Eisenmenger Syndrome is a complex and often misunderstood condition that arises from congenital heart defects. It can lead to serious complications, including pulmonary hypertension and significant changes in oxygen flow throughout the body. Understanding this syndrome is crucial not only for healthcare professionals but also for patients and families affected by it.
As more people live longer with congenital heart diseases, awareness of Eisenmenger Syndrome is increasingly important. This comprehensive guide will take you through the intricacies of diagnosis, treatment options, symptoms to watch out for, and how to manage life post-diagnosis. Whether you’re seeking information for yourself or a loved one, you’ll find valuable insights here that aim to shed light on this challenging health issue. Join us as we explore the pathophysiology behind Eisenmenger Syndrome and equip you with knowledge that can make a difference in managing this condition effectively.
What is Eisenmenger Syndrome?
Eisenmenger Syndrome is a serious condition that occurs when congenital heart defects lead to high blood pressure in the lungs. This syndrome results from a long-standing left-to-right shunt, where oxygen-poor blood bypasses the lungs and mixes with oxygen-rich blood.
As pulmonary hypertension develops, it reverses this flow, creating a right-to-left shunt. Consequently, deoxygenated blood enters systemic circulation, causing cyanosis—a bluish tint of the skin due to low oxygen levels.
“What Causes Cat Eye Syndrome? Chromosome 22 Guide”
Historically, Eisenmenger Syndrome was often considered terminal. However, advancements in medical care have improved life expectancy for those affected. Understanding its origins and implications is essential for effective management and treatment options. The impact on daily living can be profound; thus awareness remains crucial for patients and healthcare providers alike.
Eisenmenger Syndrome Definition and Overview
Eisenmenger Syndrome is a complex and serious condition that arises from untreated congenital heart defects. It occurs when there is a significant left-to-right shunt, allowing blood to flow abnormally between the chambers of the heart. Over time, this leads to increased pressure in the lungs’ blood vessels, causing pulmonary hypertension.
As a result, the body may adapt by developing right-to-left shunts. This abnormality causes deoxygenated blood to enter systemic circulation, leading to cyanosis—a bluish discoloration of the skin due to low oxygen levels.
“How Does Charcot-Marie-Tooth Disease Affect Nerves?”
Diagnosis typically happens later in life as symptoms progress. It’s important for individuals with congenital heart conditions to be monitored closely for signs of Eisenmenger Syndrome. Understanding this syndrome can help patients receive timely interventions and improve their quality of life significantly.
Historical Context
Eisenmenger Syndrome has a rich historical background that traces back to its discovery in the early 20th century. Initially, physicians recognized congenital heart defects but struggled to understand their long-term implications.
In 1897, Dr. Victor Eisenmenger first described the condition associated with congenital heart defects leading to pulmonary vascular disease and cyanosis. His groundbreaking observations paved the way for future research into this complex syndrome.
Throughout the decades, advances in medical technology have enhanced our understanding of Eisenmenger Syndrome. The development of echocardiography and cardiac catheterization allowed for better diagnosis and monitoring.
“Why Does Chronic Fatigue Syndrome Cause Persistent Tiredness?”
As awareness grew, so did the recognition of how untreated congenital heart defects could lead to severe complications like pulmonary hypertension. This knowledge shifted treatment approaches significantly over time, emphasizing early intervention and management strategies.
Pathophysiology of Eisenmenger Syndrome
Eisenmenger Syndrome primarily arises from congenital heart defects that create an abnormal communication between the heart’s chambers. These defects often lead to a left-to-right shunt, where oxygen-rich blood is incorrectly directed into the pulmonary circulation. Over time, this increased flow can cause significant damage to the lungs.
As pressure builds in the pulmonary arteries, it leads to pulmonary hypertension. This condition forces blood to reroute through a right-to-left shunt due to elevated pressures in the right side of the heart surpassing those on the left.
“What Triggers Cushing’s Syndrome? Complete Hormone Guide”
The result is systemic hypoxemia and cyanosis as deoxygenated blood enters systemic circulation. Understanding these processes helps in early diagnosis and management, crucial for improving patient outcomes with Eisenmenger Syndrome.
