits in various tissues. These abnormalities can lead to significant health issues, affecting organ function and overall well-being.
Among these disorders, idiopathic basal ganglia calcification (IBGC) shares similarities with Fahr’s Syndrome. Like Fahr’s, IBGC involves calcium buildup in the brain’s basal ganglia but may have distinct genetic or environmental triggers.
Another condition is metastatic calcification, where excess calcium from the bloodstream deposits in organs like kidneys or lungs due to systemic imbalances. This differs significantly from localized deposition seen in Fahr’s Syndrome.
Additionally, conditions such as primary hyperparathyroidism and Williams syndrome also exhibit calcifications but present unique clinical features that help differentiate them from Fahr’s. Understanding these differences is crucial for accurate diagnosis and effective management of each disorder.
Neurodegenerative Diseases
Neurodegenerative diseases encompass a range of disorders characterized by progressive degeneration of the nervous system. These conditions lead to the gradual loss of structure and function in neurons, affecting cognitive abilities, motor skills, and overall neurological health.
Conditions such as Alzheimer’s disease, Parkinson’s disease, and Huntington’s disease are some well-known examples. Each disorder presents unique symptoms but shares common features like memory decline or movement difficulties.
Fahr’s Syndrome can sometimes be mistaken for these neurodegenerative illnesses due to overlapping symptoms. The presence of brain calcifications may further complicate diagnosis when similar presentations occur.
Understanding how Fahr’s interacts with other neurodegenerative diseases is crucial for proper management. It aids clinicians in developing treatment strategies tailored specifically to each patient’s needs while fostering better outcomes through comprehensive care plans.
Metabolic Disorders
Metabolic disorders encompass a variety of health conditions that disrupt normal metabolic processes. These can lead to abnormal levels of certain substances in the body, including calcium and phosphorus, which are crucial for bone and brain health.
In patients with Fahr’s Syndrome, disruptions in calcium metabolism may contribute to the deposition of calcifications in the brain. This abnormal buildup can result from various metabolic issues, such as hyperparathyroidism or hypoparathyroidism.
Moreover, imbalances in phosphate levels also play a role. High or low phosphate values might affect neurological function and exacerbate symptoms associated with Fahr’s Syndrome.
Understanding these connections is essential for developing effective treatment plans. Monitoring metabolic parameters can provide insights into managing symptoms and preventing complications related to both Fahr’s Syndrome and underlying metabolic disorders.
Fahr’s Syndrome Treatment Approaches
Fahr’s Syndrome treatment focuses primarily on symptom management, as there is currently no cure for the condition. Neurologists often develop individualized care plans tailored to each patient’s needs.
Symptomatic management involves addressing specific neurological issues, such as seizures or movement disorders. Patients may benefit from physical therapy and occupational therapy to enhance their quality of life.
Medications can also play a crucial role in alleviating symptoms related to mood and behavioral changes. Antidepressants or antipsychotics might be prescribed based on individual assessments.
Supportive care is essential for maintaining daily functioning. Involving caregivers and family members in the treatment process helps create a supportive environment that fosters emotional well-being. Regular monitoring by healthcare professionals ensures that adjustments can be made as needed throughout the disease’s progression.
Symptomatic Management
Symptomatic management of Fahr’s Syndrome focuses on alleviating the diverse neurological and psychiatric symptoms that patients experience. Given the complexity of this condition, a tailored approach is essential.
Physical therapy is often recommended to help maintain mobility and improve coordination. Occupational therapy can assist with daily living activities, enabling individuals to manage their routines more effectively.
For managing mood disorders or anxiety, psychotherapy may be beneficial. Cognitive-behavioral techniques can provide coping strategies for emotional challenges.
Medications might also play a role in treatment. Antidepressants or antipsychotic drugs are sometimes prescribed based on individual symptom profiles.
Regular follow-ups with healthcare providers ensure that any changes in symptoms are addressed promptly. This ongoing care fosters better quality of life for those affected by Fahr’s Syndrome, making it crucial for effective management.
Medications for Specific Symptoms
When addressing Fahr’s Syndrome, medications can be tailored to manage specific symptoms effectively. Antidepressants may be prescribed for individuals experiencing mood disorders. These drugs help balance chemicals in the brain and improve overall emotional well-being.
