Chronic Fatigue Syndrome (ME/CFS) is a complex and often misunderstood condition that affects millions worldwide. At its core, it manifests as an overwhelming, persistent fatigue that can disrupt daily life in unimaginable ways. Whether it’s struggling to get out of bed or experiencing mental fog during crucial moments, those with ME/CFS face challenges that many cannot comprehend.
Despite its prevalence, the exact causes remain elusive. Medical professionals and researchers are working tirelessly to shed light on this debilitating disorder. As we delve into the intricacies of Chronic Fatigue Syndrome, we’ll explore not just its symptoms but also potential triggers and treatment options available to enhance quality of life for those affected.
Join us as we unravel the mystery surrounding Chronic Fatigue Syndrome (ME/CFS). Understanding this condition better may pave the way for improved support and awareness in both medical communities and society at large.
Defining Chronic Fatigue Syndrome/Myalgic Encephalomyelitis
Chronic Fatigue Syndrome, often referred to as Myalgic Encephalomyelitis (ME/CFS), is a debilitating disorder characterized by extreme fatigue that doesn’t improve with rest. This profound exhaustion can significantly impair daily activities and quality of life.
The complexity of ME/CFS lies in its multifaceted nature. It encompasses a range of symptoms affecting various bodily systems, including cognitive function, sleep patterns, and the immune system.
While fatigue is the hallmark symptom, many individuals experience additional challenges like muscle pain and neurological issues. The unpredictability of these symptoms can make it difficult for patients to maintain a consistent routine.
“What Causes Maffucci Syndrome? Tumor Formation Guide”
Diagnosis remains challenging due to overlapping symptoms with other conditions. As awareness grows about ME/CFS, so does the need for better understanding and recognition within healthcare settings. Continued research aims to clarify this intricate syndrome further.
Prevalence and Demographics of CFS/ME
Chronic Fatigue Syndrome (ME/CFS) affects millions of individuals worldwide. Studies estimate that approximately 836,000 to 2.5 million Americans suffer from this complex disorder.
The condition shows a distinct demographic pattern. Women are diagnosed more frequently than men, with ratios ranging from 2:1 to 4:1 in some studies. This disparity raises questions about biological and social factors influencing prevalence.
Age also plays a role; ME/CFS can affect anyone but is most commonly identified in individuals aged between 30 and 50 years. However, cases have been reported across all age groups, including children and adolescents.
“Why Does MRKH Syndrome Affect Female Development?”
Ethnic background does not appear to significantly influence the likelihood of developing ME/CFS. Nonetheless, access to healthcare resources may vary among different populations, which can impact diagnosis rates and support for those affected by the syndrome.
Potential Causes and Risk Factors
Chronic Fatigue Syndrome (ME/CFS) remains a complex and elusive condition. Researchers have identified several potential causes that may contribute to its onset.
One leading theory involves viral infections. Some individuals report the onset of ME/CFS following illnesses like Epstein-Barr virus or influenza. This suggests a link between viral triggers and long-lasting fatigue.
“How Does Meige Syndrome Cause Facial Spasms?”
Genetic predisposition is another factor worth exploring. Family history may increase susceptibility, indicating an inherited component that warrants further investigation.
Environmental factors also play a role. Exposure to toxins or prolonged stress can disrupt the body’s normal functioning, potentially catalyzing symptoms of ME/CFS in vulnerable populations.
Additionally, hormonal imbalances might be significant contributors. Dysregulation in the endocrine system could affect energy levels and overall health, posing risks for developing chronic fatigue.
Understanding these causes is vital for researchers as they work towards effective treatments and management strategies for those affected by this debilitating syndrome.