Congenital Heart Defects
Congenital heart defects (CHDs) are structural abnormalities of the heart that occur during fetal development. These defects can affect the heart’s walls, valves, or blood vessels.
CHDs range from simple issues, like small holes in the heart, to complex conditions requiring extensive treatment. Their severity often dictates symptoms and potential complications.
In many cases, these defects remain undetected until later in life. Some individuals may experience no symptoms at all for years. Others might have noticeable signs early on, including difficulty breathing or poor growth rates in infants.
“How Does Carpal Tunnel Syndrome Develop? Prevention Tips”
Factors contributing to CHDs include genetic predispositions and environmental influences such as maternal infections or substance use during pregnancy. Understanding these underlying causes is crucial for managing patients with Eisenmenger Syndrome effectively since many cases stem from untreated congenital conditions.
Pulmonary Hypertension
Pulmonary hypertension is a key factor in Eisenmenger Syndrome. It refers to elevated blood pressure in the pulmonary arteries, which can lead to serious complications.
When congenital heart defects cause increased blood flow to the lungs, this puts extra strain on these vessels. Over time, they thicken and stiffen, resulting in restricted blood flow.
Patients often experience symptoms like shortness of breath and fatigue due to reduced oxygen levels. The heart must work harder to pump blood through narrowed vessels, eventually leading to right-sided heart failure.
“What Makes Cauda Equina Syndrome a Medical Emergency?”
Management of pulmonary hypertension is crucial for improving quality of life and extending survival rates. Treatment options vary but may include medications aimed at relaxing the pulmonary arteries or reducing pressure within them.
Ongoing research continues to evolve our understanding of this complex condition, promising new therapies that target its underlying mechanisms.
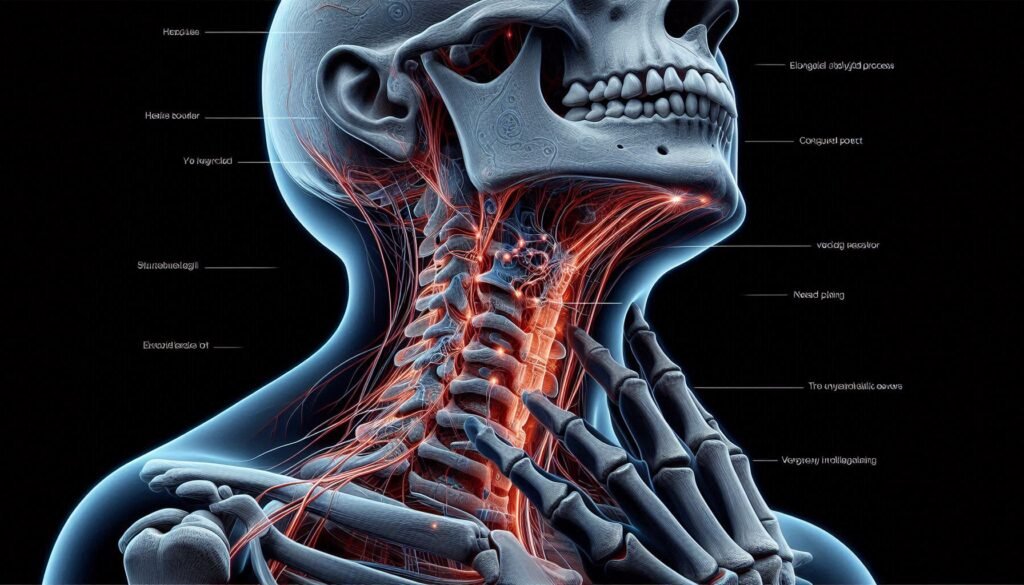
Right-to-Left Shunt
A right-to-left shunt occurs when blood flows from the right side of the heart to the left, bypassing the lungs. This abnormal flow results in deoxygenated blood entering systemic circulation.
This condition often arises from congenital heart defects, such as ventricular septal defects or tetralogy of Fallot. These structural abnormalities create pathways that allow unoxygenated blood to mix with oxygen-rich blood.
The implications of a right-to-left shunt can be severe. Patients may experience significant cyanosis due to reduced oxygen levels in their bloodstream. As a result, they might struggle with symptoms like fatigue and shortness of breath during physical activities.
