Birt–Hogg–Dubé Syndrome (BHD) is a rare genetic disorder that often flies under the radar, yet it can have significant implications for those affected. Characterized by unique skin manifestations, pulmonary cysts, and an increased risk of kidney tumors, this syndrome presents various challenges for patients. Understanding BHD is crucial not only for managing its symptoms but also for navigating the potential health risks associated with it.
For individuals and families dealing with Birt–Hogg–Dubé Syndrome, awareness plays a pivotal role in early detection and effective treatment. This blog delves into the intricacies of BHD—its genetic basis, clinical features, management strategies—and offers insights into living well with this condition. Whether you’re seeking information to help yourself or someone you love, you’re in the right place to learn more about this complex syndrome.
Overview of Birt–Hogg–Dubé Syndrome: A Rare Genetic Disorder
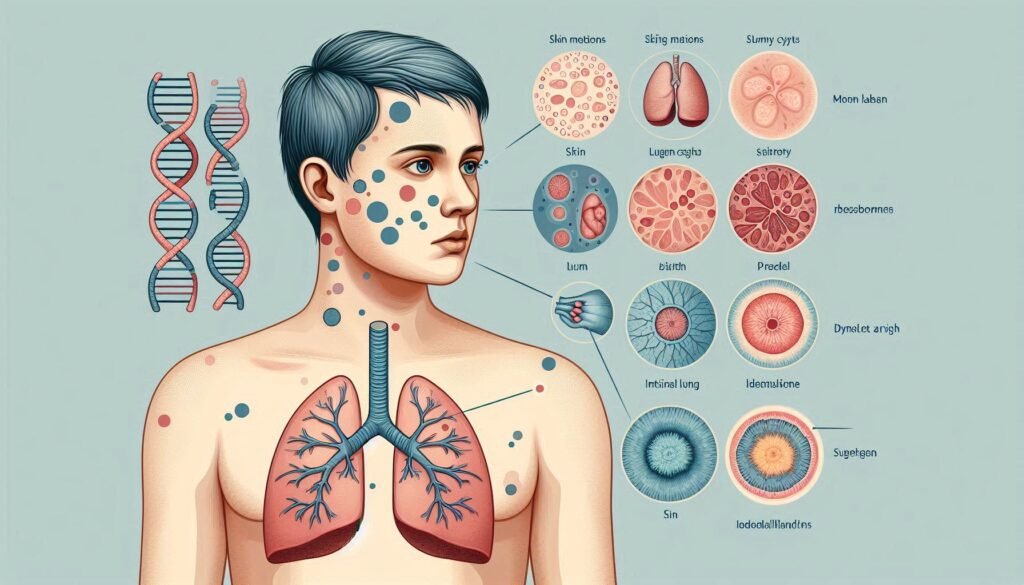
Birt–Hogg–Dubé Syndrome is a genetic disorder that affects multiple systems in the body, primarily manifesting through skin lesions, lung cysts, and renal tumors. It was first described in 1977 by researchers Birt, Hogg, and Dubé.
Individuals with BHD often exhibit distinctive fibrofolliculomas—small benign growths on the skin. These can be found predominantly on the face and neck but may also appear elsewhere.
“What Are The Early Signs of AIDS? Understanding HIV Progression”
The pulmonary aspect of this syndrome includes characteristic lung cysts that can lead to complications such as pneumothorax—a condition where air leaks into the space between the lung and chest wall.
Renal tumors associated with BHD are usually of a specific type known as hybrid oncocytic tumors or chromophobe carcinoma. Awareness of these features is critical for early diagnosis and management options tailored to individual needs.
Genetic Basis: Mutations in the FLCN Gene
Birt–Hogg–Dubé Syndrome has a distinct genetic foundation. It primarily arises from mutations in the FLCN gene, located on chromosome 17. This gene encodes for folliculin, a protein that plays a crucial role in cellular processes.
These mutations disrupt normal functioning of folliculin, leading to abnormal cell growth and development. As a result, individuals may experience various manifestations associated with this syndrome.