For movement disorders, dopaminergic agents could enhance motor function. Medications such as levodopa are often utilized to alleviate rigidity and tremors that can arise from basal ganglia dysfunction.
Additionally, anti-anxiety medications might provide relief for those facing heightened anxiety or stress due to their condition. Benzodiazepines serve this purpose but must be used cautiously due to potential dependency issues.
Seizure management is another crucial aspect of treatment. Anti-epileptic drugs like carbamazepine or lamotrigine can help control seizures linked with Fahr’s Syndrome.
Each medication choice should involve careful consideration by healthcare providers based on individual patient needs and responses.
Supportive Care
Supportive care is crucial for individuals living with Fahr’s Syndrome. It focuses on enhancing quality of life and managing symptoms rather than attempting to cure the condition.
Physical therapy plays a significant role. Tailored exercises can help improve mobility, balance, and coordination, which are often affected by movement disorders associated with this syndrome.
Occupational therapy aids in daily activities. Therapists work with patients to develop strategies that foster independence in tasks such as dressing or cooking.
Psychological support is equally important. Counseling services can assist patients in coping with emotional challenges and mood changes stemming from neurological impacts.
Additionally, patient education empowers families to better understand the disease. Knowledge about Fahr’s Syndrome fosters an environment of support and encourages open communication among family members. Adaptive technologies may also be introduced to enhance everyday functioning while prioritizing comfort and safety at home.
Fahr’s Syndrome Prognosis and Disease Progression
Fahr’s Syndrome presents a variable prognosis that can be challenging to predict. While some individuals experience mild symptoms, others may face significant neurological decline over time.
The rate of disease progression often depends on the extent and location of calcifications within the brain. Those with more extensive deposits tend to exhibit severe impairments in motor skills and cognition.
Several factors influence long-term outcomes, including age at onset, overall health, and genetic background. Younger patients may retain greater functionality compared to those diagnosed later in life.
Life expectancy varies widely among patients, with many living into their senior years despite symptoms. However, awareness of individual manifestations is essential for tailored care approaches aimed at enhancing quality of life throughout various stages of the disease process.
Long-term Outlook
The long-term outlook for individuals with Fahr’s Syndrome can vary significantly. Some patients experience a relatively stable condition, while others may face progressive neurological decline. The degree of brain calcification often correlates with symptom severity.
Early diagnosis and intervention play crucial roles in managing the disease’s impact. Regular monitoring allows healthcare providers to adjust treatment plans effectively as symptoms evolve.
Cognitive decline may occur over time, but some individuals maintain good quality of life with appropriate support systems in place.
Social interactions and engaging activities contribute positively to mental health, fostering resilience despite challenges posed by the syndrome. Family involvement also enhances emotional well-being.
Research continues to explore better understanding and management options for Fahr’s Syndrome, offering hope for advancements that could improve patient outcomes in the future.
Factors Affecting Prognosis
The prognosis for individuals with Fahr’s Syndrome can vary significantly based on a number of factors. One major element is the age at which symptoms first appear. Early onset cases often lead to more severe neurological deficits compared to those diagnosed later in life.
Another critical factor is the extent and location of calcium deposits within the brain. Specific regions affected may correlate with distinct cognitive or motor challenges, influencing overall functionality.
Genetic factors also play a role in disease progression. Mutations associated with familial forms may lead to different outcomes than sporadic cases, which tend to have less predictable trajectories.
Comorbid conditions such as psychiatric disorders or metabolic issues can further complicate an individual’s health status, potentially diminishing quality of life and care options available. Each patient’s situation requires careful assessment for tailored management strategies that address unique needs and circumstances.
Life Expectancy Considerations
Life expectancy in individuals with Fahr’s Syndrome can be variable. It largely depends on the severity of neurological symptoms and accompanying complications. Some patients may live normal lifespans, while others experience progressive decline.
The presence of significant movement disorders or severe psychiatric symptoms can impact daily functioning and overall health. These factors often lead to increased risk of accidents or secondary health issues, which could shorten life expectancy.