Understanding this mechanism is crucial for diagnosing Eisenmenger Syndrome since it directly contributes to the development of pulmonary hypertension and other complications related to this condition.
Eisenmenger Syndrome Causes and Risk Factors
Eisenmenger Syndrome primarily arises from underlying congenital heart defects. Conditions such as atrial septal defects or ventricular septal defects can lead to abnormal blood flow between the heart chambers. Over time, this causes increased pressure in the pulmonary arteries.
Genetic factors also play a significant role. Certain inherited conditions can predispose individuals to develop congenital heart issues that may eventually evolve into Eisenmenger Syndrome.
Environmental influences cannot be overlooked either. Maternal health during pregnancy, exposure to toxins, and infections like rubella are known risk factors. These elements might contribute to fetal heart development problems that manifest later in life.
Understanding these causes is essential for early diagnosis and intervention strategies tailored to minimize complications associated with Eisenmenger Syndrome.
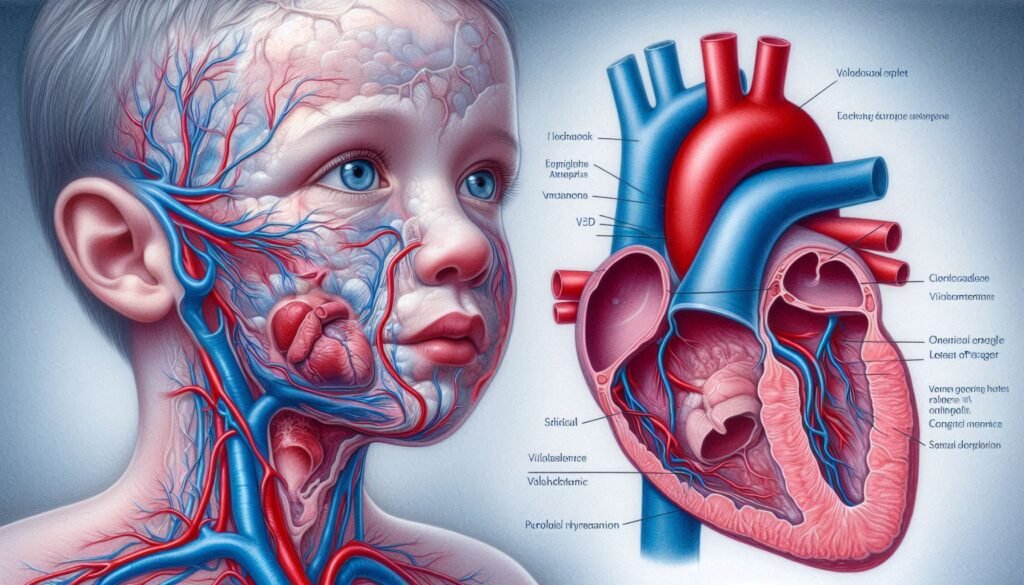
Underlying Cardiac Defects
Underlying cardiac defects are the primary culprits behind Eisenmenger Syndrome. These congenital conditions lead to abnormal heart structures that disrupt normal blood flow.
Common defects include ventricular septal defects (VSD) and atrial septal defects (ASD). Both create openings in the heart walls, allowing blood to shunt between chambers. This improper mixing of oxygenated and deoxygenated blood can escalate pressure in the pulmonary arteries over time.
Another notable defect is patent ductus arteriosus (PDA), where a fetal connection fails to close after birth. The continued passage of blood through this duct increases workload on the lungs.
The severity of these underlying issues significantly influences patient outcomes. Early recognition and management are crucial for preventing progression to more severe complications like Eisenmenger Syndrome. Understanding these foundational heart problems aids healthcare providers in developing effective treatment strategies tailored to each patient’s needs.
Genetic Factors
Genetic factors play a significant role in the development of Eisenmenger Syndrome. Certain congenital heart defects, which are often inherited, can predispose individuals to this condition. Variations in specific genes may influence how the heart forms during fetal development.
Studies suggest that mutations affecting blood vessel formation and regulation can contribute to pulmonary hypertension. Additionally, families with a history of congenital heart disease may have members who develop Eisenmenger Syndrome due to shared genetic traits.
