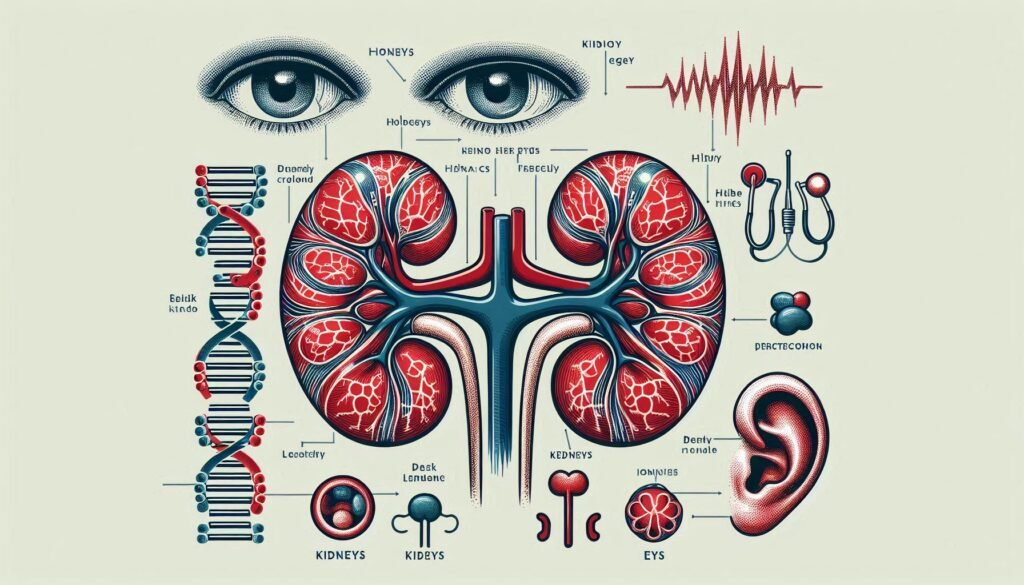
Alport Syndrome is a rare genetic disorder that significantly impacts the lives of those affected by it. Characterized by progressive kidney disease, hearing loss and ocular abnormalities, this condition poses unique challenges for patients and their families. Understanding Alport Syndrome is crucial not only for diagnosis but also for effective management strategies tailored to individual needs.
As awareness grows around this complex disorder, so does the importance of early intervention and support systems that can enhance quality of life. Let’s delve into the intricacies of Alport Syndrome—from its genetic underpinnings to innovative therapies on the horizon—providing you with essential insights into this multifaceted condition.
Alport Syndrome: An Overview of the Genetic Disorder
Alport Syndrome is a hereditary condition primarily affecting the kidneys, ears, and eyes. It results from mutations in genes responsible for producing collagen, specifically type IV collagen. This protein plays a critical role in maintaining the structure of various tissues.
The disorder manifests differently depending on its genetic variant, which can be X-linked or inherited through autosomal recessive and dominant patterns. The X-linked form is the most common and typically affects males more severely than females.
“What Causes Brugada Syndrome & Why Is It Dangerous?”
Patients often experience symptoms that lead to progressive kidney disease, hearing impairment, and visual disturbances over time. Early identification is vital for managing complications effectively. Awareness about Alport Syndrome enables better support systems and tailored treatment options for those affected by this complex genetic disorder.
Genetic Basis: X-linked, Autosomal Recessive, and Autosomal Dominant Forms
Alport Syndrome arises from mutations in genes responsible for producing collagen. This essential protein forms the structure of various tissues, including those in the kidneys, ears, and eyes.
The most common form is X-linked Alport Syndrome. It primarily affects males due to its inheritance pattern linked to the X chromosome. Females can be carriers and exhibit milder symptoms.
“Why Does Burning Mouth Syndrome Occur? Treatment Guide”
There are also autosomal recessive and autosomal dominant forms of Alport Syndrome. In autosomal recessive cases, both parents must pass down a mutated gene for a child to be affected. This type often leads to more severe manifestations.
Autosomal dominant Alport Syndrome is rarer but significant. Here, only one parent needs to pass on the mutation for an offspring to inherit the disorder. Each genetic variant plays a critical role in determining disease severity and progression across affected individuals.
Pathophysiology of Alport Syndrome
Alport Syndrome primarily affects the glomerular basement membrane, a critical structure in kidney function. The disorder is linked to mutations in genes that encode type IV collagen, which is essential for maintaining the integrity of this membrane.
“What Is Bálint’s Syndrome? Understanding Visual Processing Issues”
These genetic alterations disrupt normal collagen production. This disruption leads to structural abnormalities in kidney tissues, resulting in progressive damage. As the disease advances, affected individuals often experience glomerulosclerosis and interstitial fibrosis.
