Introduction to Abdominal Compartment Syndrome (ACS)
Abdominal Compartment Syndrome (ACS) is a critical condition that can arise unexpectedly, often leading to severe consequences if not promptly addressed. As pressure builds within the abdominal cavity, vital organs may be compromised, jeopardizing patient health and recovery.
Understanding ACS is essential for healthcare professionals and caregivers alike. In this blog post, we will delve into everything you need to know about Abdominal Compartment Syndrome—from its anatomy and causes to diagnosis and treatment options—equipping you with valuable insights for better patient outcomes.
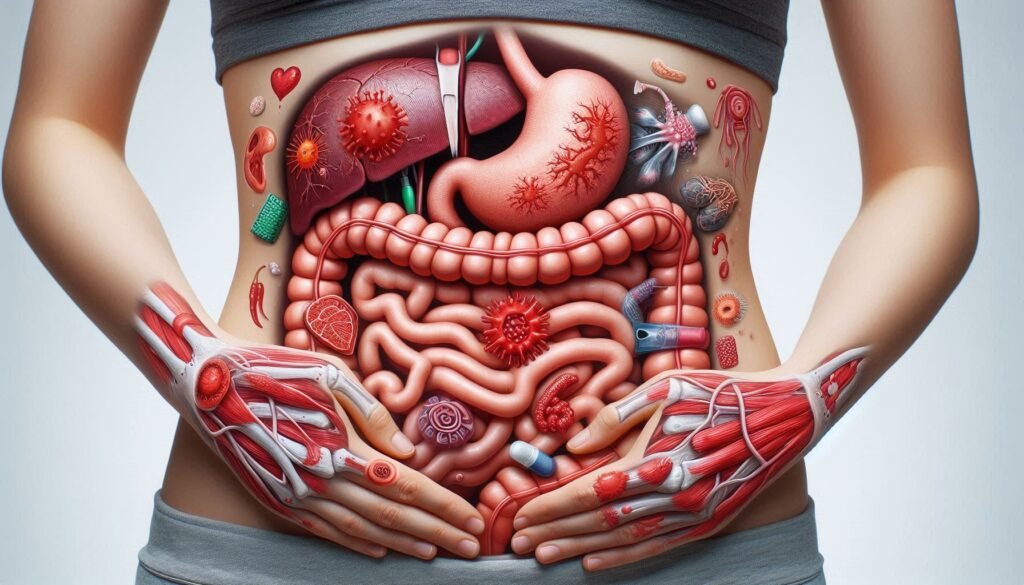
Understanding the Anatomy of the Abdominal Cavity
The abdominal cavity is a complex space that houses vital organs. It lies between the diaphragm and the pelvic floor, protected by muscles and connective tissues. The major structures within this cavity include the stomach, liver, intestines, spleen, pancreas, and kidneys.
“How Does Seckel Syndrome Impact Growth?”
This anatomical arrangement allows for essential functions like digestion and waste elimination. The peritoneum, a thin membrane lining the cavity, plays a crucial role in protecting these organs. It produces serous fluid to reduce friction during movement.
Understanding this anatomy is key when discussing abdominal compartment syndrome (ACS). Increased pressure in this area can severely impact organ function and patient outcomes if not managed promptly.
Causes and Risk Factors of ACS
Abdominal Compartment Syndrome can arise from various causes. Trauma is a significant contributor, particularly in cases of blunt or penetrating injuries to the abdomen. Such incidents can lead to hemorrhage and swelling within the abdominal cavity.
Surgical procedures also pose risks for developing ACS. After major surgeries, patients may experience fluid accumulation or hematoma formation, which increases intra-abdominal pressure. Additionally, conditions like pancreatitis cause inflammation that can further complicate matters.
“What Are The Signs of Sandhoff Syndrome in Infants?”
Certain populations are more vulnerable to ACS development. Obesity significantly raises intra-abdominal pressure due to excess fat tissue. Similarly, critically ill patients with sepsis or severe burns face heightened risk factors that make them susceptible to this serious condition.
Signs and Symptoms of ACS
Patients with Abdominal Compartment Syndrome often exhibit a range of alarming signs. Increased abdominal pressure can lead to significant discomfort or pain, which may be disproportionate to any physical findings. This pain often worsens upon movement or palpation.
Other symptoms include decreased urine output and difficulty breathing due to diaphragm displacement from increased intra-abdominal pressure. Patients might also experience nausea, vomiting, and swelling in the abdomen.
“Why Does Schwartz-Jampel Syndrome Cause Muscle Stiffness?”
As ACS progresses, vital signs may deteriorate. Tachycardia and hypotension are common as blood flow is compromised. Early recognition of these symptoms is crucial for timely intervention and better patient outcomes. Prompt attention can significantly impact recovery rates in affected individuals.
Diagnosis and Diagnostic Tools for ACS
Diagnosing Abdominal Compartment Syndrome (ACS) requires a combination of clinical assessment and diagnostic tools. Physicians often start by evaluating the patient’s medical history, physical examination findings, and vital signs. A high index of suspicion is crucial in patients with risk factors or those exhibiting symptoms.