FLCN mutations can be inherited or occur sporadically. When passed down through families, these changes follow an autosomal dominant pattern. This means that only one copy of the mutated gene is necessary for an individual to express the syndrome’s features.
“How Does Babinski-Nageotte Syndrome Affect The Brainstem?”
Understanding this genetic basis is vital for accurate diagnosis and management of BHD syndrome. Genetic testing can confirm the presence of FLCN mutations, allowing families to make informed decisions about their health and future planning.
Inheritance Pattern and Family Screening in BHD Syndrome
Birt–Hogg–Dubé Syndrome (BHD) follows an autosomal dominant inheritance pattern. This means that only one copy of the mutated FLCN gene is necessary for an individual to develop the syndrome. If one parent carries the mutation, each child has a 50% chance of inheriting it.
Family screening plays a crucial role in managing BHD. Early identification can lead to timely interventions and monitoring for associated complications like renal tumors and pulmonary cysts. Genetic counseling should be considered for affected families, as it helps them understand risks and implications.
“What Causes Baller-Gerold Syndrome? Guide to Rare Cranial Disorder”
Testing unaffected relatives may also provide insight into their risk status, guiding preventive measures. Engaging with healthcare professionals specializing in genetic disorders ensures comprehensive care tailored to each family’s needs, fostering informed decision-making regarding health management strategies related to BHD syndrome.
Cutaneous Manifestations: Fibrofolliculomas and Skin Tags
Cutaneous manifestations are a hallmark of Birt–Hogg–Dubé Syndrome. Patients often develop fibrofolliculomas, small benign tumors that appear as flesh-colored or slightly elevated bumps on the skin. These growths typically emerge in areas rich in hair follicles, such as the face, neck, and trunk.
Skin tags are another common feature among individuals with this syndrome. These soft tissue protrusions can occur anywhere on the body but are frequently found around the neck and underarms. While generally harmless, they may cause cosmetic concerns for some patients.
“Why Does Bardet-Biedl Syndrome Cause Multiple Health Issues?”
The presence of these lesions serves as an important clinical marker for diagnosing BHD syndrome. Dermatological evaluations play a crucial role in identifying and managing these skin manifestations effectively. Regular monitoring is recommended to address any changes in appearance or texture over time.
Pulmonary Involvement: Cysts and Pneumothorax Risk
Pulmonary involvement in Birt–Hogg–Dubé Syndrome is significant and presents a unique set of challenges. Patients often develop multiple pulmonary cysts, which are fluid-filled sacs in the lungs. These cysts can vary in size and number, making monitoring essential.
The presence of these cysts increases the risk of pneumothorax, a condition where air leaks into the space between the lung and chest wall. This can lead to serious respiratory issues requiring immediate medical attention. Symptoms may include sudden chest pain or difficulty breathing.
“How Does Bartter Syndrome Affect Kidney Function? Expert Guide”
Routine imaging studies like chest CT scans play a crucial role in identifying these complications early on. Awareness of this risk allows for timely interventions that can alleviate potential health threats associated with pulmonary manifestations of BHD syndrome. Regular follow-ups with healthcare providers ensure that patients remain vigilant about their lung health throughout their lives.
Renal Tumors in Birt–Hogg–Dubé Syndrome
Renal tumors are a significant concern in individuals with Birt–Hogg–Dubé Syndrome (BHD). These tumors often present as renal cell carcinoma, which can develop at an earlier age than seen in the general population.
Patients with BHD have an increased risk for developing multiple types of renal neoplasms. Chromophobe and oncocytoma variants are particularly common among these patients. Regular surveillance through imaging is critical to catch any potential growth early.
“What Triggers Behcet’s Syndrome & How Can It Be Managed?”
The relationship between FLCN gene mutations and tumor development highlights the importance of genetic testing. Understanding this connection aids healthcare providers in crafting personalized management plans tailored to individual risks.
Surgical intervention may be necessary if tumors become large or symptomatic. Nephron-sparing techniques are preferred when possible, due to their ability to preserve kidney function while effectively treating cancerous lesions.
