Irritable Bowel Syndrome (IBS) is a term that often elicits confusion and concern among those who hear it. For many, it’s not just a casual inconvenience but a daily reality filled with discomfort and uncertainty. Characterized by symptoms such as abdominal pain, bloating, and changes in bowel habits, IBS affects millions of people worldwide—but what exactly does this functional gut disorder entail?
As awareness around digestive health grows, so does the need for comprehensive knowledge about IBS. Understanding its nuances can empower individuals to take control of their symptoms and improve their quality of life. In this blog post, we’ll navigate through the complexities surrounding Irritable Bowel Syndrome—from its definitions and prevalence to treatment options that aim to restore balance within the body.
Join us on this informative journey as we delve deeper into the world of IBS—because understanding your gut is key to feeling better!
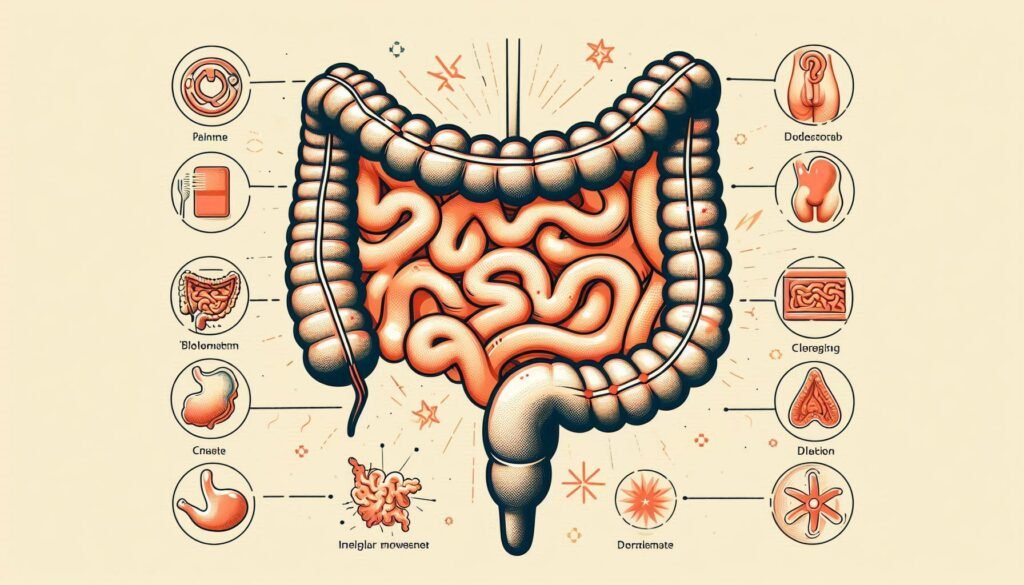
Defining Irritable Bowel Syndrome
Irritable Bowel Syndrome (IBS) is a chronic functional gastrointestinal disorder. It primarily affects the large intestine and disrupts normal bowel function. Unlike other digestive disorders, IBS does not cause visible damage to the intestines.
The hallmark of IBS is its diverse range of symptoms, which can vary significantly from person to person. Common complaints include abdominal discomfort, bloating, gas, diarrhea, or constipation. These symptoms often fluctuate over time and may even occur in flare-ups.
“Why Does Quebec Platelet Disorder Affect Blood Clotting?”
IBS tends to be categorized as a syndrome rather than a disease due to this variability in presentation. There’s no single test for diagnosis; instead, it relies on clinical criteria and symptom evaluation.
Understanding IBS requires recognizing that it’s more than just an upset stomach—it’s a complex interplay between gut health and overall well-being that can profoundly impact daily life.
Prevalence and Demographics of IBS
Irritable Bowel Syndrome (IBS) affects millions worldwide, making it one of the most common gastrointestinal disorders. Studies suggest that around 10-15% of the global population experience symptoms related to IBS.
This condition is notably more prevalent in women than men. Estimates indicate that women are about two to three times more likely to be diagnosed with IBS. Factors contributing to this disparity may include hormonal differences and psychological stressors.
