Adie Syndrome is a fascinating neurological condition that often goes unnoticed by the general public. Characterized primarily by a tonic pupil and absent reflexes, this syndrome can significantly impact daily life. While it may sound complex, understanding Adie Syndrome is crucial for those who experience its symptoms or wish to support someone affected by it.
Imagine having pupils that react sluggishly to light or experiencing unusual sensations in your limbs due to absent reflexes. These are just glimpses of what individuals with Adie Syndrome might face regularly. Moreover, the connection between the autonomic nervous system and these symptoms adds another layer of intrigue to this condition.
In this blog post, we will explore various aspects of Adie Syndrome—from its history and clinical features to diagnosis and management strategies—providing you with a comprehensive understanding of this unique neurological disorder. Whether you’re searching for information out of personal interest or seeking insights for better management options, you’ve come to the right place!
Defining Adie Syndrome: An Overview of the Neurological Condition
Adie Syndrome, also known as Adie’s pupil or Holmes-Adie syndrome, is a neurological condition that affects the autonomic nervous system. It primarily manifests through a tonic pupil—one that is dilated and reacts sluggishly to light.
The cause of Adie Syndrome remains somewhat elusive but is believed to involve damage to certain nerve fibers in the eye. This disruption can lead to impaired pupillary constriction and altered reflexes throughout the body.
“Can Abandoned Child Syndrome Affect Adult Life? Signs & Recovery Guide”
Individuals with this syndrome may experience not only visual disturbances but also abnormal deep tendon reflexes. These symptoms highlight how intricately connected our nervous system is and how disruptions can manifest physically.
While often benign, individuals with Adie Syndrome should be mindful of their symptoms, as they can affect quality of life in various ways. Understanding these aspects lays the groundwork for better insights into its management and implications.
The History of Adie Syndrome: From Discovery to Modern Understanding
Adie Syndrome was first described in 1931 by Dr. William James Adie, a British neurologist. His observations of patients with unusual pupillary responses and absent reflexes laid the foundation for understanding this condition.
Initially considered rare, advancements in neurological research have unveiled more about its prevalence and mechanisms. Early studies focused on the implications of tonic pupils but lacked comprehensive insights into associated symptoms.
“What Is Abruzzo-Erickson Syndrome? Understanding This Rare Genetic Condition”
Over decades, researchers connected autonomic nervous system dysfunction to Adie Syndrome’s clinical presentation. This broadened our understanding beyond just ocular symptoms to include systemic effects like sweating abnormalities.
Modern diagnostic techniques have further clarified its characteristics, allowing healthcare providers to better identify and manage cases. As knowledge grows, so does awareness among medical professionals about how Adie Syndrome affects daily life for those affected.
Pathophysiology of Adie Syndrome: Autonomic Nervous System Involvement
Adie Syndrome primarily involves the dysfunction of the autonomic nervous system, particularly affecting the ciliary ganglion. This ganglion plays a crucial role in controlling pupil size and reaction to light.
A key feature is the impairment of parasympathetic pathways. These pathways are responsible for constricting pupils when exposed to bright light or focusing on nearby objects.
“Achard-Thiers Syndrome: Why Does It Cause Diabetes & Hirsutism in Women?”
When these signals falter, it results in a tonic pupil that reacts sluggishly or not at all. The disruption also extends to deep tendon reflexes due to similar autonomic involvement.
Neurons may become damaged or degenerate over time, leading to altered signaling mechanisms throughout the body. This can contribute to other symptoms such as abnormal sweating and cardiovascular responses, showcasing how interconnected bodily functions are within this syndrome. Understanding these underlying processes helps illuminate why individuals with Adie Syndrome experience their specific symptoms.
Clinical Features of Adie Syndrome: Tonic Pupil and Tendon Reflexes
Adie Syndrome presents with distinctive clinical features, most notably the tonic pupil. This condition results in an abnormally dilated pupil that reacts sluggishly to light but constricts slowly during accommodation. Patients often find bright lights uncomfortable due to this sensitivity.