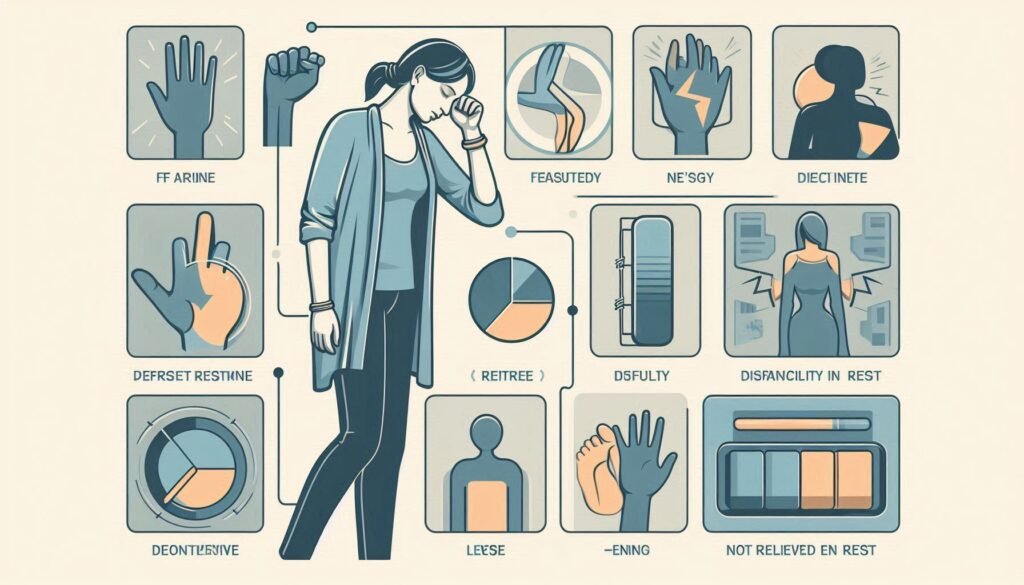
Debilitating Fatigue: The Hallmark Symptom
Debilitating fatigue is the cornerstone of Chronic Fatigue Syndrome (ME/CFS). It differs significantly from ordinary tiredness. While most people can bounce back after rest, those with ME/CFS find that their exhaustion remains unrelenting.
“What Are The Signs of Metabolic Syndrome? Prevention Guide”
This profound fatigue affects both physical and mental functioning. Even simple tasks become monumental challenges. Daily activities, such as showering or grocery shopping, may leave individuals completely drained.
The intensity and impact of this fatigue fluctuate throughout the day. Some may experience brief periods of improvement but often return to a state of overwhelming exhaustion soon after.
Many describe this sensation as an all-consuming heaviness that weighs down every aspect of life. Understanding this hallmark symptom is crucial for recognizing the complexities associated with ME/CFS and supporting those affected by it effectively.
Post-Exertional Malaise (PEM) and Activity Intolerance
Post-Exertional Malaise (PEM) is a defining feature of Chronic Fatigue Syndrome (ME/CFS). Individuals often experience extreme fatigue and worsening symptoms following even minimal physical or mental exertion. This profound exhaustion can last for days, weeks, or longer.
PEM differs significantly from typical tiredness; it’s an exacerbation of pre-existing symptoms rather than simple fatigue recovery. The unpredictability of PEM makes daily life challenging for many affected individuals.
“Why Does Marfan Syndrome Affect Connective Tissue?”
Activity intolerance accompanies PEM, preventing patients from engaging in regular activities. Tasks that were once manageable may become overwhelming obstacles. Even routine chores can lead to debilitating crashes.
Understanding the triggers is vital for those with ME/CFS. Recognizing personal limits helps people avoid overexertion and manage their energy more effectively throughout the day. Maintaining a balance between activity and rest becomes essential in navigating this complex condition.
Cognitive Symptoms: Brain Fog and Memory Issues
Cognitive symptoms are a common and frustrating aspect of Chronic Fatigue Syndrome (ME/CFS). Many individuals report experiencing brain fog, which can manifest as confusion, lack of clarity, or difficulty concentrating. Simple tasks that once came easily may suddenly feel overwhelming.
Memory issues also play a significant role in this condition. Patients often struggle with short-term memory loss or find it hard to recall information they previously knew well. This cognitive decline can hinder daily life activities and affect work performance.
“How Does McCune-Albright Syndrome Affect Bone Growth?”
The impact of these symptoms extends beyond mere frustration; it can lead to feelings of isolation and anxiety. Social interactions may become challenging due to an inability to follow conversations or remember names and faces.