“How Does Quincke’s Edema Syndrome Cause Swelling?”
Age also plays a role; IBS can occur at any age but often begins in late adolescence or early adulthood. Interestingly, many cases remain undiagnosed due to stigmas surrounding digestive issues or a lack of awareness among healthcare providers.
IBS crosses ethnic and cultural boundaries, impacting diverse populations globally. Understanding its demographics helps tailor effective management strategies for those affected by this multifaceted disorder.
Pathophysiology: Brain-Gut Axis Dysfunction
The brain-gut axis is a complex communication network linking the central nervous system and the gastrointestinal tract. This connection plays a vital role in regulating gut function.
In individuals with Irritable Bowel Syndrome (IBS), this relationship often becomes dysregulated. The brain may misinterpret signals from the gut, leading to abnormal motility and heightened sensitivity.
“What Causes Qigong-Induced Psychotic Syndrome?”
Neurotransmitters like serotonin are key players in this interaction. Approximately 90% of serotonin is produced in the gut, influencing both mood and digestive processes. Disruptions in serotonin levels can contribute to IBS symptoms.
Additionally, stress impacts this axis significantly. Psychological factors can trigger or exacerbate gastrointestinal issues, creating a feedback loop between emotional health and gut function.
Understanding how these systems interact offers insights into managing IBS effectively through targeted treatments that address both physical and psychological aspects of care.
Types of IBS: IBS-D, IBS-C, and IBS-M
Irritable Bowel Syndrome (IBS) presents in three primary types, each characterized by distinct bowel movement patterns.
IBS-D, or diarrhea-predominant IBS, involves frequent loose stools and urgency. Those affected may experience distressing symptoms that can significantly impact their daily life.
On the other hand, IBS-C stands for constipation-predominant IBS. Individuals with this type often struggle with infrequent bowel movements and discomfort from bloating and straining during episodes.
“Why Does Quick Syndrome Affect Heart Rhythm?”
There’s IBS-M, which is a mixed form of the disorder. People with IBS-M face alternating bouts of both diarrhea and constipation. This inconsistency adds another layer of complexity to managing their symptoms effectively.
Understanding these subtypes is crucial for tailoring treatment approaches to address specific challenges within each group effectively.
Common Symptoms and Clinical Presentation
Irritable Bowel Syndrome (IBS) presents a range of symptoms that can vary significantly from person to person. Abdominal pain is one of the hallmark signs, often alleviated by bowel movements.
Many individuals experience altered bowel habits, including diarrhea or constipation, leading to a subtype classification of IBS. Some may alternate between both types, adding complexity to their experiences.
“How Does Quirke’s Syndrome Impact Development?”
Bloating and gas are also common complaints. This uncomfortable sensation can be distressing and contribute to the overall impact on daily life.
In addition, people with IBS frequently report an urgency for bowel movements along with feelings of incomplete evacuation. Fatigue and difficulty sleeping may accompany these gastrointestinal issues as well.
The interplay of these symptoms significantly affects quality of life for those living with this functional gut disorder. Understanding them is essential in managing IBS effectively.
Diagnostic Criteria: Rome IV Guidelines
The Rome IV criteria provide a standardized approach to diagnosing Irritable Bowel Syndrome (IBS). Established by the Rome Foundation, these guidelines emphasize symptom-based diagnosis rather than invasive testing.
To meet the criteria for IBS, patients must experience recurrent abdominal pain on average at least one day per week over three months. This pain should be associated with two or more of the following: discomfort related to bowel movements, changes in stool frequency, or alterations in stool form.
“What Triggers Rasmussen Syndrome? Brain Disorder Guide”
These specific requirements help healthcare providers distinguish IBS from other gastrointestinal disorders. The focus on symptoms allows for a more accurate and timely diagnosis, which is crucial for effective management strategies tailored to individual needs. Understanding these guidelines can empower patients to engage in meaningful discussions with their healthcare professionals about their symptoms and concerns regarding IBS.
