Pain is a universal experience, yet some forms of it remain shrouded in mystery. One such condition is Complex Regional Pain Syndrome (CRPS), an enigmatic disorder that affects countless individuals worldwide. Characterized by severe and sometimes debilitating pain, CRPS can significantly impact one’s quality of life. Understanding this complex condition is crucial for those affected and their loved ones.
Imagine feeling pain that extends far beyond the injury itself—pain that persists long after the initial trauma has healed. For many with CRPS, this is a daily reality. This blog post aims to shed light on CRPS, exploring its types, symptoms, causes, treatment options, and much more. Whether you’re seeking information for yourself or someone close to you who suffers from this condition, you’ll find valuable insights here to navigate the intricacies of Complex Regional Pain Syndrome effectively.
Defining Complex Regional Pain Syndrome
Complex Regional Pain Syndrome (CRPS) is a chronic pain condition that typically occurs following an injury, surgery, or trauma. It is marked by prolonged and intense pain that often exceeds the initial cause of the discomfort.
The syndrome primarily affects limbs but can manifest in other areas as well. CRPS is thought to arise from dysfunction in the nervous system, leading to abnormal responses to pain signals.
“How Does Paraneoplastic Syndrome Signal Cancer?”
There are two main types: Type I, which does not involve nerve damage, and Type II, characterized by identifiable nerve injuries. Both forms share similar symptoms but may vary in intensity and duration.
Patients with CRPS may experience extreme sensitivity to touch and movement limitations. This disorder not only challenges physical health but also impacts emotional well-being significantly. Understanding CRPS starts with recognizing its complex nature as both a physiological and psychological condition.
Types of CRPS: Type I and Type II
Complex Regional Pain Syndrome (CRPS) is categorized into two distinct types: Type I and Type II.
Type I, often referred to as Reflex Sympathetic Dystrophy (RSD), occurs without any identifiable nerve injury. It typically follows an injury or trauma, leading to a cascade of pain and sensory abnormalities in the affected area. This type is more common and has a broader range of symptoms.
Type II, known as causalgia, arises following a confirmed nerve injury. The pain experienced in this case is associated with specific damage to nerves. Patients may experience heightened sensitivity and other autonomic dysfunctions linked directly to the injured nerves.
“What Causes Patent Ductus Arteriosus Syndrome in Newborns?”
Both types share similarities but can vary significantly in their presentation and underlying causes. Understanding these nuances aids in accurate diagnosis and effective treatment strategies for those suffering from CRPS.
Incidence and Prevalence of CRPS
Complex Regional Pain Syndrome (CRPS) is a rare but significant condition. Its incidence varies, with estimates suggesting it affects 5 to 26 individuals per 100,000 people annually.
The prevalence of CRPS is notably higher in women than men, particularly those aged between 40 and 60 years. However, it can manifest at any age and often follows an injury or trauma.
“Why Does Pearson Syndrome Affect Blood Cells?”
Research indicates that up to 1% of patients with limb injuries may develop CRPS. This suggests that while the condition remains relatively uncommon, awareness among healthcare professionals is crucial for early diagnosis and treatment.
Geographic location also plays a role in prevalence rates. Certain regions report higher occurrences due to environmental factors or population characteristics. Understanding these dynamics helps researchers better address this perplexing disorder.
Potential Causes and Triggering Events
Complex Regional Pain Syndrome (CRPS) can arise following an injury or trauma, but the origins are not always clear. It often develops after fractures, sprains, or surgeries. However, some cases emerge without any identifiable event.
The body’s response to injury plays a pivotal role in CRPS development. An exaggerated inflammatory reaction may trigger persistent pain signals that don’t subside as expected. This abnormal response can lead to nerve damage and altered pain processing pathways.
“How Does Prader-Willi Syndrome Impact Growth?”
Psychological factors also contribute significantly. Stressful life events or emotional distress might act as catalysts for onset or exacerbation of symptoms.
Additionally, genetic predispositions may influence susceptibility to CRPS. Certain individuals might have inherited traits that make them more prone to develop this condition following even minor injuries. Understanding these potential causes is essential for effective management and intervention strategies.
Pathophysiology of CRPS
Complex Regional Pain Syndrome (CRPS) involves a complex interplay of neurological, inflammatory, and vascular components. The condition often arises after an injury but can persist long after the initial trauma has healed.
At its core, CRPS is characterized by abnormal responses within the peripheral and central nervous systems. Following an injury, heightened sensitivity occurs due to altered pain signaling pathways. This results in exaggerated pain perception.
“What Are The Signs of Parsonage-Turner Syndrome?”