“What Causes ARDS (Acute Respiratory Distress Syndrome)? Complete Guide”
Another hallmark of Adie Syndrome is diminished or absent deep tendon reflexes. Reflex responses may be significantly weakened, affecting movements and coordination.
These characteristics arise from involvement of the autonomic nervous system and can lead to further complications. While some patients experience only mild symptoms, others might face challenges impacting their daily activities.
The combination of these signs offers a unique insight into how Adie Syndrome manifests clinically, emphasizing its impact on both visual function and motor responses. Understanding these features aids healthcare professionals in diagnosing and managing this complex neurological condition effectively.
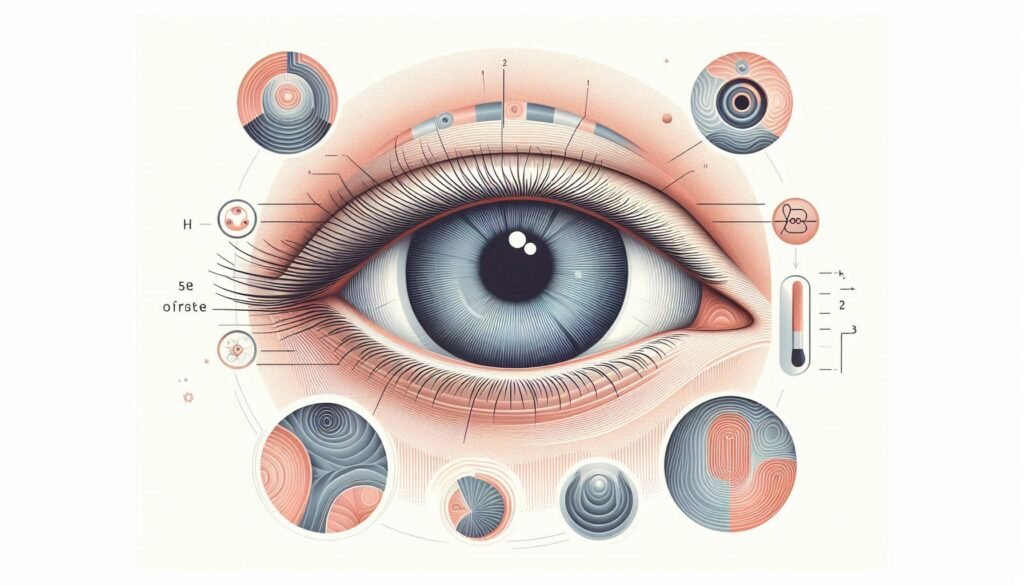
The Characteristic Tonic Pupil: Appearance and Pupillary Response
The tonic pupil is a hallmark feature of Adie Syndrome. It presents as an enlarged, irregularly shaped pupil that reacts sluggishly to light. This distinctive appearance can often be confusing for those unfamiliar with the condition.
“How Does Adams-Oliver Syndrome Affect Development? Expert Explained”
When exposed to bright light, the tonic pupil constricts slowly and may not fully close, leading to a noticeable difference from the unaffected eye. In dim lighting conditions, however, it might respond somewhat better due to increased sympathetic tone.
During accommodation tasks—like focusing on near objects—the pupillary reaction is typically impaired or absent altogether. This lack of response can lead to visual challenges for individuals living with this syndrome.
Patients may also experience photophobia or sensitivity to bright lights because of their compromised ability to adjust pupil size effectively. Understanding these characteristics is crucial in recognizing Adie Syndrome early and facilitating appropriate management strategies.
Absent or Diminished Deep Tendon Reflexes in Adie Syndrome
Absent or diminished deep tendon reflexes are a hallmark of Adie Syndrome. This neurological condition primarily affects the autonomic nervous system, leading to noticeable changes in reflex responses.
Patients often experience reduced or absent knee and ankle jerks. These diminished reactions occur due to impaired communication between peripheral nerves and the spinal cord. The loss of these reflexes can impact balance and coordination.