Intra-abdominal pressure (IAP) measurement is the gold standard for diagnosis. This can be done using a catheter placed into the bladder, allowing accurate monitoring of pressure changes within the abdominal cavity.
“How Does Shapiro Syndrome Affect Body Temperature?”
Imaging studies like ultrasound or CT scans may also assist in identifying underlying causes of ACS. These methods help visualize organ swelling, fluid collections, or other abnormalities that contribute to increased intra-abdominal pressure.
Three categories of ACS
Abdominal Compartment Syndrome (ACS) is classified into three categories based on its underlying causes. The first category is primary ACS, which typically arises from intra-abdominal pathology such as trauma or hemorrhage. This type often requires urgent intervention due to the immediate threat it poses.
“What Causes Sudden Infant Death Syndrome? Prevention Guide”
The second category, secondary ACS, occurs when increased intra-abdominal pressure develops as a complication of other medical conditions like sepsis or pancreatitis. These situations can escalate quickly and require careful monitoring.
There’s chronic ACS. This form develops gradually over time and may be seen in patients with ongoing abdominal issues like obesity or cirrhosis. It can lead to significant morbidity if not identified and managed effectively.
Treatment Options for ACS
Treatment for abdominal compartment syndrome focuses on relieving pressure and addressing underlying causes. Medical management includes optimizing fluid resuscitation, vasopressor support, and ensuring adequate ventilation. These measures can stabilize patients while assessing the need for further intervention.
“Why Does Takayasu’s Arteritis Syndrome Affect Blood Vessels?”
Surgical intervention is often necessary in severe cases. The most common approach is decompressive laparotomy, which involves opening the abdomen to reduce pressure. This procedure may also help identify any intra-abdominal injuries requiring attention.
Other therapies include careful monitoring of intra-abdominal pressure (IAP) and adjusting patient positioning to enhance comfort and circulation. Pain management strategies are essential, along with nutritional support to promote recovery during this critical period.
Medical Management
Medical management of Abdominal Compartment Syndrome focuses on stabilizing the patient and addressing underlying conditions. This approach often starts with optimizing fluid resuscitation to maintain adequate blood pressure while preventing organ dysfunction.
“How Does Tay-Sachs Syndrome Progress? Complete Guide”
Medications such as diuretics may be used cautiously to reduce intra-abdominal pressure, but close monitoring is essential. Analgesics help manage pain, allowing for better patient comfort and cooperation during treatment.
Additionally, sedation might be necessary for patients in severe distress or those requiring mechanical ventilation. Regular assessment of intra-abdominal pressure through catheters provides valuable data to guide therapy adjustments effectively. The goal is always to prevent complications while promoting recovery within a controlled environment.
Surgical Intervention
Surgical intervention is often necessary for severe cases of abdominal compartment syndrome. When conservative measures fail, a surgical approach may be the best option to relieve pressure on vital organs. This typically involves procedures like decompressive laparotomy.
During this procedure, a large incision is made in the abdominal wall to allow for expansion and reduce intra-abdominal pressure. This can significantly improve blood flow and organ function.
Post-operative care is crucial for monitoring recovery and ensuring that complications do not arise. Close observation helps detect any signs of infection or further complications early, allowing for timely interventions if needed.
Other Therapies (such as decompressive laparotomy)
Other therapies for Abdominal Compartment Syndrome (ACS) often focus on relieving pressure within the abdominal cavity. Decompressive laparotomy is a key intervention in severe cases. This surgical procedure involves making an incision in the abdomen to allow for expansion and pressure relief.
In addition to decompressive laparotomy, other techniques may include percutaneous drainage or use of negative-pressure wound therapy. Each option aims to reduce intra-abdominal pressure while promoting healing.
It’s essential that each patient’s situation is evaluated individually. The choice of therapy depends on multiple factors, including severity of ACS, overall health, and response to prior treatments. Proper selection can significantly improve patient outcomes.
Nursing Care and Considerations for Patients with ACS
Nursing care for patients with Abdominal Compartment Syndrome (ACS) is crucial. Regular monitoring of intra-abdominal pressure (IAP) is essential to track changes in the patient’s condition. This involves using specialized equipment and understanding normal IAP ranges.
Positioning and turning strategies can significantly impact patient comfort and outcomes. Maintaining optimal positioning helps reduce pressure on the abdomen, enhancing circulation and facilitating lung expansion.
Additionally, effective pain management should be prioritized to ensure patient comfort. This may involve administering prescribed analgesics or adjusting interventions based on individual needs. Nutritional support and fluid balance are also critical components of care, helping to stabilize the patient’s overall health during recovery from ACS.
Monitoring Intra-abdominal Pressure (IAP)
Monitoring intra-abdominal pressure (IAP) is crucial in managing abdominal compartment syndrome (ACS). Elevated IAP can lead to serious complications, making regular assessment essential for timely intervention.
There are various methods to measure IAP, including bladder pressure monitoring and direct measurement via catheters. The most commonly used technique involves placing a catheter in the bladder to accurately gauge pressure changes.