Other Associated Neoplasms in BHD Syndrome
Birt–Hogg–Dubé Syndrome (BHD) is primarily known for its cutaneous and renal manifestations. However, other associated neoplasms can also emerge in individuals with this genetic condition.
Patients may develop fibrofolliculomas, which are benign tumors of hair follicles. These often present as small skin-colored or slightly pigmented bumps, typically found on the face, neck, and upper body.
In addition to fibrofolliculomas, some studies indicate a potential risk for malignant neoplasms. Thyroid cancer has been reported among BHD patients at a higher rate than the general population.
“Why Does Bloom Syndrome Increase Cancer Risk? Complete Guide”
Moreover, there have been instances of colon polyps and gastrointestinal malignancies in affected families. The relationship between these conditions and BHD remains an area of ongoing research. Awareness of these possible associations is crucial for comprehensive patient care and monitoring strategies.
Clinical Diagnostic Criteria for BHD Syndrome
Diagnosing Birt–Hogg–Dubé Syndrome (BHD) involves a combination of clinical evaluation and specific criteria. Dermatological manifestations play a crucial role in the identification process. Patients typically present with fibrofolliculomas, which are small, dome-shaped lesions on the face, neck, and upper trunk.
In addition to skin findings, pulmonary cysts are often discovered incidentally during imaging studies. These cysts may lead to pneumothorax, adding another layer of complexity to diagnosis.
Family history is also significant. A known relative with BHD can strengthen the case for suspicion. Genetic testing for mutations in the FLCN gene provides definitive confirmation but is not always necessary when clinical signs are prominent.
Healthcare professionals utilize these criteria collectively to establish an accurate diagnosis of BHD syndrome and guide further management strategies effectively.
Genetic Testing and Counseling for BHD Families
Genetic testing plays a crucial role for families affected by Birt–Hogg–Dubé Syndrome. Identifying mutations in the FLCN gene helps confirm a diagnosis and assess risks for family members.
Counseling provides essential support, guiding families through complex emotional and medical landscapes. Understanding the hereditary nature of BHD allows relatives to make informed decisions regarding their health.
Families can benefit from discussions about screening options and preventive measures tailored to individual risk profiles. This proactive approach aids not only in early detection but also in managing associated complications effectively.
Moreover, genetic counseling fosters open communication within families about potential implications for future generations. It empowers individuals with knowledge, offering them resources to navigate living with or without the condition confidently.
Dermatological Evaluation and Management
Dermatological evaluation is crucial for individuals with Birt–Hogg–Dubé Syndrome. The skin manifestations, primarily fibrofolliculomas and skin tags, can significantly impact quality of life. Regular dermatological assessments help in monitoring these lesions.
During evaluations, dermatologists may use dermoscopy to identify specific features associated with BHD. This technique enhances the visualization of hair follicle-related growths and aids in accurate diagnosis.
Management often includes regular removal of bothersome or symptomatic fibrofolliculomas. Several methods such as excision, laser therapy, or electro-dessication are available depending on individual cases.
Additionally, patient education plays a key role in self-monitoring skin changes over time. Awareness helps individuals seek timely medical advice when new lesions appear or if existing ones change characteristically.
Maintaining a collaborative approach with healthcare providers ensures comprehensive care tailored to the needs of those affected by this genetic disorder.
Pulmonary Function Tests and Imaging in BHD
Pulmonary function tests (PFTs) are essential for assessing lung health in patients with Birt–Hogg–Dubé Syndrome. These tests measure how well the lungs work, helping to identify any functional impairments caused by pulmonary cysts.
Imaging studies play a crucial role in monitoring lung conditions associated with BHD. High-resolution computed tomography (HRCT) scans provide detailed images of the lungs, revealing cystic changes and any signs of pneumothorax. Regular imaging is vital for early detection and management of potential complications.
Patients often experience spontaneous pneumothorax due to weakened lung tissue surrounding the cysts. Close monitoring through PFTs and imaging helps guide treatment decisions, ensuring timely interventions when necessary.
These diagnostic tools contribute significantly to understanding an individual’s pulmonary health within the context of Birt–Hogg–Dubé Syndrome, promoting better patient outcomes over time.