The pathophysiological changes extend beyond renal implications. Abnormalities also impact ocular structures and cochlear cells due to shared collagen pathways. This results in characteristic visual impairments and hearing loss associated with Alport Syndrome.
Understanding these mechanisms provides valuable insight into potential therapeutic approaches aimed at mitigating organ damage and improving patient outcomes across various manifestations of the disorder.
Epidemiology and Prevalence of Alport Syndrome
Alport Syndrome is a rare genetic disorder affecting the kidneys, ears, and eyes. Its prevalence varies across different populations. Estimates suggest that it occurs in approximately 1 in 5,000 to 10,000 individuals worldwide.
The X-linked form is the most common and predominantly affects males. Females can also be carriers but often experience milder symptoms due to their second normal X chromosome.
“How Does CADASIL Syndrome Affect Brain Blood Vessels?”
Autosomal recessive and dominant forms exist as well but are less frequently diagnosed. These variations contribute to differences in symptom severity and age of onset among patients.
Epidemiological studies indicate that Alport Syndrome may go underdiagnosed or misdiagnosed due to its overlapping features with other renal disorders. Enhanced awareness among healthcare providers can lead to improved identification rates within affected communities.
Clinical Manifestations: Kidney Involvement
Alport Syndrome primarily affects the kidneys, leading to a range of clinical manifestations. Patients often experience hematuria, which is blood in the urine. This symptom can be intermittent and may vary in severity.
Proteinuria is another common feature, indicating that protein leaks into the urine due to kidney damage. Over time, this can progress to nephrotic syndrome, characterized by significant protein loss and swelling.
“What Causes Cat Eye Syndrome? Chromosome 22 Guide”
As the disease advances, chronic kidney disease (CKD) may develop. Patients might show elevated creatinine levels and reduced glomerular filtration rate (GFR).
Monitoring renal function regularly is crucial for timely interventions. Early identification of worsening kidney involvement allows healthcare providers to implement management strategies effectively. Each patient’s journey with Alport Syndrome can differ significantly based on their genetic background and other factors influencing kidney health.
Ocular Abnormalities in Alport Syndrome
Ocular abnormalities are a notable aspect of Alport Syndrome. Patients often experience various eye-related issues linked to the underlying genetic disorder.
One common manifestation is anterior lenticonus, characterized by a cone-shaped distortion of the lens. This condition can lead to visual impairment if not addressed promptly.
“How Does Charcot-Marie-Tooth Disease Affect Nerves?”
Retinal changes may also occur, including flecks or deposits that affect vision quality. These retinal alterations can be subtle and require careful monitoring by an ophthalmologist.
Keratoconus is another concern for individuals with Alport Syndrome. It involves thinning and bulging of the cornea, leading to distorted vision and increased sensitivity to light.
Regular eye examinations are crucial for early detection and management of these ocular manifestations. By addressing these issues proactively, healthcare providers can help enhance the quality of life for those affected by this genetic kidney disease.
Hearing Loss: A Common Feature of Alport Syndrome
Hearing loss is a prominent feature of Alport Syndrome, affecting approximately 50% to 90% of individuals with the disorder. This auditory impairment typically manifests in late childhood or early adolescence.
The hearing loss associated with Alport Syndrome is often progressive and can vary in severity. It primarily involves high-frequency sounds, making it challenging for patients to hear conversations or sounds like birds chirping.
“Why Does Chronic Fatigue Syndrome Cause Persistent Tiredness?”
This condition arises from mutations in genes that are crucial for the formation of collagen type IV, which plays a vital role in the structure of the inner ear. As a result, damage occurs within the cochlea, leading to sensorineural hearing loss.
Early detection and intervention are essential to manage this aspect effectively. Hearing aids or cochlear implants may significantly improve communication abilities and overall quality of life for those affected by this genetic disorder.
Dermatological Manifestations in Alport Patients
Dermatological manifestations in Alport syndrome can vary among patients. While the primary focus of this genetic disorder is on kidney function, skin symptoms may also present.
Some individuals experience changes in nail structure. These alterations can include thickening or ridging, which might be noticeable over time.
Additionally, there are reports of skin lesions resembling eczema. Such conditions could lead to discomfort and require appropriate management to alleviate symptoms.
Another notable aspect is the potential for scarring alopecia, a rare manifestation where hair loss occurs due to inflammation affecting hair follicles. This condition requires careful dermatological evaluation and treatment.
Awareness of these skin-related concerns is essential for comprehensive care in Alport syndrome patients. Regular check-ups with dermatologists help address any emerging issues early on while ensuring optimal patient support throughout their journey with this condition.