Addressing cognitive symptoms is crucial for managing ME/CFS effectively. Understanding their nature helps both patients and caregivers navigate the complexities associated with this debilitating syndrome more compassionately.
Sleep Disturbances and Non-Restorative Sleep
Sleep disturbances are a defining feature of Chronic Fatigue Syndrome (ME/CFS). Many patients report difficulties falling and staying asleep. This can lead to a cycle of fatigue that exacerbates other symptoms.
Non-restorative sleep is particularly troubling for those with ME/CFS. Even after hours of rest, individuals often wake up feeling unrefreshed or exhausted. This phenomenon disrupts daily functioning and impacts mental clarity.
Research indicates that the quality of sleep suffers significantly in affected individuals. Sleep architecture may be altered, resulting in reduced deep sleep stages crucial for recovery and rejuvenation.
Nighttime awakenings, vivid dreams, or insomnia further complicate the issue. These disruptions prevent the body from engaging in its natural healing processes during sleep cycles.
Addressing these disturbances is essential for managing ME/CFS effectively. Understanding individual sleep patterns can pave the way toward interventions aimed at improving overall well-being.
Pain Symptoms: Headaches, Muscle, and Joint Pain
Chronic Fatigue Syndrome (ME/CFS) often brings a variety of pain symptoms that can significantly impact daily life. Many individuals report persistent headaches, which may vary in intensity and frequency. These headaches can be debilitating, further complicating the challenges faced by those with ME/CFS.
Muscle pain is another common complaint. People frequently experience widespread muscle aches that resemble fibromyalgia symptoms. This discomfort can make even simple tasks feel overwhelming.
Joint pain also plays a role in the symptomatology of CFS/ME. Affected joints might swell or feel stiff, leading to increased difficulty with movement and mobility.
Understanding these pain symptoms is crucial for effective management. Each individual may experience them differently, contributing to the complexity of this condition and highlighting the need for personalized treatment approaches.
Immune System Dysfunction in CFS/ME
Immune system dysfunction is a prominent feature of Chronic Fatigue Syndrome (ME/CFS). Many patients report an array of immune-related symptoms that can complicate their condition.
Research indicates that individuals with ME/CFS often have abnormalities in immune cell function. This may include altered levels of cytokines, which are proteins essential for cellular communication during immune responses.
Additionally, some studies show evidence of chronic inflammation in these patients. This persistent inflammatory response can contribute to the fatigue and other debilitating symptoms experienced.
Moreover, infections or viral triggers are frequently noted among those diagnosed with CFS/ME. These factors might further disrupt normal immune functioning, leading to heightened vulnerability and prolonged recovery times after illness.
Understanding the intricacies of immune system involvement is crucial for developing effective treatments and improving patient outcomes.
Autonomic Nervous System Abnormalities
Chronic Fatigue Syndrome (ME/CFS) often involves abnormalities in the autonomic nervous system (ANS). The ANS regulates involuntary bodily functions, including heart rate, blood pressure, and digestion.
Patients frequently report symptoms like lightheadedness and rapid heartbeat upon standing—known as orthostatic intolerance. This occurs because the body struggles to maintain proper blood flow when shifting positions.
Additionally, some individuals with ME/CFS experience dysregulation of temperature control. They may feel excessively cold or hot without any apparent reason.
These autonomic dysfunctions can contribute to feelings of fatigue and exacerbate other symptoms. Understanding these issues is crucial for developing effective management strategies for those affected by this complex condition.
Diagnostic Criteria and Challenges
Diagnosing Chronic Fatigue Syndrome (ME/CFS) poses significant challenges. There is no definitive laboratory test for this condition, making it reliant on clinical judgment and patient history.
Healthcare providers often use specific diagnostic criteria, such as the Fukuda criteria or the Institute of Medicine’s recommendations. These frameworks emphasize prolonged fatigue lasting six months or more, paired with other debilitating symptoms.
However, many patients experience delays in diagnosis due to overlapping symptoms with conditions like fibromyalgia or depression. This can lead to misdiagnosis and inadequate treatment options.
Moreover, awareness among healthcare professionals varies widely. Some may lack familiarity with ME/CFS altogether, further complicating accurate assessments.