Additionally, comorbid conditions such as seizures or metabolic abnormalities play a crucial role in determining longevity. Regular monitoring and management are essential for addressing these challenges.
Supportive care is vital for enhancing quality of life and potentially improving outcomes. A tailored approach focusing on individual needs helps maximize functionality in everyday tasks while promoting emotional well-being.
Fahr’s Syndrome Genetic Counseling
Genetic counseling plays a crucial role for families affected by Fahr’s Syndrome. Understanding inheritance patterns is essential for those with a family history of the condition. This syndrome often follows an autosomal dominant pattern, meaning only one copy of the altered gene from either parent can increase the risk.
For prospective parents, genetic counseling provides valuable insights into potential risks and outcomes. Counselors can discuss options like prenatal testing or carrier screening to assess whether future children may inherit the disorder.
In addition, family members might consider genetic testing to determine their own risk levels. Identifying carriers within the family helps tailor monitoring and preventive strategies tailored to individual needs.
Counseling sessions also address emotional support and decision-making processes related to familial implications of Fahr’s Syndrome. The aim is not just information but empowering families with choices that suit their circumstances and aspirations.
Inheritance Patterns
Fahr’s Syndrome often exhibits an autosomal dominant inheritance pattern. This means that a single copy of the mutated gene, inherited from one parent, can lead to the condition in offspring.
However, not every case is linked to family history. Some individuals experience sporadic cases without any known genetic predisposition. These instances may arise due to new mutations occurring during development or other unrecognized factors.
Genetic variations play a crucial role in how Fahr’s Syndrome manifests. Different mutations can affect symptom severity and onset age among affected individuals within the same family.
Understanding these patterns helps families assess their risk for future generations and informs medical professionals about potential treatment options tailored to specific genetic contexts. Proper identification of inheritance patterns could also guide efforts in genetic counseling for families impacted by this rare disorder.
Family Planning Considerations
When considering family planning with a history of Fahr’s Syndrome, it is crucial to consult a genetic counselor. This professional can provide insights into the inheritance patterns associated with the condition.
Understanding whether Fahr’s Syndrome has a hereditary component in your family informs reproductive choices. If a parent carries known genetic mutations, there may be risks for future children.
Couples may explore options such as preimplantation genetic diagnosis (PGD) during in vitro fertilization (IVF). This technique allows for the selection of embryos without the disorder before implantation.
Additionally, discussing potential prenatal testing provides further clarity on any health concerns that might arise during pregnancy. This proactive approach can empower families to make informed decisions while preparing for various outcomes related to Fahr’s Syndrome and its implications.
Genetic Testing for Family Members
Genetic testing for family members of individuals diagnosed with Fahr’s Syndrome can provide valuable insights. It helps identify whether relatives carry genetic mutations associated with the condition.
This testing is particularly relevant if there is a known family history of the syndrome or related disorders. The results can guide decisions about monitoring and preventive measures.
Understanding inheritance patterns is key. Since Fahr’s Syndrome may follow an autosomal dominant pattern, affected individuals have a 50% chance of passing on the gene to their offspring.
Family members may benefit from counseling prior to testing. This ensures they are well-informed about potential outcomes and implications for their health.
Early detection through genetic testing can facilitate timely intervention strategies, improving overall care management for those at risk.
Living with Fahr’s Syndrome
Living with Fahr’s Syndrome can present significant challenges. Individuals may experience various neurological and psychiatric symptoms that impact daily life.
Coping strategies are essential for managing these difficulties. Support groups can offer a sense of community, allowing individuals and families to share experiences and resources. These connections often alleviate feelings of isolation.
Adaptive technologies also play a vital role in enhancing independence. For example, speech recognition software or mobility aids can make everyday tasks more manageable.
Regular communication with healthcare professionals ensures ongoing support tailored to individual needs. This proactive approach helps address both physical and emotional well-being effectively.
Encouraging family involvement fosters understanding of the condition while providing emotional backing for those affected by Fahr’s Syndrome. Building strong support networks is invaluable in navigating this journey together.
Coping Strategies
Coping with Fahr’s Syndrome can be challenging for both patients and caregivers. Developing a strong support network is essential. Connecting with others who understand the condition fosters emotional resilience.