“What Is Adie Syndrome & Why Does It Affect Your Pupils? Complete Guide”
The absence of normal reflexive action may not be immediately apparent. Clinicians typically assess these during routine examinations, using tools like hammers for testing.
Interestingly, while some individuals might feel no symptoms from this deficiency, others could notice increased fatigue or difficulty with certain movements. Understanding these variations is crucial for proper management and support strategies tailored to each patient’s needs.
Associated Symptoms: Sweating Abnormalities and Cardiovascular Effects
Adie Syndrome is often accompanied by a range of associated symptoms beyond the hallmark tonic pupil. One notable feature includes sweating abnormalities. Patients may experience either excessive sweating or reduced perspiration, particularly in areas such as the hands and feet.
These fluctuations occur due to disruptions in autonomic regulation. The sympathetic nervous system’s involvement can lead to an imbalance that affects sweat glands differently among individuals.
Cardiovascular effects are also common in those with Adie Syndrome. Many patients report changes in heart rate and blood pressure regulation, potentially leading to episodes of dizziness or lightheadedness upon standing up quickly.
For some, these cardiovascular symptoms might contribute to feelings of fatigue or discomfort during physical activities. Understanding these additional signs is crucial for comprehensive management and improving daily living conditions for those affected by this neurological condition.
Diagnosing Adie Syndrome: Clinical Examination and Special Tests
Diagnosing Adie Syndrome typically begins with a thorough clinical examination. An eye specialist will assess the pupil’s size and reactivity to light. The classic presentation is a dilated tonic pupil that responds poorly to light but reacts better during accommodation.
Additional tests, such as the Holmes-Adie test, may be performed. This involves observing the reaction of both pupils under different lighting conditions. A distinctive feature of this syndrome is the unequal dilation between eyes.
Doctors often check deep tendon reflexes during the examination. Diminished or absent reflexes can help support a diagnosis of Adie Syndrome.
Specialized imaging and laboratory tests are generally not required for initial diagnosis but may assist in ruling out other conditions when necessary. Accurate observation by medical professionals plays a critical role in confirming this neurological disorder.
Pharmacological Testing in Adie Syndrome Diagnosis
Pharmacological testing plays a vital role in diagnosing Adie Syndrome. The most commonly used agent is pilocarpine, which mimics the action of acetylcholine on the eye’s muscles.
When administered topically, this medication causes constriction of the pupil. In individuals with Adie Syndrome, the tonic pupil will react more significantly to pilocarpine than a normal pupil would. This hypersensitivity can help healthcare providers confirm their suspicions about an underlying autonomic nervous system disorder.
Another useful pharmacological test involves using cocaine eye drops. Normally, cocaine inhibits reuptake at adrenergic synapses and should dilate healthy pupils. However, in cases of Adie Syndrome, there is little or no dilation due to decreased sympathetic innervation.
These tests provide crucial information that assists doctors in making accurate diagnoses while distinguishing Adie Syndrome from other similar conditions affecting pupillary response.
Differential Diagnosis: Distinguishing Adie Syndrome from Similar Conditions
Differential diagnosis is crucial for accurately identifying Adie Syndrome. Several conditions share similar symptoms, making it essential to distinguish them.
One such condition is Horner’s syndrome. This disorder affects the sympathetic nerves and can lead to a constricted pupil, unlike the dilated tonic pupil seen in Adie’s Syndrome.
Another potential mimic is third cranial nerve palsy, which may present with ptosis and ophthalmoplegia but typically does not exhibit the same pupillary response patterns associated with Adie’s.
Neurological disorders like multiple sclerosis or diabetic neuropathy also need consideration. These can cause autonomic dysfunction but often have additional neurological signs that differ from those in Adie’s.
A thorough clinical assessment combined with specific tests helps clarify these distinctions. Identifying accompanying symptoms ensures proper management strategies are implemented for each unique case.