Patients frequently report feelings of frustration during their journey towards receiving a proper diagnosis. The complexity of symptoms adds another layer of difficulty in distinguishing ME/CFS from other illnesses that share similar features.
Differential Diagnosis: Ruling Out Other Conditions
Differential diagnosis is a critical step in identifying Chronic Fatigue Syndrome (ME/CFS). Many conditions can mimic its symptoms, making accurate diagnosis challenging. Healthcare providers must consider various disorders when evaluating a patient.
Conditions like fibromyalgia, multiple sclerosis, and depression often present with similar fatigue and pain. Blood tests may reveal thyroid dysfunction or vitamin deficiencies that could explain the symptoms as well.
Infections such as Lyme disease or Epstein-Barr virus also need to be ruled out. Each of these conditions has distinct treatment approaches that differ significantly from ME/CFS management.
A thorough medical history and symptom review are essential for clinicians. They often look for specific features—like post-exertional malaise—that distinguish ME/CFS from other illnesses.
This careful process helps ensure patients receive appropriate care tailored to their unique needs, preventing misdiagnosis and unnecessary treatments.
Treatment Approaches: Managing Symptoms
Managing symptoms of Chronic Fatigue Syndrome (ME/CFS) often requires a comprehensive and individualized approach. There is no one-size-fits-all treatment, as each person’s experience with ME/CFS varies significantly.
A combination of lifestyle adjustments, therapies, and medications may be beneficial. Many patients find relief through pacing techniques that help balance activity with rest. This method encourages individuals to engage in manageable physical exertion without triggering symptom flare-ups.
Cognitive Behavioral Therapy (CBT) can also play a role in symptom management. It helps patients develop coping strategies for dealing with the emotional impact of living with chronic fatigue.
Pharmacological interventions are another option. Certain medications might alleviate specific symptoms like pain or sleep disturbances, but their effectiveness can vary widely among individuals.
Working closely with healthcare providers allows for tailored strategies that address personal needs while aiming to improve overall quality of life.
Pacing and Energy Conservation Techniques
Pacing and energy conservation are crucial for individuals managing Chronic Fatigue Syndrome (ME/CFS). These techniques aim to balance activity and rest, preventing the exacerbation of symptoms.
Setting realistic goals is a key aspect of pacing. Individuals can break tasks into smaller, manageable steps. This approach minimizes the risk of overexertion while promoting a sense of accomplishment.
Monitoring daily activities helps in understanding personal limits. Keeping an energy diary can reveal patterns between activity levels and fatigue flare-ups.
Scheduled breaks throughout the day serve as valuable recovery periods. Short rests allow for replenishing energy reserves without triggering post-exertional malaise.
Incorporating relaxation methods like deep breathing or meditation may enhance recovery during these intervals. Adopting simple lifestyle adjustments fosters a more sustainable routine while living with ME/CFS.
Cognitive Behavioral Therapy for CFS/ME
Cognitive Behavioral Therapy (CBT) has emerged as a valuable tool in managing Chronic Fatigue Syndrome (ME/CFS). This psychotherapy approach focuses on identifying and changing negative thought patterns that may contribute to the fatigue cycle.
Through CBT, patients learn coping strategies to handle their symptoms more effectively. It encourages individuals to challenge unrealistic beliefs about their illness, which can often exacerbate feelings of helplessness.
Therapists work with patients to develop personalized action plans. These plans help in setting achievable goals for daily activities while promoting gradual exposure to previously avoided tasks.
Research indicates that CBT can lead to significant improvements in overall functioning and quality of life for those living with CFS/ME. While it may not address all physical aspects of the condition, many find emotional relief and better management strategies through this therapeutic approach.
Pharmacological Interventions and Their Efficacy
Pharmacological interventions for Chronic Fatigue Syndrome (ME/CFS) aim to alleviate symptoms rather than cure the condition. Many patients explore options like pain relievers, antidepressants, and sleep aids. These medications can sometimes provide relief from specific symptoms.
Antidepressants, particularly low-dose tricyclics, may improve sleep quality and reduce pain sensitivity. However, their effects vary among individuals.