Research continues to explore various genetic markers associated with these conditions. Understanding these links can help identify at-risk populations for early intervention and treatment strategies aimed at preventing severe complications related to Eisenmenger Syndrome.
Environmental Influences
Environmental influences play a significant role in the development of Eisenmenger Syndrome. Factors such as exposure to pollutants and toxins can contribute to lung damage over time. Polluted air, particularly in urban settings, may exacerbate existing pulmonary issues linked with congenital heart defects.
Maternal health during pregnancy is another crucial factor. Infections or complications experienced by the mother can impact fetal development, potentially leading to congenital heart conditions that later progress to Eisenmenger Syndrome.
Additionally, socioeconomic status affects access to healthcare and early diagnosis. Individuals from underprivileged backgrounds may experience delays in receiving appropriate treatment for underlying cardiac anomalies.
The interplay between these environmental elements underscores the complexity surrounding this syndrome. Understanding these influences aids both patients and healthcare providers in managing risks associated with Eisenmenger Syndrome effectively.
Eisenmenger Syndrome Signs and Symptoms
Eisenmenger Syndrome presents a range of distinctive signs and symptoms that can significantly impact daily life. One of the most noticeable is cyanosis, which results in a bluish tint to the skin, lips, and nails due to decreased oxygen levels in the blood.
Individuals often experience dyspnea and fatigue during physical activities. Simple tasks may become exhausting as reduced blood flow hinders oxygen delivery.
Another hallmark symptom is clubbing of fingers and toes. This condition causes bulbous enlargements at the tips of digits, reflecting prolonged low oxygen levels.
Arrhythmias are also common in these patients, leading to irregular heartbeats that can cause palpitations or dizziness. Additionally, hemoptysis—coughing up blood—can occur as pressure builds within pulmonary vessels over time.
These varied symptoms highlight the complexity of Eisenmenger Syndrome and underscore its serious nature for those affected.
Cyanosis
Cyanosis is a key sign of Eisenmenger Syndrome. It manifests as a bluish tint to the skin, lips, and nails. This discoloration occurs due to low oxygen levels in the blood.
As the right-to-left shunt develops, deoxygenated blood enters systemic circulation. The body’s tissues then receive insufficient oxygen. This lack can lead to significant organ dysfunction over time.
The severity of cyanosis often correlates with disease progression. Patients may notice that it worsens during physical activities or stress when oxygen demand increases.
Monitoring this symptom is crucial for managing Eisenmenger Syndrome effectively. It’s an important indicator that requires attention from healthcare providers and caregivers alike.
Dyspnea and Fatigue
Dyspnea, or shortness of breath, is a common symptom in individuals with Eisenmenger Syndrome. This occurs due to increased pressure in the pulmonary arteries, making it difficult for blood to flow efficiently through the lungs. As oxygen levels drop, patients often experience an overwhelming sense of breathlessness during routine activities.
Fatigue accompanies dyspnea as well. The heart struggles to pump oxygen-rich blood effectively throughout the body. Consequently, everyday tasks can feel daunting and exhausting.
Patients may find that even minimal exertion exacerbates these symptoms. Climbing stairs or walking short distances might lead to significant fatigue and feelings of weakness.
Understanding these symptoms is crucial for managing daily life with Eisenmenger Syndrome. Recognizing when rest is needed can help maintain energy levels and improve overall quality of life.
Clubbing of Fingers and Toes
Clubbing of fingers and toes is a notable symptom associated with Eisenmenger Syndrome. This condition manifests as the enlargement and rounding of the fingertips or toes, creating a distinct appearance.
The changes occur due to prolonged low oxygen levels in the blood. When this happens, your body responds by increasing blood flow to certain areas, particularly in the extremities. Over time, these adjustments lead to alterations in bone structure and soft tissue growth at the tips of fingers and toes.
This phenomenon can be alarming for patients and their loved ones. It serves as an important visual indicator that warrants further medical evaluation. Recognizing clubbing early can facilitate timely diagnosis and management of underlying issues related to Eisenmenger Syndrome.
For those affected, understanding this symptom is crucial for monitoring their health effectively.
Arrhythmias
Arrhythmias are a significant concern in patients with Eisenmenger Syndrome. These irregular heartbeats can manifest as palpitations, rapid heart rates, or even skipped beats.