Healthcare providers should establish baseline values for each patient and monitor trends over time. Careful attention can help identify significant increases in IAP that require prompt medical or surgical response, ultimately improving patient outcomes and reducing morbidity associated with ACS.
Positioning and Turning Strategies
Proper positioning is crucial for patients with Abdominal Compartment Syndrome. Elevating the head of the bed can help improve diaphragmatic function, facilitating better lung expansion and oxygenation.
Frequent turning of the patient is essential to prevent pressure ulcers and enhance circulation. Rotating them every two hours can reduce tissue ischemia while also easing discomfort from prolonged immobility.
Utilizing specific turning devices or pillows can aid in achieving optimal positioning without compromising intra-abdominal pressure. Always assess each patient’s response to positional changes, as some may require individualized strategies tailored to their unique condition.
Pain Management
Pain management is a critical aspect of caring for patients with Abdominal Compartment Syndrome. Managing pain effectively can significantly improve patient comfort and promote recovery. It’s essential to assess pain levels regularly using standardized scales, ensuring timely interventions based on the patient’s needs.
Pharmacological approaches often include opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and adjunct medications like gabapentin or ketamine for nerve-related discomfort. Dosing should be carefully monitored due to potential side effects, especially in this vulnerable population.
Non-pharmacological methods can also play a role in alleviating pain. Techniques such as relaxation exercises, guided imagery, and physical therapy may help enhance overall well-being while reducing reliance on medications.
Nutritional Support and Fluid Balance
Nutritional support is vital for patients with Abdominal Compartment Syndrome. Adequate nutrition aids in healing and maintaining overall health. A tailored dietary plan should focus on proteins, vitamins, and minerals to promote recovery.
Fluid balance is equally crucial in managing ACS. Monitoring fluid intake and output helps prevent complications like dehydration or overhydration. Adjustments may be necessary based on the patient’s response to treatment.
Healthcare providers must assess electrolyte levels regularly. Imbalances can worsen the condition or complicate recovery efforts. By ensuring proper nutritional support and fluid management, outcomes for patients can significantly improve during their care journey.
Potential Complications of ACS and How to Prevent Them?
Abdominal Compartment Syndrome (ACS) can lead to serious complications if not addressed promptly. One major risk is organ failure, as elevated pressure can restrict blood flow and oxygen delivery to vital organs. This may result in long-term damage or even death.
Another concern is the development of abdominal compartment syndrome-related infections. The compromised tissue environment creates a breeding ground for bacteria, increasing the likelihood of sepsis.
Preventing these complications involves regular monitoring of intra-abdominal pressure and quick interventions when ACS is suspected. Healthcare providers should also implement strategies such as early decompression and maintaining optimal fluid balance to mitigate risks associated with this condition.
Long-Term Outcomes for Patients with ACS
Long-term outcomes for patients with abdominal compartment syndrome (ACS) can vary widely. Many factors influence recovery, including the severity of ACS, promptness of treatment, and underlying health conditions. Some patients may experience significant improvements in their quality of life after effective management.
However, complications can arise even after successful interventions. Issues such as chronic pain, organ dysfunction, or psychological effects might persist. Continuous monitoring and follow-up care are essential for mitigating these risks.
Rehabilitation plays a crucial role in patient recovery. Tailored programs focusing on physical therapy and nutritional support help restore strength and overall well-being. Engaging healthcare teams ensures comprehensive care throughout the long-term journey post-ACS diagnosis.
Patient
Patients with Abdominal Compartment Syndrome require close monitoring and tailored interventions. Understanding their unique needs is crucial for optimal recovery. Each case can vary significantly, making individualized care essential.
Communication plays a vital role in managing patients effectively. Encourage them to express their symptoms and concerns openly, as this enhances the quality of care provided. Support from healthcare providers can ease anxiety during treatment.
Education about ACS empowers patients to participate actively in their own recovery process. Providing clear information on what to expect helps demystify the experience and fosters trust between the patient and healthcare team. Engaging patients leads to better adherence to treatment plans, ultimately improving outcomes.
Summary and Conclusion
Abdominal Compartment Syndrome (ACS) is a serious condition that requires prompt recognition and intervention. Understanding the anatomy of the abdominal cavity, as well as the causes and risk factors, can aid in early detection.
Recognizing signs and symptoms is critical for timely diagnosis. Healthcare professionals must be familiar with diagnostic tools to assess intra-abdominal pressure effectively.
Treatment options range from medical management to surgical interventions like decompressive laparotomy. Each approach aims to relieve pressure and restore normal function.
Nursing care plays a pivotal role in patient outcomes. Monitoring intra-abdominal pressure, ensuring proper positioning, managing pain, and maintaining nutritional support are essential strategies.
Potential complications of ACS can impact recovery; thus preventive measures should be prioritized. Long-term outcomes depend on swift treatment and effective nursing care.
Understanding these facets of Abdominal Compartment Syndrome equips healthcare providers with valuable knowledge that enhances patient safety and improves overall health outcomes.