Mindfulness and relaxation techniques can significantly reduce anxiety levels. Activities such as yoga, meditation, or deep-breathing exercises help individuals manage stress effectively.
Establishing a daily routine promotes stability. Consistent schedules for meals, medication, and activities create predictability in life. This structure benefits mental well-being.
Engaging in social activities also plays a vital role. Participating in community events or joining support groups provides opportunities for connection and shared experiences.
Maintaining open communication with healthcare providers allows for tailored coping strategies that address specific needs while adapting to new challenges over time.
Adaptive Technologies
Adaptive technologies play a crucial role in enhancing the quality of life for individuals living with Fahr’s Syndrome. These tools are designed to assist with daily activities and improve independence.
For those facing mobility challenges, devices such as walkers or wheelchairs can significantly aid movement. Smart home systems also offer convenience by allowing users to control lights, temperature, and security through voice commands or mobile apps.
Cognitive aids like specialized software applications help manage memory issues or cognitive impairments. Many programs focus on reminders for medications and appointments, promoting better health management.
Communication devices are essential too. Augmentative and alternative communication (AAC) devices support individuals who may struggle with speech, facilitating more effective interactions with caregivers and loved ones.
By incorporating adaptive technologies into everyday routines, individuals affected by Fahr’s Syndrome can achieve greater autonomy while navigating their unique challenges.
Research and Clinical Trials
Research into Fahr’s Syndrome has gained momentum in recent years. Scientists are delving deeper into the underlying mechanisms of calcium deposition in the brain. This focus aims to uncover potential therapeutic targets.
Current studies explore various genetic and environmental factors contributing to the syndrome. Researchers are investigating how these elements interact, which may lead to better understanding and treatment options.
Clinical trials play a crucial role in advancing knowledge about Fahr’s Syndrome. These trials evaluate new medications and therapies aimed at alleviating symptoms or slowing disease progression. Involvement in such studies can provide patients access to cutting-edge approaches that may not be widely available yet.
Collaboration among institutions is vital for success. Multidisciplinary teams work together, sharing insights that enhance overall research efforts. As this field evolves, it holds promise for improved patient outcomes through innovative treatments and strategies tailored specifically for those affected by Fahr’s Syndrome.
Current Research Directions
Current research on Fahr’s Syndrome is focused on understanding the underlying mechanisms of calcium deposition in the brain. Scientists are investigating why certain regions are more susceptible to calcification and what genetic factors contribute to this process.
Another area of interest includes exploring potential therapeutic approaches. Researchers are evaluating medications that may help alleviate symptoms or slow disease progression. These studies aim to provide patients with better management options.
Additionally, advancements in neuroimaging techniques continue to enhance our understanding of Fahr’s Syndrome. Improved imaging can lead to earlier diagnosis and more accurate tracking of disease progression over time.
Collaborative efforts among institutions also aim at forming registries for better data collection, which could pave the way for future clinical trials targeting specific aspects of the syndrome. As knowledge grows, so does hope for innovative treatments tailored specifically for those affected by this condition.
Ongoing Clinical Studies
Ongoing clinical studies focused on Fahr’s Syndrome aim to deepen our understanding of this rare condition. Researchers are examining the biological mechanisms behind brain calcifications and their neurological consequences.
One significant area of investigation involves genetic analysis. These studies assess familial patterns, looking for potential mutations that could lead to better diagnostic techniques or targeted therapies.
Additionally, researchers explore various treatment modalities in clinical trials. These include medication regimens specifically designed to manage symptoms like mood disorders and movement issues commonly associated with the syndrome.
Collaboration among institutions is essential for these endeavors. By pooling resources and expertise, scientists hope to accelerate discoveries related to prognosis and effective management strategies for patients with Fahr’s Syndrome. This collective effort may contribute significantly toward improved quality of life for affected individuals and their families.
Potential Future Treatments
Research into Fahr’s Syndrome is evolving, opening doors to potential future treatments. One promising area involves targeted therapies that address the underlying mechanisms of calcium deposition in the brain.