The underlying changes in the heart structure and function due to congenital defects contribute to these electrical disturbances. As pulmonary hypertension worsens, the right ventricle becomes hypertrophied, further complicating its ability to maintain a normal rhythm.
Patients may experience symptoms such as dizziness or fainting spells when arrhythmias occur. Continuous monitoring is crucial for timely intervention.
Treatment options vary based on the type of arrhythmia present and its severity. In some cases, medications like beta-blockers can help manage symptoms and restore regularity. For more severe disruptions, procedures such as catheter ablation might be considered.
Living with arrhythmias requires careful management and often close collaboration between healthcare providers and patients to ensure optimal outcomes.
Hemoptysis
Hemoptysis, or coughing up blood, is a significant symptom associated with Eisenmenger Syndrome. It occurs due to increased pressure in the pulmonary arteries. This elevated pressure can lead to damage and rupture of small blood vessels within the lungs.
Patients may notice streaks of blood in their sputum or larger amounts during coughing episodes. The severity often correlates with the progression of pulmonary hypertension.
While alarming, hemoptysis varies greatly among individuals; some experience it infrequently while others face recurrent episodes. Factors such as infection or exacerbation of heart failure can worsen this condition.
Prompt medical evaluation is essential when experiencing hemoptysis. Identifying its cause ensures appropriate management and prevents further complications related to Eisenmenger Syndrome’s underlying issues. Regular monitoring by healthcare professionals helps maintain lung health and overall well-being for affected patients.
Diagnosis of Eisenmenger Syndrome
Diagnosing Eisenmenger Syndrome involves a comprehensive clinical evaluation. Physicians begin with a detailed medical history and physical examination, focusing on symptoms like cyanosis or shortness of breath.
Echocardiography plays a crucial role in the diagnosis. This imaging technique allows doctors to visualize heart structures and assess blood flow patterns, revealing any congenital defects that could lead to Eisenmenger Syndrome.
Cardiac catheterization is another pivotal diagnostic tool. It provides direct measurement of pressures within the heart and pulmonary arteries, confirming the presence of pulmonary hypertension.
Other imaging techniques such as MRI or CT scans may also be utilized for further assessment. These methods help identify changes in cardiac anatomy and function over time, guiding effective management strategies tailored to each patient’s condition.
Clinical Evaluation
Clinical evaluation is a crucial step in diagnosing Eisenmenger Syndrome. It begins with a comprehensive medical history, where the healthcare provider assesses symptoms and any known congenital heart defects.
During the physical examination, signs of cyanosis may be observed, which indicates low oxygen levels in the blood. This can often reveal underlying issues that require further investigation.
A careful auscultation of the heart might uncover abnormal heart sounds or murmurs indicative of shunts or valvular problems. The presence of clubbing in fingers and toes can also provide valuable diagnostic clues.
It’s essential for clinicians to perform thorough evaluations because early detection significantly impacts management strategies. A well-rounded clinical assessment lays the groundwork for more advanced diagnostic tests, ensuring patients receive timely and appropriate care tailored to their needs.
Echocardiography
Echocardiography is a crucial diagnostic tool for Eisenmenger Syndrome. This non-invasive imaging technique uses sound waves to create detailed images of the heart.
During an echocardiogram, high-frequency sound waves are transmitted through the chest wall. The echoes bounce off heart structures and are captured to produce real-time images. These visuals help assess heart size, structure, and function.
Specifically for Eisenmenger Syndrome, echocardiography can reveal underlying congenital defects. It allows doctors to evaluate blood flow patterns, identify shunts, and measure pressure changes in the chambers of the heart.
Furthermore, Doppler imaging enhances this study by providing information on blood velocities. Clinicians can detect pulmonary hypertension more effectively with these insights. Echocardiography plays a vital role in confirming diagnoses and guiding treatment strategies for patients affected by this complex condition.
Cardiac Catheterization
Cardiac catheterization is a key diagnostic tool for evaluating Eisenmenger Syndrome. This minimally invasive procedure involves threading a thin tube, or catheter, through blood vessels to the heart. It provides crucial insights into the heart’s structure and function.