Cardiovascular Complications Associated with Alport Syndrome
Cardiovascular complications are an important aspect of Alport Syndrome that often receive less attention than kidney and hearing issues. Research indicates a higher prevalence of hypertension among patients with this genetic disorder.
Elevated blood pressure can result from the kidney’s impaired function, leading to excess fluid retention. This condition increases the workload on the heart. Over time, it may contribute to left ventricular hypertrophy and other cardiac problems.
Additionally, some studies suggest a correlation between Alport Syndrome and structural heart abnormalities. These include conditions such as mitral valve prolapse or arrhythmias.
Regular cardiovascular assessments should be part of patient management plans. Monitoring blood pressure is crucial for early intervention. Lifestyle modifications, along with pharmacological treatments when needed, can help mitigate these risks effectively.
Diagnostic Approaches: Clinical, Genetic, and Histological
Diagnosing Alport Syndrome involves a multifaceted approach. Clinicians first assess the patient’s medical history and family background. A thorough physical examination can reveal signs like hematuria or proteinuria.
Genetic testing plays a crucial role in confirming the diagnosis. Identifying mutations in genes such as COL4A3, COL4A4, or COL4A5 helps distinguish between different forms of the disorder. These tests provide insights into inheritance patterns and guide treatment options.
Histological analysis is another vital diagnostic tool. A kidney biopsy may show characteristic changes in glomerular structure under a microscope, such as irregularities in the basement membrane. This can support clinical findings and genetic test results.
Combining these diagnostic methods allows for accurate identification of Alport Syndrome while also ruling out other conditions that present similarly. Each step is essential to tailor an effective management plan for affected individuals.
Genetic Testing and Counseling for Alport Syndrome
Genetic testing is a critical tool for diagnosing Alport Syndrome. It helps identify specific mutations in genes associated with the disorder, primarily COL4A3, COL4A4, and COL4A5. This testing can confirm a diagnosis when clinical symptoms are present.
Counseling plays an essential role alongside genetic testing. Families affected by Alport Syndrome often have questions about inheritance patterns and risks for future generations. A healthcare provider specializing in genetics can offer insights tailored to individual family circumstances.
Understanding the genetic basis of this condition allows families to make informed decisions regarding management and potential interventions. It also aids in clarifying prognosis based on identified mutations.
Additionally, pre-conception counseling may be beneficial for at-risk couples considering starting a family. Knowledge gained through genetic counseling empowers individuals with choices that align with their values and reproductive goals.
Differential Diagnosis: Conditions Similar to Alport Syndrome
Differential diagnosis is crucial when evaluating suspected cases of Alport Syndrome. Several conditions can mimic its symptoms, leading to potential misdiagnosis.
One notable condition is Thin Basement Membrane Nephropathy (TBMN). TBMN often presents with hematuria and proteinuria but lacks the additional systemic features seen in Alport Syndrome.
Another similar disorder is Fabry Disease, a genetic condition that also causes kidney damage. However, it typically includes distinctive skin lesions and neuropathic pain not found in Alport patients.
Lupus nephritis must also be considered. This autoimmune disease can cause kidney inflammation and shares some clinical manifestations such as hematuria and proteinuria.
IgA Nephropathy may present with episodic blood in urine after infections or exercise. Distinguishing between these conditions requires careful clinical evaluation and appropriate testing for accurate diagnosis.
Management of Chronic Kidney Disease in Alport Patients
Managing chronic kidney disease (CKD) in Alport syndrome patients necessitates a tailored approach. Regular monitoring of kidney function is essential to track progression and adjust treatment plans accordingly.
Dietary modifications can play a significant role. A diet low in protein, sodium, and phosphorus may help reduce the workload on kidneys while managing blood pressure.
Pharmacological interventions include the use of ACE inhibitors. These medications not only lower blood pressure but also provide renal protection by reducing proteinuria, which is common in these patients.
Patients should receive education about recognizing early signs of complications. This empowers them to seek timely medical attention when needed.
Additionally, lifestyle changes such as quitting smoking and maintaining an active lifestyle contribute positively toward overall health management for individuals with Alport syndrome. Engaging with healthcare professionals regularly ensures that any adjustments to care are made promptly based on individual needs.
Proteinuria Control and ACE Inhibitor Therapy
Proteinuria is a significant marker of kidney damage in Alport Syndrome. Managing protein levels in urine is crucial for slowing disease progression.
ACE inhibitors are commonly prescribed to control proteinuria. They work by relaxing blood vessels, which decreases pressure within the kidneys. This action helps reduce the amount of protein that leaks into the urine.