Gene therapy may also emerge as a viable option. By correcting genetic mutations linked to the condition, researchers hope to halt or even reverse calcification processes.
Pharmacological advancements are underway too. New medications aimed at regulating calcium and phosphate metabolism could significantly alter disease progression.
Additionally, lifestyle interventions focusing on diet and exercise might complement other treatment modalities. These strategies can help manage symptoms while improving overall quality of life for affected individuals.
Clinical trials continue to explore these possibilities. Participation in such studies not only contributes valuable data but also offers patients access to cutting-edge therapies previously unavailable.
Pediatric Fahr’s Syndrome
Pediatric Fahr’s Syndrome presents unique challenges compared to its adult counterparts. Early-onset cases can manifest in children with distinct symptoms, often complicating diagnosis.
Symptoms may include cognitive delays and developmental milestones that lag behind peers. Parents might notice behavioral changes sooner than the more severe neurological impacts associated with this syndrome.
Detection typically involves neuroimaging studies like MRI or CT scans, which reveal calcifications in specific brain areas. These structural abnormalities help differentiate it from other pediatric disorders.
Management requires a tailored approach since children’s needs vary widely based on age and symptom severity. Close monitoring by healthcare professionals familiar with both neurology and pediatrics is crucial for effective care strategies.
Understanding the implications of early diagnosis leads to better coping mechanisms for families facing this condition. Ongoing research aims to shed light on treatment options specifically designed for younger patients living with Fahr’s Syndrome.
Early-Onset Cases
Early-onset Fahr’s Syndrome refers to cases where symptoms manifest during childhood or adolescence. These instances, although rare, can be particularly challenging for families and healthcare providers.
Children with early-onset Fahr’s may display a range of neurological issues. Cognitive delays are often observed alongside motor difficulties. This can impact their ability to perform everyday tasks.
Diagnosis in younger patients requires careful neuroimaging studies. The characteristic brain calcifications must be identified clearly to differentiate it from other conditions that present similar symptoms.
In addition to neurological impacts, psychiatric manifestations might emerge at an early age. Mood swings, anxiety, or behavioral changes can complicate the clinical picture further.
Treatment approaches for young patients focus on managing symptoms effectively while supporting developmental milestones. Early intervention is crucial in optimizing outcomes and enhancing quality of life as they grow older.
Developmental Considerations
Developmental considerations in pediatric Fahr’s Syndrome highlight the unique challenges faced by affected children. Early-onset cases can manifest significant neurological and cognitive impairments, impacting learning and social interactions.
Children may exhibit developmental delays that necessitate early intervention strategies. These interventions are crucial for improving their quality of life and enhancing overall development.
Parents often report concerns regarding motor skills, language acquisition, and emotional regulation. Tailored therapies focusing on speech, occupational therapy, and physical activity can promote growth in these areas.
Additionally, monitoring for psychiatric symptoms is essential as they may emerge during adolescence when developmental changes occur rapidly. Addressing these issues early can help mitigate potential long-term effects on mental health.
Regular follow-ups with specialists can ensure that both medical needs and educational support are adequately met throughout their formative years.
Neuropsychiatric Aspects of Fahr’s Syndrome
Fahr’s Syndrome is not just a neurological condition; it also profoundly impacts mental health. Patients often experience cognitive impairments that can affect memory, attention, and executive functioning. This decline can make everyday tasks challenging and frustrating.
Mood disorders are common in those with Fahr’s Syndrome. Depression and anxiety may arise due to both the disease’s physical manifestations and the emotional toll of living with chronic illness. Behavioral changes can further complicate relationships with family members and friends.
Additionally, individuals might exhibit irritability or personality shifts, making social interactions difficult. Understanding these neuropsychiatric aspects is crucial for comprehensive care.
Tailoring treatment plans to address both neurological symptoms and psychiatric needs fosters better outcomes for patients navigating this complex syndrome. Multidisciplinary approaches involving neurologists, psychiatrists, and therapists are vital for holistic management of Fahr’s Syndrome.
Cognitive Impairments
Cognitive impairments are a notable aspect of Fahr’s Syndrome. Patients often experience difficulties with memory, attention, and executive functions. These challenges can significantly affect daily life.