During the process, doctors can measure pressures in different chambers of the heart and assess blood flow dynamics. This helps identify any abnormalities associated with congenital defects or pulmonary hypertension.
Additionally, cardiac catheterization allows for direct visualization of shunts that may contribute to Eisenmenger Syndrome. By measuring oxygen levels within various parts of the circulatory system, physicians can determine whether there’s a right-to-left shunt present.
Cardiac catheterization plays an essential role in diagnosing this complex condition. The results guide treatment options effectively tailored to each patient’s specific needs.
Other Imaging Techniques
In addition to echocardiography and cardiac catheterization, other imaging techniques play a crucial role in diagnosing Eisenmenger Syndrome. Magnetic Resonance Imaging (MRI) offers detailed insights into the heart’s structure and function without exposing patients to radiation.
CT scans can also be beneficial, particularly for assessing pulmonary vascular anatomy. They help visualize blood flow patterns and any potential blockages that may contribute to complications.
Nuclear medicine studies, such as Positron Emission Tomography (PET), provide information on myocardial perfusion. This technique allows healthcare providers to evaluate how well blood flows through the heart muscle.
Each of these advanced imaging modalities enhances diagnostic accuracy. By combining findings from multiple sources, clinicians can develop a comprehensive understanding of the patient’s condition. This thorough evaluation is essential for guiding appropriate management strategies for those living with Eisenmenger Syndrome.
Eisenmenger Syndrome Management and Treatment
Managing Eisenmenger Syndrome requires a multidisciplinary approach tailored to each patient’s needs. Medical therapy plays a crucial role in alleviating symptoms and improving quality of life.
Pulmonary vasodilators are commonly prescribed to reduce pressure in the pulmonary arteries. These medications help improve oxygen delivery throughout the body, enhancing overall function.
Oxygen therapy can also be beneficial for patients experiencing low blood oxygen levels. It aims to alleviate hypoxia and provide more comfort during daily activities.
Anticoagulation is essential for preventing thromboembolic events, which can occur due to increased blood viscosity in these patients. Regular monitoring ensures that appropriate levels are maintained without increasing bleeding risks.
In severe cases where medical management fails or complications arise, heart-lung transplantation may be considered. This option offers hope for those with progressive disease who experience diminished quality of life due to their condition.
Medical Therapy
Medical therapy for Eisenmenger Syndrome focuses on alleviating symptoms and improving quality of life. While it cannot reverse the underlying heart defect, it plays a critical role in managing complications.
One common approach involves the use of pulmonary vasodilators. These medications help to relax blood vessels in the lungs, reducing pressure and easing strain on the heart.
Diuretics are also frequently prescribed. They assist in removing excess fluid from the body, which can alleviate swelling and reduce workload on the heart.
Additionally, oxygen therapy is beneficial for patients experiencing low oxygen levels. It provides supplemental oxygen to enhance overall saturation and improve symptoms like shortness of breath.
Anticoagulation therapy may be recommended to prevent blood clots. Given that individuals with Eisenmenger Syndrome have increased risks of thromboembolism, these medications can significantly lower those chances.
Pulmonary Vasodilators
Pulmonary vasodilators play a crucial role in managing Eisenmenger Syndrome. These medications help to relax and widen blood vessels in the lungs, which can reduce pulmonary hypertension.
Commonly used pulmonary vasodilators include endothelin receptor antagonists, phosphodiesterase-5 inhibitors, and prostacyclin analogs. Each of these drugs works through different mechanisms but shares the goal of lowering pressure within the pulmonary arteries.
Patients often experience improved exercise capacity and quality of life while on these treatments. However, monitoring is essential due to potential side effects like headaches or gastrointestinal issues.
The choice of a specific vasodilator depends on individual patient needs and overall health status. Regular follow-ups with healthcare providers are necessary for optimal management of symptoms associated with Eisenmenger Syndrome.
Oxygen Therapy
Oxygen therapy plays a crucial role in managing Eisenmenger Syndrome. Patients often experience low oxygen levels due to the right-to-left shunt, which leads to reduced oxygenated blood circulating throughout the body.
By delivering supplemental oxygen, healthcare providers can help improve overall oxygen saturation. This intervention alleviates symptoms like dyspnea and fatigue, enhancing patients’ quality of life.