Differential Diagnosis and Exclusion of Other Conditions
Differential diagnosis is crucial when diagnosing Irritable Bowel Syndrome (IBS). Symptoms can overlap with various gastrointestinal disorders, making accurate identification essential.
Conditions such as inflammatory bowel disease (IBD), celiac disease, and infections must be ruled out first. Each of these has distinct characteristics that differ from IBS. For instance, IBD often presents with bloody diarrhea and weight loss.
Functional dyspepsia and gastroesophageal reflux disease (GERD) can also mimic IBS symptoms. Patients may report abdominal discomfort or bloating in both cases.
Healthcare providers typically conduct a thorough medical history review and physical examination to differentiate these conditions. Blood tests, stool tests, or imaging studies might be necessary for further investigation.
By carefully excluding other potential causes of symptoms, practitioners ensure that patients receive the most appropriate treatment tailored specifically for their needs related to IBS.
Triggers and Exacerbating Factors
Irritable Bowel Syndrome (IBS) can be influenced by a range of triggers that exacerbate symptoms. These factors often vary from person to person, making management challenging.
Diet plays a significant role in IBS flare-ups. Common culprits include spicy foods, caffeine, alcohol, and high-fat meals. Individuals may find certain food additives or preservatives worsen their condition as well.
Stress is another powerful trigger. Stressful situations can lead to increased bowel sensitivity and spasms. The relationship between mental health and gut function is intricate; anxiety and depression frequently accompany IBS.
Hormonal fluctuations are also noteworthy for women with IBS. Many report symptom exacerbation during menstruation due to hormonal changes affecting gut motility.
Lifestyle choices like irregular sleeping patterns can further contribute to symptom severity. Understanding these triggers helps in creating tailored management plans for those living with IBS.
Role of Stress and Psychological Factors
Stress plays a significant role in the onset and exacerbation of Irritable Bowel Syndrome (IBS). The gut-brain axis is a complex communication network between the gastrointestinal tract and the brain. When stress levels rise, this connection can become dysregulated.
Psychological factors such as anxiety and depression often coexist with IBS. These conditions can amplify symptoms like abdominal pain and bloating. Individuals may find that stressful situations lead to flare-ups or more intense discomfort.
Coping mechanisms vary among individuals. Some might resort to unhealthy habits, further aggravating their condition. Others may benefit from mindfulness practices or relaxation techniques, which can help reduce overall stress levels.
Understanding this relationship highlights the importance of addressing both psychological health and gastrointestinal wellness in managing IBS effectively. A holistic approach that includes mental well-being could pave the way for improved symptom control.
Dietary Considerations and Food Sensitivities
Dietary considerations play a crucial role in managing Irritable Bowel Syndrome (IBS). Many individuals with IBS report specific food sensitivities that can trigger symptoms. Common culprits include dairy products, gluten, and certain high-fiber foods.
Identifying personal triggers is essential. Keeping a food diary can help track what you eat and how it affects your digestion. This method allows for better understanding over time.
Additionally, portion sizes matter. Eating smaller meals more frequently can ease the burden on the digestive system. It’s also important to stay hydrated by drinking plenty of water throughout the day.
Consulting with a healthcare professional or dietitian may provide valuable guidance tailored to individual needs. They can help create an elimination diet plan to pinpoint problematic foods while ensuring nutritional balance remains intact.
Low FODMAP Diet and Its Efficacy
The Low FODMAP diet has gained recognition as an effective management strategy for Irritable Bowel Syndrome (IBS). FODMAP stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. These short-chain carbohydrates can trigger symptoms in sensitive individuals.
This dietary approach involves three phases: elimination, reintroduction, and personalization. Initially, high-FODMAP foods are removed from the diet to alleviate symptoms. After a period of symptom relief, certain foods are gradually reintroduced to identify specific triggers.