Memory issues may manifest as trouble recalling recent events or learning new information. Individuals might find it hard to focus on tasks or switch between activities efficiently. This decline in cognitive flexibility can lead to frustration and confusion.
Moreover, executive function deficits can hinder decision-making and problem-solving abilities. Everyday choices may become overwhelming for those affected by the syndrome.
These cognitive changes can vary widely from person to person, making personalized care essential. Early recognition of these symptoms is vital for implementing supportive strategies that enhance quality of life for patients with Fahr’s Syndrome.
Mood Disorders
Mood disorders are a significant aspect of Fahr’s Syndrome. Individuals affected by this condition may experience fluctuations in their emotional well-being.
Depression is common among patients, often manifesting as persistent sadness and fatigue. This can impact daily functioning and relationships.
Anxiety also surfaces frequently, leading to heightened feelings of worry or fear. These emotions can create barriers to engaging in social activities or pursuing interests.
Some individuals might encounter mood swings that shift dramatically from one extreme to another. Such instability complicates the management of both personal and professional life.
Recognizing these symptoms early ensures timely intervention. Mental health support becomes crucial for improving quality of life for those living with Fahr’s Syndrome, fostering resilience against emotional challenges.
Behavioral Changes
Behavioral changes in individuals with Fahr’s Syndrome can be subtle yet impactful. These alterations may manifest as shifts in personality or mood, leading to increased irritability or emotional instability.
Patients often experience a decline in social interactions. They might withdraw from friends and family, showing less interest in previously enjoyed activities. This isolation can exacerbate feelings of loneliness and frustration.
In some cases, impulsivity increases. Individuals may engage in risky behaviors without fully considering the consequences. This unpredictability can strain relationships and complicate daily life.
Cognitive impairments associated with Fahr’s Syndrome also contribute to behavioral changes. Difficulty concentrating or processing information can lead to misunderstandings and conflicts, further affecting social dynamics.
Monitoring these shifts is crucial for caregivers and healthcare providers alike. Understanding the nuances of these behavioral transformations helps tailor supportive interventions that enhance quality of life.
Metabolic Abnormalities
Metabolic abnormalities play a significant role in Fahr’s Syndrome, particularly concerning calcium and phosphate metabolism. Dysregulation can lead to excessive calcium deposition in the brain, contributing to neurological dysfunction.
Endocrine dysfunctions are also common among individuals with Fahr’s Syndrome. Hormonal imbalances may further exacerbate metabolic irregularities, impacting overall health and well-being.
Nutritional considerations cannot be overlooked either. A balanced diet is essential for managing symptoms associated with this condition. Specific nutrients might aid in maintaining better metabolic function and supporting cognitive health.
Monitoring these metabolic aspects is crucial for comprehensive care management. Addressing nutritional needs alongside hormonal balance can improve quality of life for those affected by Fahr’s Syndrome. The interplay between metabolism and neurological health remains an area ripe for exploration in research and clinical practice.
Calcium and Phosphate Metabolism
Calcium and phosphate metabolism plays a crucial role in maintaining overall health, particularly within the nervous system. These minerals are essential for numerous physiological functions, including bone formation and neuronal signaling.
In Fahr’s Syndrome, abnormalities in calcium and phosphate levels can lead to pathological calcifications in the brain. Disruptions in normal metabolic processes may result from genetic factors or environmental influences, causing an imbalance that affects mineral homeostasis.
The regulation of these minerals involves various hormones such as parathyroid hormone (PTH) and vitamin D. When these regulatory mechanisms fail, excess calcium may precipitate into tissues where it shouldn’t accumulate.
Understanding how alterations in calcium and phosphate metabolism contribute to Fahr’s Syndrome is vital for researchers seeking effective treatments. It sheds light on potential therapeutic targets aimed at restoring balance within this delicate system.
Endocrine Dysfunctions
Endocrine dysfunction is a notable aspect of Fahr’s Syndrome. This condition can disrupt hormonal balance, leading to various health issues. The brain calcifications associated with Fahr’s Syndrome may interfere with the hypothalamus and pituitary gland’s regulation.