Administered through various methods—such as nasal cannulas or face masks—oxygen therapy is tailored to individual needs. Regular monitoring ensures that patients receive optimal levels for their condition.
While it does not address the underlying heart defect, this treatment provides significant symptomatic relief. As a result, patients are better equipped to manage daily activities and maintain an improved sense of well-being.
Anticoagulation
Anticoagulation plays a crucial role in managing Eisenmenger Syndrome. As patients with this condition often experience increased blood flow and turbulence, there is a heightened risk of thrombus formation. Anticoagulants help reduce this risk by preventing the clotting process.
Common anticoagulant medications include warfarin, rivaroxaban, and apixaban. Each has its unique mechanism of action and dosing requirements. Regular monitoring is essential to ensure that the patient maintains appropriate levels for effective management while minimizing potential bleeding complications.
It’s important for healthcare providers to assess each patient’s individual risks before initiating therapy. Adjustments may be necessary based on their overall health status or concurrent medications.
Patients should also be educated about signs of bleeding or thrombosis so they can seek medical attention promptly if needed. Adhering to prescribed regimens can significantly impact long-term outcomes in those living with Eisenmenger Syndrome.
Heart-Lung Transplantation
Heart-lung transplantation is a complex surgical procedure primarily reserved for patients with severe Eisenmenger Syndrome and advanced pulmonary hypertension. This operation involves the replacement of both the heart and lungs with matching organs from a deceased donor.
The criteria for eligibility can be stringent, requiring comprehensive evaluations to ensure candidates can tolerate such an extensive surgery. This includes assessments of overall health, organ function, and psychosocial factors.
Post-transplant care is crucial for success. Patients must adhere to lifelong immunosuppressive therapy to prevent organ rejection. Regular follow-ups are essential to monitor heart and lung function along with managing any complications that may arise.
While this procedure offers new hope for individuals suffering from end-stage disease linked to Eisenmenger Syndrome, it also carries risks. Each case requires careful consideration by a multidisciplinary team specializing in transplant medicine.
Complications and Prognosis
Eisenmenger Syndrome can lead to several serious complications. One significant risk is during pregnancy, where there’s an increased chance of maternal and fetal morbidity due to the strain on cardiovascular health.
Thromboembolism is another concern, as the altered blood flow may cause clot formation that could travel to vital organs, resulting in life-threatening situations.
Heart failure often develops as the heart struggles against elevated pressures over time. This can severely impact a patient’s quality of life.
When it comes to prognosis, it varies widely among individuals with Eisenmenger Syndrome. Factors such as age at diagnosis and overall health play critical roles in determining outcomes.
Life expectancy has improved with advances in treatment options; however, many patients still face ongoing challenges related to their condition. Regular monitoring and comprehensive care are essential for managing these complexities effectively.
Pregnancy Risks
Pregnancy presents unique challenges for individuals with Eisenmenger Syndrome. The condition can exacerbate existing heart issues, leading to serious complications during pregnancy.
Increased blood volume and cardiac output demand additional strain on the heart. This can heighten the risk of maternal mortality or significant morbidity. Women may experience worsening pulmonary hypertension as their bodies adapt to pregnancy.
Additionally, oxygen delivery becomes compromised due to right-to-left shunting in Eisenmenger patients. Hypoxia poses risks not only for the mother but also for fetal development and health.
Close monitoring is essential throughout gestation. Cardiac specialists often recommend a multidisciplinary approach involving obstetricians experienced in high-risk pregnancies.
Patients should engage in thorough discussions about family planning options, including potential risks associated with carrying a baby to term. Such decisions are crucial for ensuring both maternal and child safety.
Thromboembolism
Thromboembolism is a serious complication often associated with Eisenmenger Syndrome. It occurs when a blood clot forms in one part of the body and travels to another, potentially blocking blood flow.
In individuals with this syndrome, changes in blood flow dynamics can increase the likelihood of clot formation. The right-to-left shunt allows deoxygenated blood to bypass the lungs, leading to hypoxia and subsequent platelet activation.
Symptoms may vary depending on where the embolism occurs. If it lodges in the lungs, patients may experience sudden shortness of breath or chest pain. Clots that travel to other areas could lead to strokes or organ damage.