Inflammation also plays a significant role. Increased levels of pro-inflammatory cytokines contribute to ongoing pain and tissue changes. These inflammatory processes can lead to further nerve damage.
Vascular abnormalities are common in CRPS as well. Patients may experience changes in blood flow regulation that result in temperature fluctuations and color changes in affected limbs.
Together, these mechanisms create a challenging environment for recovery, making effective treatment essential for improving patient outcomes.
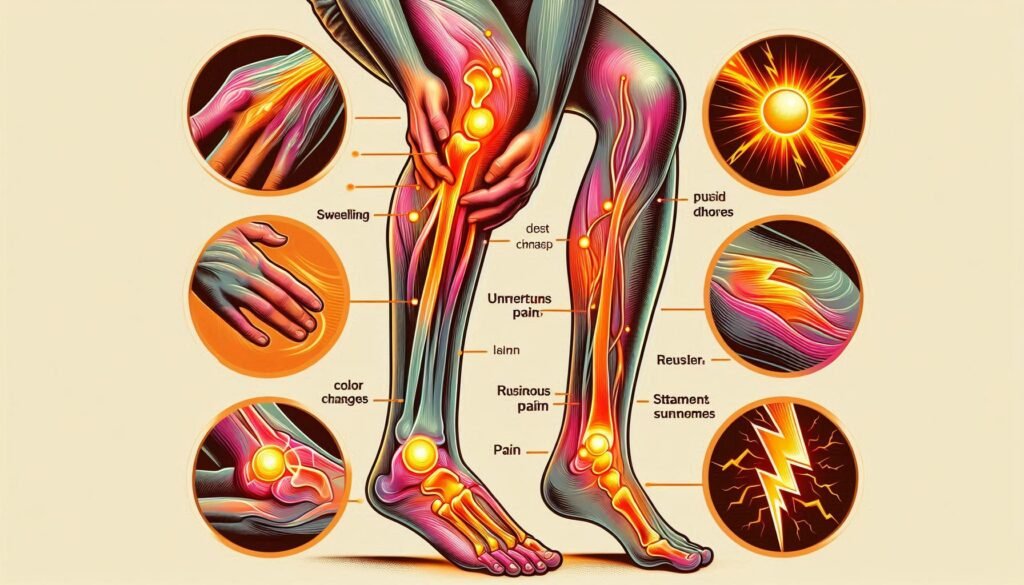
Characteristic Symptoms and Clinical Presentation
Complex Regional Pain Syndrome (CRPS) presents with a diverse range of symptoms, often making it challenging to diagnose. The hallmark is persistent pain that is disproportionate to the initial injury or trauma.
Patients frequently report burning sensations and heightened sensitivity in the affected area. Touching the skin might elicit severe discomfort, known as allodynia. Swelling and changes in skin temperature are common.
“Why Does Patterson-Kelly Syndrome Cause Swallowing Issues?”
Color variations can occur, with affected limbs appearing more red or pale than surrounding areas. Patients may also experience excessive sweating or abnormal nail growth.
Motor function can be impaired, leading to weakness and involuntary movements such as tremors. Additionally, psychological components like anxiety and depression often emerge due to chronic pain experiences.
Recognizing these symptoms early is crucial for effective management of CRPS and improving patient outcomes.
Pain Patterns and Sensory Abnormalities
Individuals with Complex Regional Pain Syndrome (CRPS) often experience distinct pain patterns that can greatly affect their daily lives. The pain is usually described as burning, throbbing, or aching and tends to be disproportionate to the initial injury. It may fluctuate in intensity and can spread beyond the original site of trauma.
Sensory abnormalities are also common in CRPS patients. Many report heightened sensitivity known as allodynia, where even light touch feels painful. Others may experience hyperalgesia, an exaggerated response to stimuli that would typically cause mild discomfort.
These sensory changes contribute to a profound impact on both physical function and emotional well-being. Patients might avoid using affected limbs due to fear of triggering intense pain responses, which can lead to further complications such as muscle atrophy and reduced mobility. Understanding these unique pain experiences is crucial for effective management strategies moving forward.
Autonomic Dysfunction in CRPS
Autonomic dysfunction is a key feature of Complex Regional Pain Syndrome (CRPS). This condition disrupts the normal functioning of the autonomic nervous system. The autonomic nervous system regulates involuntary bodily functions, including heart rate and blood pressure.
Individuals with CRPS often experience changes in skin temperature and color. Affected limbs may feel overly warm or cold to the touch. Sweating abnormalities are also common, leading to either excessive sweating or dryness.
These symptoms can significantly impact daily life. Activities that were once routine may become challenging due to discomfort or altered sensations. Patients might notice swelling in the affected area as well.