The Natural History of Adie Syndrome: Progression and Long-term Outlook
Adie Syndrome is characterized by a generally benign course. Many patients experience stability in their symptoms over time. However, some individuals may notice gradual changes.
The progression can vary significantly from person to person. While tonic pupil and absent reflexes remain the hallmark features, additional autonomic dysfunction might emerge in certain cases.
Long-term outlook for those with Adie Syndrome is typically positive. Most individuals maintain functional independence throughout their lives. Symptoms often do not severely impact daily activities or overall well-being.
Regular follow-ups are essential to monitor any potential complications or new developments. Awareness of associated conditions can aid early intervention when necessary, ensuring the best quality of life for affected individuals.
Management Strategies for Adie Syndrome: Symptomatic Treatment
Managing Adie Syndrome focuses primarily on symptomatic treatment. Since the condition affects the autonomic nervous system, addressing individual symptoms is essential to improve quality of life.
For those experiencing light sensitivity due to tonic pupil, sunglasses or photochromatic lenses can provide relief. These aids help reduce glare and make outdoor environments more comfortable.
Patients with difficulties in accommodation may benefit from visual aids like reading glasses. This helps individuals engage in daily tasks without straining their eyes.
Physical therapy might also play a role for patients with diminished tendon reflexes. Gentle exercises can enhance mobility and strength while preventing muscle stiffness.
Additionally, monitoring cardiovascular signs is crucial as some patients report fluctuations in heart rate or blood pressure. Regular check-ups ensure that any emerging issues are addressed promptly.
Educating patients about stress management techniques can further alleviate symptoms tied to anxiety or discomfort related to their condition.
Ocular Management: Dealing with Light Sensitivity and Accommodation Issues
Light sensitivity, or photophobia, is a common issue for those with Adie Syndrome. This can significantly affect daily activities. Individuals often find bright lights uncomfortable and may squint or avoid them altogether.
To manage this symptom, wearing tinted glasses can provide relief. Specialized lens coatings help reduce glare and enhance visual comfort. Additionally, using hats or visors in sunny environments can minimize exposure to harsh light.
Accommodation issues present another challenge. Patients may experience difficulty focusing on nearby objects due to the tonic pupil’s response delay. Vision therapy exercises designed by eye care professionals can help strengthen accommodation abilities over time.
Regular check-ups with an ophthalmologist are essential for monitoring changes in vision and addressing any new concerns promptly. By implementing these strategies, individuals with Adie Syndrome can improve their ocular comfort and overall quality of life.
The Role of Pilocarpine in Managing Adie’s Tonic Pupil
Pilocarpine is a cholinergic agonist commonly used in managing Adie’s tonic pupil. This medication works by stimulating the sphincter muscle of the iris, which can help reduce pupil size and improve light sensitivity.
Patients with Adie syndrome often experience discomfort due to their dilated pupils. Pilocarpine alleviates this issue, making it easier for them to tolerate bright environments. Administered as eye drops, its effects can be both immediate and lasting.
While pilocarpine effectively addresses the cosmetic and functional aspects of a tonic pupil, it may have side effects such as brow ache or increased salivation. Therefore, dosage should be carefully monitored by an eye care professional.
Regular follow-ups are essential to assess treatment efficacy and adjust dosages accordingly. For many patients, pilocarpine represents a lifeline in managing day-to-day challenges posed by Adie’s tonic pupil.
Neurological Monitoring in Adie Syndrome Patients
Neurological monitoring is crucial for patients with Adie Syndrome. Regular assessments help track the progression of symptoms and manage their impact on daily life.
Clinicians typically evaluate pupillary responses and reflexes during appointments. This approach allows healthcare providers to observe any changes over time. Enhanced vigilance ensures timely intervention if complications arise.
Patients may benefit from tailored neuropsychological evaluations as well. These can identify cognitive impacts related to autonomic dysfunction, adding another layer to management strategies.