In addition to protecting kidney function, ACE inhibitors can help manage hypertension frequently seen in these patients. Lowering blood pressure alleviates stress on renal tissues and may enhance overall outcomes.
Regular monitoring of kidney function and urinary protein levels is essential during treatment with ACE inhibitors. Adjustments in dosage or medication might be necessary based on individual response and side effects.
Patients should maintain open communication with healthcare providers about any changes they experience while on therapy to ensure optimal management strategies are implemented effectively.
Renal Replacement Therapy: Dialysis and Transplantation
Renal replacement therapy is essential for patients with end-stage kidney disease, particularly those affected by Alport Syndrome. There are two main options: dialysis and transplantation.
Dialysis serves as a life-sustaining treatment that mimics kidney function. It helps remove waste products and excess fluids from the body. Patients can choose between hemodialysis, which filters blood through a machine, or peritoneal dialysis, where the lining of the abdomen acts as a filter.
Transplantation offers another avenue for restoring renal function. A suitable donor’s kidney can significantly improve quality of life and longevity for Alport Syndrome patients. However, finding an appropriate match may take time.
Both treatments have their own risks and benefits. It’s crucial to work closely with healthcare providers to determine which option aligns best with individual health needs and lifestyle preferences. Regular follow-ups ensure optimal management throughout this journey.
Hearing Aids and Cochlear Implants for Auditory Management
For individuals with Alport Syndrome experiencing hearing loss, auditory management is crucial. Hearing aids can significantly enhance sound perception in many cases. These devices amplify sounds to help those affected communicate more effectively.
Cochlear implants represent an alternative for patients with severe to profound hearing loss. Unlike traditional hearing aids, cochlear implants bypass damaged parts of the ear and directly stimulate the auditory nerve. This technology can restore a sense of sound where conventional methods fall short.
Regular audiological assessments are necessary to tailor the best approach for each individual’s needs. A multidisciplinary team often collaborates to provide comprehensive care, ensuring that both auditory and overall health needs are met efficiently.
Ophthalmological Care in Alport Syndrome
Ophthalmological care is essential for individuals with Alport Syndrome. This genetic condition often leads to various eye abnormalities, primarily affecting the lens and retina. Regular eye examinations are crucial for early detection of these issues.
Patients may experience cataracts or keratoconus, which can significantly impact vision quality. Addressing these problems promptly can help maintain visual function.
In some cases, specialized lenses or corrective eyewear may be necessary to enhance sight. Surgery might also be recommended for more severe ocular complications.
Collaboration between nephrologists and ophthalmologists ensures comprehensive management of patient health in Alport Syndrome. By monitoring eye health closely, specialists can provide tailored interventions that improve overall quality of life for affected individuals.
Psychological Support and Quality of Life Considerations
Living with Alport Syndrome can significantly impact emotional well-being. Patients often face challenges related to chronic kidney disease, hearing loss, and ocular issues. These factors can lead to anxiety and depression.
Support systems play a crucial role in managing these psychological pressures. Family involvement is essential. Open communication helps patients express their feelings and concerns. Understanding from loved ones fosters a sense of security.
Professional assistance also proves invaluable. Psychologists or counselors specializing in chronic illness provide tailored strategies for coping with emotional distress. Group therapy offers shared experiences that reduce feelings of isolation.
Quality of life considerations extend beyond physical health. Engaging in support groups encourages resilience and hope among patients facing similar struggles. Resources are available to help navigate the complexities associated with Alport Syndrome, making it easier for individuals to advocate for their mental health needs alongside their medical care.
Emerging Therapies and Clinical Trials for Alport Syndrome
Emerging therapies and clinical trials for Alport Syndrome show promise in improving patient outcomes. Researchers are exploring various treatment modalities aimed at addressing the underlying genetic causes of this condition. Gene therapy is one area capturing attention, with the potential to rectify mutations responsible for Alport Syndrome.
Several clinical trials are investigating new pharmacological agents that may slow disease progression or enhance kidney function. These include medications targeting specific pathways involved in fibrosis and inflammation within the kidneys. Early results from these studies suggest a positive impact on proteinuria levels, which is crucial for managing chronic kidney disease associated with Alport Syndrome.
Additionally, there have been advancements in regenerative medicine approaches like stem cell therapy, aiming to restore damaged renal tissues. While still in experimental stages, these therapies offer hope for long-term recovery and improved quality of life for patients facing this challenging disorder.
Collaborative efforts among research institutions and healthcare providers are essential to advance understanding and management of Alport Syndrome. The ongoing commitment to uncovering innovative treatments will play a critical role in transforming care strategies and providing support for affected individuals and their families. As research evolves, it holds the key to unlocking better therapeutic options tailored specifically for those living with Alport Syndrome.