Renal Imaging and Surveillance Protocols
Regular renal imaging is vital for patients with Birt–Hogg–Dubé Syndrome. This genetic condition predisposes individuals to renal tumors, making surveillance critical.
Ultrasound is often the first-line imaging tool. It’s non-invasive and helps identify cysts or masses in the kidneys. MRI offers a more detailed view and can distinguish between benign and malignant lesions.
CT scans are also valuable but involve radiation exposure, so they should be used judiciously. Regular screenings typically begin in adolescence or early adulthood, as early detection improves outcomes significantly.
The frequency of surveillance usually depends on individual risk factors, such as family history or prior tumor development. Collaboration with a healthcare team ensures personalized protocols that adapt over time based on emerging evidence and patient needs.
Staying informed about advancements in imaging technologies can enhance monitoring strategies for those affected by this syndrome.
Management of Spontaneous Pneumothorax in BHD Patients
Spontaneous pneumothorax is a significant concern for individuals with Birt–Hogg–Dubé Syndrome. This condition arises due to the formation of cysts in the lungs, which can rupture and lead to air leakage into the pleural space.
Management typically begins with monitoring symptoms. If chest pain or shortness of breath occurs, immediate medical assessment is essential. Healthcare providers may recommend imaging studies like a chest X-ray or CT scan to evaluate the severity.
In cases where pneumothorax is large or symptomatic, treatment options include needle decompression followed by chest tube placement. This intervention helps remove excess air and allows re-expansion of the lung.
Patients should be educated about recognizing warning signs early on. Regular follow-ups are crucial for ongoing surveillance and management strategies tailored to their unique situation. Each case requires individualized care based on specific patient needs and clinical presentation.
Surgical Approaches to Renal Tumors in BHD Syndrome
Surgical intervention is often necessary for managing renal tumors associated with Birt–Hogg–Dubé Syndrome. The choice of surgery typically depends on tumor size, location, and the patient’s overall health.
Laparoscopic nephrectomy has become a popular approach due to its minimally invasive nature. This technique allows for reduced recovery time and less postoperative pain compared to traditional open surgeries.
In cases where tumors are localized, partial nephrectomy may be performed. This procedure preserves healthy kidney tissue while effectively removing cancerous cells.
Surgeons must assess each case individually, as multiple tumors can complicate treatment plans. Close collaboration between urologists and oncologists ensures optimal outcomes for patients facing these challenges.
Preoperative imaging plays a crucial role in planning the surgical approach by providing detailed insights into tumor characteristics and surrounding structures.
Differential Diagnosis: Conditions Similar to BHD
Birt–Hogg–Dubé Syndrome (BHD) presents unique clinical features, but several other conditions can mimic its symptoms. Accurate diagnosis is essential for effective management.
One similar disorder is tuberous sclerosis complex (TSC). It involves skin lesions and renal tumors, often creating confusion with BHD. However, TSC typically also affects neurological function.
Another condition to consider is familial multiple lipomatosis. Patients may develop skin tags and fibrous growths, resembling fibrofolliculomas found in BHD but without the pulmonary or renal implications.
Gardner syndrome also shares overlapping traits such as cutaneous manifestations and a predisposition to cancer. Unlike BHD, it predominantly leads to colorectal polyps and osteomas.
Genetic testing plays a crucial role in differentiating these syndromes. Comprehensive evaluations help clarify diagnoses by analyzing family histories and phenotypic presentations effectively.
Psychological Impact of BHD Diagnosis and Management
Receiving a diagnosis of Birt–Hogg–Dubé Syndrome can be overwhelming. Patients often experience anxiety and uncertainty about their health. The potential for developing renal tumors or pulmonary complications adds to this emotional burden.
Individuals may grapple with concerns over their genetic legacy, especially if family members are affected. This feeling can lead to guilt or fear regarding future generations.
Moreover, the visible skin manifestations of BHD can impact self-esteem and body image. Many patients report social withdrawal due to embarrassment over fibrofolliculomas and skin tags.