Stimulants are another option but come with potential side effects and dependency risks. Some find them helpful during severe fatigue episodes.
Corticosteroids are occasionally prescribed for inflammation-related issues but should be used cautiously due to long-term side effects.
It’s crucial for patients to work closely with healthcare providers when considering these treatments. Tailoring medication plans based on individual responses is essential since what works well for one person might not benefit another at all.
Nutritional Considerations and Dietary Approaches
Nutritional considerations play a crucial role in managing Chronic Fatigue Syndrome (ME/CFS). Many individuals with ME/CFS report improvements when adhering to specific dietary guidelines. A balanced diet rich in whole foods can help support energy levels and overall health.
Incorporating anti-inflammatory foods, such as leafy greens, berries, and fatty fish, may alleviate some symptoms. These ingredients can help reduce inflammation linked to the condition. Additionally, maintaining proper hydration is essential for optimal bodily function.
Some patients find that eliminating processed sugars and refined carbohydrates helps stabilize energy fluctuations throughout the day. Tracking food intake can also identify potential allergens or sensitivities contributing to fatigue.
Moreover, certain supplements like magnesium and vitamin D might provide added benefits. However, it’s crucial for individuals to consult healthcare professionals before making significant dietary changes or starting new supplements tailored to their unique needs.
Exercise Controversies and Graded Exercise Therapy
Exercise controversies surrounding Chronic Fatigue Syndrome (ME/CFS) have garnered significant attention in recent years. The debate largely centers on the role of physical activity in managing symptoms.
Graded Exercise Therapy (GET) has been a recommended approach for some patients, promoting gradual increases in exercise intensity. Proponents argue it can help improve function and reduce fatigue over time.
However, many individuals with ME/CFS report worsening symptoms after even minimal exertion. This phenomenon highlights the risk of post-exertional malaise (PEM), where patients experience debilitating fatigue following physical or mental activity.
Critics of GET emphasize that it may not be suitable for everyone with CFS/ME and could potentially do more harm than good. As research continues to evolve, understanding individual responses to exercise remains crucial for effective management strategies tailored to each patient’s unique needs.
Impact on Quality of Life and Disability
Chronic Fatigue Syndrome (ME/CFS) can drastically alter a person’s quality of life. The persistent fatigue and associated symptoms often hinder daily activities, making even simple tasks feel monumental.
Individuals may find it challenging to maintain employment or engage in social interactions. This isolation can lead to feelings of frustration and hopelessness.
Disability is common among those with ME/CFS, as many rely on assistance for their day-to-day needs. The unpredictability of the condition adds another layer of complexity; good days can quickly turn into debilitating ones without warning.
The emotional toll cannot be overlooked either. Anxiety and depression frequently accompany this syndrome, compounding its impact on mental well-being. Adapting to such changes requires immense resilience from patients and their families alike.
Support systems play a crucial role in navigating these challenges, offering understanding amid the struggles that come with Chronic Fatigue Syndrome (ME/CFS).
Current Research and Emerging Treatments
Current research on Chronic Fatigue Syndrome (ME/CFS) is gaining momentum, shedding light on this complex condition. Scientists are exploring various avenues to understand its underlying mechanisms better. Advances in immunology and neurology are particularly promising.
Recent studies have focused on the immune system’s role in ME/CFS, suggesting that inflammation may be a contributing factor to symptoms. This has led researchers to investigate potential treatments targeting immune dysfunction.
Another area of interest is the autonomic nervous system, which regulates many bodily functions without conscious control. Some studies indicate abnormalities in this system could explain some of the debilitating symptoms experienced by those with ME/CFS.
Emerging therapies aim at symptom management rather than a cure due to the multifaceted nature of the disorder. Clinical trials are assessing new drug therapies that might help alleviate pain or improve energy levels.
Moreover, there’s an increasing focus on personalized medicine approaches tailored to individual patient profiles based on their specific symptoms and responses to treatment.
As awareness grows within both medical communities and society at large, there’s hope for more comprehensive understanding and support for individuals living with Chronic Fatigue Syndrome (ME/CFS). With continued research efforts, we move closer to finding effective strategies for managing this challenging condition.