Research shows that many people with IBS experience significant improvement in symptoms such as bloating and abdominal pain when following this diet. It empowers patients by helping them understand their food sensitivities better.
However, it’s essential to undertake this dietary change under professional guidance. This ensures nutritional balance while effectively managing IBS symptoms without unnecessary restrictions over the long term.
Pharmacological Treatment Options
Pharmacological treatment options for Irritable Bowel Syndrome (IBS) can vary based on the specific type of IBS a patient experiences. For those with IBS-D (diarrhea predominant), medications like loperamide may provide immediate relief by slowing intestinal transit.
In contrast, patients suffering from IBS-C (constipation predominant) often benefit from laxatives or newer agents such as linaclotide and plecanatide. These drugs help increase bowel movements and alleviate discomfort.
Antidepressants are also frequently prescribed for their dual role in pain management and mood stabilization. Low doses of tricyclic antidepressants can reduce visceral hypersensitivity, which is common in IBS sufferers.
Additionally, rifaximin, an antibiotic targeting small intestine bacterial overgrowth, has shown promise in relieving symptoms for some patients. Each medication comes with its own set of potential side effects; thus, consultations with healthcare providers are essential to tailor treatments effectively.
Probiotics and Gut Microbiome Modulation
Probiotics play a crucial role in managing Irritable Bowel Syndrome (IBS) by modulating the gut microbiome. These live microorganisms can restore balance among gut bacteria, improving overall digestive health.
Research indicates that certain probiotic strains may alleviate IBS symptoms such as bloating and abdominal pain. Lactobacillus and Bifidobacterium species are commonly studied for their beneficial effects on gut function.
Incorporating probiotics into your diet can be achieved through supplements or fermented foods like yogurt, kefir, and sauerkraut. Regular consumption might enhance gut flora diversity, which is vital for optimal digestion.
However, responses to probiotics vary among individuals with IBS. This variability underscores the importance of personalized approaches when selecting specific strains or products tailored to individual needs. Understanding how these organisms interact with our bodies opens new avenues for symptom management in those living with this complex condition.
Cognitive Behavioral Therapy for IBS
Cognitive Behavioral Therapy (CBT) has gained recognition as an effective treatment for Irritable Bowel Syndrome (IBS). This therapeutic approach focuses on identifying and changing negative thought patterns that contribute to stress and anxiety, which can exacerbate IBS symptoms.
During CBT sessions, patients learn coping strategies to manage their reactions to discomfort. By addressing the psychological aspects of IBS, individuals often find relief from both physical symptoms and mental distress. Techniques may include relaxation exercises, mindfulness practices, and guided imagery.
Research suggests that patients who engage in CBT report improvements in their overall quality of life. They experience fewer flare-ups and enhanced emotional well-being. As a non-invasive option, CBT offers hope for those struggling with the daily challenges posed by IBS while promoting long-term health benefits.
Hypnotherapy and Relaxation Techniques
Hypnotherapy is gaining attention as a complementary approach for managing Irritable Bowel Syndrome (IBS). This technique involves guided relaxation and focused concentration. It aims to create a state of heightened awareness where patients can explore their thoughts and feelings about their symptoms.
Research indicates that hypnotherapy may help reduce pain and improve overall gut function. By addressing the brain-gut connection, it targets psychological aspects often linked with IBS flare-ups.
Relaxation techniques such as deep breathing, progressive muscle relaxation, and mindfulness meditation also play a crucial role in symptom management. These practices can lower stress levels, which are significant triggers for many individuals suffering from IBS.
Incorporating these methods into daily routines can enhance emotional well-being. Patients often report improved coping strategies when facing the challenges of living with IBS.
Exercise and Physical Activity Benefits
Exercise plays a crucial role in managing Irritable Bowel Syndrome (IBS). Regular physical activity can help alleviate symptoms and improve overall gut function.
Engaging in moderate exercise promotes better digestion by stimulating intestinal contractions. This can reduce bloating and discomfort commonly associated with IBS.