These disruptions can manifest in multiple ways. One common outcome is thyroid dysfunction, which might cause fatigue, weight changes, or temperature sensitivity. Additionally, adrenal insufficiency could occur, affecting stress response and energy levels.
Patients may also experience altered calcium metabolism due to parathyroid involvement. Abnormal calcium levels can lead to bone pain or kidney stones.
Hormonal imbalances further complicate the clinical picture for individuals living with this syndrome. Addressing these endocrine abnormalities requires a tailored approach that considers each patient’s unique needs and symptoms within their overall treatment plan.
Nutritional Considerations
Nutritional considerations play a vital role in managing Fahr’s Syndrome. Patients often face challenges with dietary habits due to neurological and psychiatric symptoms. It becomes essential to focus on a balanced diet that supports overall brain health.
Incorporating foods rich in antioxidants can help combat oxidative stress, which may be elevated in individuals with this condition. Fruits, vegetables, nuts, and seeds are excellent sources of these protective compounds.
Additionally, calcium and phosphate metabolism is crucial for those affected by Fahr’s Syndrome. A careful balance must be maintained to avoid complications related to abnormal calcifications. Consulting a nutritionist who understands the disorder can guide appropriate food choices while considering individual needs.
Hydration cannot be overlooked either; staying adequately hydrated is important for cognitive function and general well-being. Tailoring nutritional strategies allows patients to enhance their quality of life while addressing specific dietary requirements linked to Fahr’s Syndrome.
Care Management
Effective care management for Fahr’s Syndrome requires a comprehensive and multidisciplinary approach. This ensures that all aspects of the patient’s health are addressed holistically.
A team typically includes neurologists, psychiatrists, physical therapists, and occupational therapists. Each specialist plays a vital role in managing symptoms and improving quality of life.
Regular follow-ups are crucial to monitor disease progression and adjust treatment plans accordingly. Patients may benefit from tailored therapies aimed at reducing neurological symptoms or behavioral issues.
Family involvement is also significant. Educating family members about Fahr’s Syndrome helps them provide better support while understanding the patient’s challenges.
Long-term care planning must consider potential changes in mobility, cognition, and independence levels as the condition progresses. This proactive strategy enhances safety and improves daily living conditions for those affected by this complex syndrome.
Multidisciplinary Team Approach
A multidisciplinary team approach is essential for effective management of Fahr’s Syndrome. This condition requires input from various healthcare professionals to address the diverse challenges faced by patients.
Neurologists play a pivotal role in diagnosing and treating neurological symptoms. They monitor brain health and recommend therapies tailored to individual needs. Psychiatrists assist in managing any psychiatric manifestations, providing counseling and medication options.
Physical therapists contribute significantly through rehabilitation programs aimed at improving mobility and coordination. Occupational therapists help patients adapt their daily routines, enhancing independence.
Nutritionists also have a crucial part to play, guiding dietary choices that support overall health while addressing any metabolic abnormalities related to the syndrome.
This collaborative effort ensures comprehensive care, allowing for better quality of life for those living with Fahr’s Syndrome.
Long-term Care Planning
Long-term care planning for individuals with Fahr’s Syndrome involves a comprehensive approach that takes into account the unique challenges posed by this condition. It is essential to develop a robust support system that includes healthcare professionals, family members, and caregivers.
Setting clear goals for treatment and daily living can enhance quality of life. Regular assessments should be conducted to monitor symptoms and adjust care plans as necessary. This proactive management helps in addressing both neurological and psychiatric needs over time.
Incorporating therapies such as physical therapy, occupational therapy, or speech therapy can aid in maintaining independence longer. Additionally, creating an environment that fosters safety and accessibility is crucial.
Financial planning also plays a significant role. Understanding insurance coverage options and potential out-of-pocket expenses will alleviate some stress associated with long-term care needs.
Support groups offer emotional benefits too; connecting with others facing similar challenges provides valuable insights and coping strategies. Engaging in social activities encourages mental stimulation while combating feelings of isolation.
Careful planning ensures individuals with Fahr’s Syndrome receive the best possible care throughout their lives. By prioritizing their health needs alongside personal aspirations, families can create fulfilling experiences despite the complexities of this syndrome.