Digital tools are increasingly being utilized in monitoring this condition. Wearable devices can record physiological data, providing real-time insights into patient health metrics that might otherwise go unnoticed.
Collaborative care among specialists also plays a significant role. Neurologists, ophthalmologists, and primary care physicians should work together to create comprehensive plans addressing both neurological and ocular aspects of Adie Syndrome.
Adie Syndrome and Quality of Life: Coping with Daily Challenges
Living with Adie Syndrome can bring a unique set of challenges. Patients often face daily hurdles related to their symptoms, impacting various aspects of life.
One common issue is light sensitivity. This can make bright environments uncomfortable and difficult to navigate. Wearing sunglasses or hats can help mitigate these effects outdoors.
Additionally, the altered pupillary response affects vision, making tasks like reading or driving more challenging. Using adaptive technologies may enhance comfort and safety in these situations.
Social interactions might also be influenced by associated symptoms such as sweating abnormalities. Strategies for managing embarrassment or discomfort in social settings are essential for maintaining relationships.
Support groups offer valuable resources where individuals share experiences and coping techniques. Connecting with others facing similar challenges fosters understanding and reduces feelings of isolation as one navigates life with Adie Syndrome.
Rare Complications and Associations of Adie Syndrome
Adie Syndrome can present with rare complications that extend beyond its primary features. One notable association is the occurrence of Horner’s syndrome, which affects the sympathetic nervous system and may lead to ptosis (drooping eyelid) or miosis (constricted pupil).
Another complication involves ocular motility disorders. Patients might experience difficulties in eye movements, contributing to visual disturbances. This can significantly impact daily activities, such as reading or driving.
Additionally, some individuals report gastrointestinal issues like gastroparesis, where gastric emptying is delayed. This condition can lead to nausea and bloating after meals.
There are also anecdotal reports linking Adie Syndrome with autoimmune conditions such as lupus or Sjögren’s syndrome. These associations warrant further research for better understanding and management options.
Psychological impacts should not be overlooked. Anxiety about symptoms could arise due to visible signs like a dilated pupil or associated discomforts.
Genetic Factors in Adie Syndrome: Current Research and Insights
Recent studies have begun to explore the genetic underpinnings of Adie Syndrome. While the exact cause remains elusive, researchers are analyzing potential hereditary factors that may contribute to its development.
One area of interest involves mutations in genes related to neuronal function and survival. These mutations could disrupt normal autonomic nervous system operations, leading to symptoms characteristic of Adie Syndrome.
Genome-wide association studies (GWAS) have identified several candidate loci associated with neuropathies. This research is crucial for understanding how certain individuals might be predisposed to this condition.
Current insights suggest a multifactorial approach where genetics interact with environmental elements. Understanding these relationships can pave the way for targeted therapies or preventive strategies in vulnerable populations.
As research continues, future findings may shed light on personalized management approaches tailored to an individual’s genetic makeup.
Adie Syndrome in Special Populations: Children and Elderly
Adie Syndrome can manifest differently across various demographics, particularly among children and the elderly. In children, the condition may go unnoticed for some time due to its subtle symptoms. Parents might attribute difficulties with vision or attention issues to typical childhood behavior rather than a neurological concern. Early diagnosis is essential in this population to ensure appropriate management and support.
For elderly individuals, Adie Syndrome can complicate existing health conditions. The aging process often brings about changes in autonomic function; thus, identifying Adie’s unique characteristics becomes crucial for effective treatment strategies. Symptoms such as light sensitivity might be dismissed as age-related problems when they could indicate an underlying issue related to Adie Syndrome.
Both groups require tailored approaches when managing this condition. Pediatric assessments should focus on behavioral observations and visual acuity tests along with thorough neurological evaluations. For older adults, regular monitoring of their neurologic status is necessary since comorbidities can influence symptom presentation.
Research into genetic factors continues to provide insights into how these populations are affected by Adie Syndrome differently. Understanding these nuances helps healthcare providers deliver more personalized care while improving quality of life for those living with this condition at any age.