Support groups play a crucial role in addressing these psychological challenges. Connecting with others who share similar experiences helps reduce feelings of isolation. Mental health professionals also provide valuable coping strategies tailored to managing life with BHD syndrome.
Lifestyle Modifications and Preventive Measures
Managing Birt–Hogg–Dubé Syndrome involves several lifestyle modifications that can enhance quality of life. Regular dermatological check-ups are essential for monitoring skin lesions and managing fibrofolliculomas effectively.
Incorporating a healthy diet rich in antioxidants may help support overall health. Focusing on fruits, vegetables, and whole grains can contribute to better immune function.
Staying active is also crucial. Engaging in regular exercise boosts lung function and reduces the risk of complications associated with pulmonary cysts.
Avoiding tobacco use is vital as it increases the risk of respiratory issues and lung cancer, particularly for those already predisposed due to their genetic condition.
Stress management techniques like yoga or meditation can enhance mental well-being. These practices promote relaxation and resilience against anxiety related to health concerns.
Staying informed about Birt–Hogg–Dubé Syndrome fosters proactive engagement with healthcare providers for tailored preventive strategies.
Pregnancy Considerations in BHD Syndrome
Pregnancy in women with Birt–Hogg–Dubé Syndrome warrants careful consideration. The presence of renal tumors or pulmonary cysts may complicate pregnancy, necessitating a multidisciplinary approach to care.
Expectant mothers should undergo thorough evaluations before conception. Regular imaging can help monitor the status of any renal masses and assess lung health, reducing potential risks during pregnancy.
Hormonal changes can influence tumor behavior. Consulting with specialists is vital for personalized management plans throughout gestation.
Labor and delivery also require planning due to possible pulmonary complications, such as spontaneous pneumothorax. An experienced medical team should be on standby to address emergencies if they arise.
Postpartum follow-up is essential for monitoring both maternal health and any impact on existing conditions caused by the stress of childbirth. Awareness and proactive measures can foster healthier outcomes for both mother and child in this unique clinical context.
Long-term Prognosis and Follow-up Care
The long-term prognosis for individuals with Birt–Hogg–Dubé Syndrome varies significantly. Early detection and regular monitoring greatly influence outcomes. Patients often require lifelong surveillance due to the risk of renal tumors.
Follow-up care is crucial and typically includes annual imaging studies, such as ultrasound or MRI, to monitor kidney health. This proactive approach helps in identifying any changes early on.
Patients should also engage in routine dermatological check-ups to manage skin lesions effectively. Treatment options may include surgical removal of troublesome fibrofolliculomas or skin tags.
Regular pulmonary assessments are essential as well, given the potential for cysts and pneumothorax development. Maintaining an open line of communication with healthcare providers ensures timely interventions when necessary.
Support from multidisciplinary teams can provide comprehensive care tailored to individual needs, improving quality of life over time. Regular genetic counseling sessions can also help families navigate the implications of this syndrome responsibly.
Current Research and Emerging Therapies for BHD Syndrome
Current research on Birt–Hogg–Dubé Syndrome is expanding our understanding of this rare genetic disorder and paving the way for potential therapies. Scientists are investigating the role of the FLCN gene in cellular pathways to determine how mutations lead to disease manifestations. This exploration could unlock targeted treatments that address not just symptoms but also underlying causes.
Emerging therapies focus on managing renal tumors and mitigating complications like pneumothorax. Researchers are evaluating inhibitors that may affect tumor growth or enhance immune response against neoplasms associated with BHD syndrome. Additionally, clinical trials are underway for gene therapy approaches aimed at correcting or compensating for FLCN mutations.
Patient registries and collaborative studies are enabling a deeper look into long-term outcomes, enhancing surveillance strategies, and improving management protocols across healthcare settings. As knowledge about BHD syndrome evolves, so too does hope for those affected by it. Continuous advancements in genetics hold promise for developing effective interventions that can ultimately improve quality of life.
As researchers uncover new findings, it’s crucial for patients and families to stay informed about available options and participate actively in discussions with their healthcare providers regarding emerging treatments tailored to individual needs within the framework of Birt–Hogg–Dubé Syndrome management.