Management typically involves anticoagulation therapy to prevent further clot formation. Regular monitoring and prompt treatment are crucial for reducing risks associated with thromboembolism in Eisenmenger Syndrome patients.
Heart Failure due to Eisenmenger Syndrome
Heart failure due to Eisenmenger Syndrome is a serious condition that arises when the heart struggles to meet the body’s demands. This syndrome often develops from congenital heart defects, leading to significant changes in blood flow and pressure.
As pulmonary hypertension progresses, the right ventricle faces increased strain. Over time, this can lead to its enlargement and weakened function, resulting in right-sided heart failure. Symptoms may include swelling in the legs and abdomen, chronic fatigue, and difficulty breathing.
Management of heart failure focuses on alleviating symptoms while addressing underlying issues related to Eisenmenger Syndrome. Regular monitoring by healthcare professionals is vital for adjusting treatment plans as needed.
Patients with this complication must remain vigilant about their health status. Early intervention can significantly improve quality of life despite living with such a challenging condition.
Life Expectancy
Life expectancy for individuals with Eisenmenger Syndrome can vary significantly. Several factors influence this variability, including the severity of the condition and the presence of other health issues.
Many individuals may live into their 40s or even beyond with appropriate management. However, those who experience severe complications often face a more challenging prognosis.
Patients should be proactive in managing their health through regular check-ups and adhering to treatment plans. This approach can help mitigate risks and potentially extend life span.
Advancements in medical research continue to improve outcomes for patients with Eisenmenger Syndrome. New treatments emerge regularly, contributing positively to quality of life and longevity.
It’s essential for patients to remain informed about their condition and engage actively in discussions regarding care options with healthcare providers.
Living with Eisenmenger Syndrome
Living with Eisenmenger Syndrome requires a proactive approach to health and wellness. Patients often need to make lifestyle modifications that support cardiovascular health. This can include following a heart-healthy diet rich in fruits, vegetables, and whole grains while limiting sodium intake.
Exercise is essential but should be tailored to individual capabilities. Engaging in low-impact activities helps maintain fitness without overexertion. Consulting healthcare professionals for personalized exercise plans is crucial.
Regular monitoring of symptoms is vital as well. Keeping track of changes or new symptoms can aid in timely medical intervention.
Support from family and friends plays an important role too. Emotional well-being can significantly impact overall health, so joining support groups may provide comfort and shared experiences among those facing similar challenges.
Staying informed about the condition empowers patients to take charge of their health journey actively.
Lifestyle Modifications
Living with Eisenmenger Syndrome requires thoughtful lifestyle modifications. These changes can significantly improve overall well-being and help manage symptoms effectively.
First, a balanced diet is essential. Focus on whole foods rich in nutrients to support heart health. Limit processed foods, sodium, and unhealthy fats to maintain optimal blood pressure levels.
Regular monitoring of oxygen saturation is crucial. Patients should use pulse oximeters at home to track their oxygen levels and report any significant changes to healthcare providers promptly.
Hydration plays an important role as well. Staying adequately hydrated supports circulation but be cautious about fluid intake if advised by a doctor.
It’s vital to engage in stress-reducing activities. Techniques such as yoga or meditation can foster emotional balance while promoting relaxation and reducing the risk of complications associated with anxiety or stress-related conditions.
Exercise Recommendations
Exercise plays a vital role in managing Eisenmenger Syndrome, but it requires careful consideration. Due to the complexities of this condition, patients should work closely with healthcare providers when developing an exercise plan.
Low-impact activities are typically recommended. Walking, swimming, and cycling can be beneficial while minimizing stress on the heart and lungs. Strength training may also be safe if performed under supervision. It’s crucial to listen to your body; any signs of distress or increased symptoms warrant immediate cessation.
Regular physical activity promotes overall well-being and can improve quality of life for those living with Eisenmenger Syndrome. However, moderation is key. Strenuous exercises or competitive sports can exacerbate symptoms due to the strain they place on cardiovascular function.
Personalized plans that incorporate regular monitoring ensure safety while encouraging active lifestyles for individuals with Eisenmenger Syndrome. Prioritizing health through suitable exercise routines enhances both physical strength and emotional resilience in facing daily challenges associated with this complex condition.