Additionally, exercise is an excellent stress reliever. Since stress often exacerbates IBS symptoms, activities like walking, swimming, or yoga can lead to significant improvements.
Moreover, physical activity increases the release of endorphins. These natural mood lifters contribute to emotional well-being and may lessen anxiety related to bowel issues.
Maintaining a healthy weight through regular exercise can positively impact gut health. It helps balance hormones that regulate digestion and metabolism. Prioritizing movement may enhance your quality of life while living with IBS.
Complementary and Alternative Therapies
Complementary and alternative therapies are gaining traction among individuals with Irritable Bowel Syndrome (IBS). Many seek these approaches to alleviate symptoms when conventional treatments fall short.
Acupuncture is one popular option. This ancient practice may help reduce abdominal pain and improve gut function through targeted stimulation of specific points on the body.
Herbal remedies also play a role in managing IBS symptoms. Peppermint oil, for example, has shown promise in soothing digestive discomfort. Similarly, ginger can aid digestion and relieve nausea.
Mind-body techniques like yoga and tai chi promote relaxation. They not only enhance flexibility but also help manage stress, which can exacerbate IBS symptoms.
Dietary supplements such as prebiotics and omega-3 fatty acids have gained attention for their potential to support gut health. Each person’s experience with these therapies can vary widely, making it essential to consult healthcare professionals for tailored recommendations.
Impact on Quality of Life and Daily Functioning
Irritable Bowel Syndrome (IBS) significantly affects the quality of life for many individuals. Those living with IBS often experience unpredictable symptoms, which can lead to anxiety and social withdrawal.
Daily activities such as work, school, or social events may become challenging. The fear of an urgent need for a restroom can deter people from engaging in outings or traveling. This sense of uncertainty creates a constant emotional burden.
The impact extends beyond physical discomfort. Relationships can suffer due to misunderstandings about this invisible condition. Friends and family might not grasp the severity of daily struggles faced by someone with IBS.
Mental health is also affected; stress and frustration are common companions for those managing IBS symptoms. Individuals may find themselves caught in a cycle where mental strain exacerbates gut issues, making effective management more complex.
Management of IBS in Special Populations
Managing Irritable Bowel Syndrome (IBS) in special populations, such as children, the elderly, and pregnant women, requires tailored approaches. Each group has unique considerations that can influence treatment.
For children with IBS, parental involvement is crucial. Educating families about dietary modifications and stress management techniques fosters a supportive environment conducive to symptom relief.
Elderly individuals may experience polypharmacy or have comorbidities affecting gut health. Careful assessment of medications is essential to avoid exacerbating IBS symptoms. Gentle exercise programs can improve mobility and digestion without overwhelming the body.
Pregnant women face hormonal shifts that can impact gastrointestinal function. Dietary adjustments should focus on fiber intake while ensuring adequate hydration for both mother and child’s well-being.
Each subgroup demands a nuanced understanding of their specific challenges when developing effective management strategies for IBS, emphasizing individualization in care plans.
Emerging Research and Novel Treatments
Emerging research in Irritable Bowel Syndrome (IBS) is paving the way for innovative treatments and a deeper understanding of this complex condition. Scientists are increasingly focusing on the gut microbiome’s role, exploring how specific bacterial populations influence IBS symptoms. This ongoing exploration may lead to targeted probiotic therapies tailored to individual needs.
Additionally, advances in genetic research are shedding light on potential hereditary links associated with IBS. Understanding these connections could enable healthcare providers to identify at-risk individuals earlier and implement preventative strategies.
Novel treatments such as biofeedback therapy and neuromodulation techniques show promise in managing symptoms more effectively. These approaches aim not only to alleviate discomfort but also enhance overall quality of life for those affected by IBS.
As studies continue, there’s hope that integrative methods combining pharmacological options with lifestyle interventions will provide a comprehensive approach for patients. The future looks brighter for those navigating the challenges of Irritable Bowel Syndrome, as new insights and therapies emerge from scientific inquiry into this functional gut disorder.