Understanding these autonomic changes is crucial for developing effective treatment plans for CRPS patients. Addressing autonomic dysfunction can help improve overall quality of life and enhance recovery prospects for those suffering from this complex pain disorder.
Motor Symptoms and Movement Disorders
Motor symptoms in Complex Regional Pain Syndrome (CRPS) can significantly impact a patient’s quality of life. These motor disturbances often manifest as weakness, tremors, or involuntary movements in the affected limb.
Patients may experience difficulty with coordination and fine motor tasks. This can make everyday activities such as writing, buttoning shirts, or holding objects challenging.
Dystonia is another common feature seen in CRPS patients. It involves abnormal muscle contractions leading to twisting movements or postures that are painful and unsettling.
Additionally, some individuals might exhibit decreased range of motion due to pain-related guarding behaviors. This protective mechanism can further limit mobility and exacerbate feelings of frustration.
Understanding these motor symptoms is crucial for developing effective treatment strategies tailored to each patient’s needs. Rehabilitation approaches focusing on strengthening and improving function play an essential role in managing these movement disorders associated with CRPS.
Psychological Impact and Mental Health Considerations
Complex Regional Pain Syndrome (CRPS) significantly affects mental health. Living with chronic pain can lead to anxiety and depression. The unpredictability of symptoms often creates feelings of helplessness.
Patients may experience isolation as they struggle to engage in daily activities. This social withdrawal can further exacerbate their emotional distress.
Coping with the complexity of CRPS requires not only physical management but also psychological support. Therapeutic approaches, such as cognitive-behavioral therapy, can help patients develop healthier coping mechanisms.
Support groups offer a sense of community for those affected by CRPS. Sharing experiences fosters understanding and reduces feelings of loneliness.
Mental health professionals play a crucial role in addressing these challenges. Comprehensive care involves both pain management and psychological well-being to enhance overall quality of life for individuals suffering from this enigmatic disorder.
Diagnostic Criteria and Assessment Methods
Diagnostic criteria for Complex Regional Pain Syndrome (CRPS) are primarily guided by the Budapest Criteria. This framework emphasizes a combination of clinical signs and symptoms that help healthcare providers identify the condition accurately.
To establish a diagnosis, medical professionals assess patients based on their history, reported pain levels, and physical examination findings. Key indicators include ongoing pain that’s disproportionate to any inciting event or injury.
Assessment methods often involve evaluating sensory changes such as hyperesthesia or allodynia. These sensations can significantly affect a person’s daily life.
Imaging studies like MRI or bone scans may be used to rule out other conditions but are not definitive for CRPS itself. Comprehensive evaluations also take psychological factors into account since mental health can influence how individuals experience and manage their pain.
Imaging Studies and Their Role in Diagnosis
Imaging studies play a crucial role in diagnosing Complex Regional Pain Syndrome (CRPS). While there is no definitive test for CRPS, these imaging techniques can help rule out other conditions and provide insights into the extent of nerve damage.
Magnetic Resonance Imaging (MRI) is commonly used to visualize changes in soft tissues and bones. It helps identify any underlying issues like fractures or tumors that might mimic CRPS symptoms.
Bone scans are another valuable tool. They can detect changes in blood flow and metabolic activity within bone tissue, which may indicate the presence of CRPS.
Ultrasound has gained popularity due to its ability to assess structural abnormalities in nerves and surrounding tissues. This non-invasive method offers real-time images during movement, enhancing diagnostic accuracy.
While imaging alone cannot confirm a CRPS diagnosis, it significantly aids healthcare providers by providing additional context alongside clinical evaluations.
Differential Diagnosis: Similar Pain Conditions
Differential diagnosis is crucial for accurately identifying Complex Regional Pain Syndrome (CRPS). Several similar pain conditions can mimic its symptoms, making it essential to distinguish between them.
One such condition is neuropathic pain, often resulting from nerve injury. Patients may experience burning sensations and heightened sensitivity, akin to CRPS.
Fibromyalgia also presents a challenge. Characterized by widespread pain and fatigue, fibromyalgia shares some sensory abnormalities with CRPS but typically lacks the localized swelling or color changes seen in CRPS cases.
Another notable condition is complex pain syndrome related to post-stroke patients. This can lead to altered sensation and persistent discomfort in affected limbs, resembling CRPS without the specific autonomic features.
Rheumatoid arthritis may present joint pain that could be confused with CRPS manifestations. However, systemic symptoms differentiate these conditions significantly.
Thorough clinical evaluation remains indispensable for accurate identification and appropriate management of these overlapping disorders.
Early Intervention and Treatment Approaches
Early intervention is crucial for managing Complex Regional Pain Syndrome (CRPS). Timely treatment can prevent the progression of symptoms and improve patient outcomes.
One effective approach involves a multidisciplinary strategy, integrating pain management specialists, physical therapists, and psychologists. This collaboration ensures that all aspects of the disorder are addressed comprehensively.
Physical therapy plays a vital role in early intervention. Gentle exercises aimed at restoring movement can help reduce stiffness and improve function. Occupational therapy also focuses on daily activities to enhance quality of life.
Pharmacological treatments may be introduced promptly to manage pain effectively. Medications like anticonvulsants or topical analgesics can provide relief while minimizing side effects.
Prompt psychological support is essential as well. Cognitive-behavioral therapy (CBT) can equip patients with coping strategies to deal with chronic pain challenges, fostering resilience during recovery efforts.
Pharmacological Management of CRPS
Pharmacological management of Complex Regional Pain Syndrome (CRPS) aims to alleviate pain and improve function. Medications often form the cornerstone of treatment strategies.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed for mild to moderate pain relief. These can help reduce inflammation and discomfort associated with CRPS.
Antidepressants, particularly tricyclics like amitriptyline, have shown effectiveness in managing neuropathic pain. They also address any underlying mood disorders that may arise due to chronic pain.
Gabapentinoids, such as gabapentin or pregabalin, target nerve-related pain specifically. These medications can decrease hyperexcitability of neurons involved in CRPS.
For more severe cases, opioids might be necessary but come with risks of dependency. Therefore, they should be used judiciously under medical supervision.
Topical agents like lidocaine patches offer localized relief without systemic side effects. Each patient’s response varies; therefore, individualized pharmacological plans are essential for effective management.
Interventional Pain Management Techniques
Interventional pain management techniques play a critical role in treating Complex Regional Pain Syndrome (CRPS). These methods aim to relieve pain directly at the source, offering patients hope for improved function and quality of life.
One common technique is nerve blocks. By injecting anesthetic near specific nerves, physicians can interrupt pain signals before they reach the brain. This approach often provides immediate relief and helps guide further treatment decisions.
Another option includes spinal cord stimulation. This involves implanting a device that sends electrical impulses to the spinal cord, masking painful sensations from CRPS. Many patients report significant reductions in their discomfort following this procedure.
In some cases, intrathecal drug delivery systems are utilized. These devices deliver medication directly into the cerebrospinal fluid surrounding the spine, allowing for lower doses with fewer side effects than traditional oral medications.
These interventional strategies offer tailored solutions for managing CRPS symptoms effectively.
Physical and Occupational Therapy for CRPS
Physical and occupational therapy play crucial roles in managing Complex Regional Pain Syndrome (CRPS). These therapies aim to improve function, reduce pain, and enhance the quality of life for those affected.
Physical therapy focuses on restoring movement. Targeted exercises help maintain joint mobility and strength. Gradual desensitization techniques can alleviate hypersensitivity associated with CRPS.
Occupational therapy emphasizes daily activities. Therapists work with patients to adapt routines and incorporate assistive devices. This support fosters independence despite physical limitations.
Both therapies promote a holistic approach, addressing not just physical symptoms but also emotional well-being. They encourage patient engagement through education about CRPS and self-management strategies.
Regular sessions are vital in establishing a routine that combats the debilitating effects of CRPS over time. Collaborating closely with healthcare providers ensures that treatment plans remain tailored to individual needs for optimal recovery outcomes.
Psychological Interventions and Coping Strategies
Psychological interventions play a crucial role in managing Complex Regional Pain Syndrome (CRPS). Cognitive Behavioral Therapy (CBT) helps patients reframe their thoughts about pain, reducing anxiety and depression linked to the condition. By shifting focus from pain to coping mechanisms, individuals can regain a sense of control over their lives.
Mindfulness techniques offer another valuable strategy. Practicing mindfulness encourages patients to stay present and accept their sensations without judgment. This approach reduces stress and fosters emotional resilience.
Support groups also provide vital connections for those living with CRPS. Sharing experiences creates an understanding community that diminishes feelings of isolation and helplessness.
Incorporating relaxation techniques such as guided imagery or deep breathing exercises can alleviate tension. These practices enhance overall well-being by promoting a calmer mental state amidst chronic pain challenges.
Emerging Treatments and Clinical Trials
Emerging treatments for Complex Regional Pain Syndrome (CRPS) are gaining attention as researchers explore new avenues to alleviate this complex condition. Recent clinical trials have focused on advanced pharmacological options, including novel analgesics and anti-inflammatory agents that target pain pathways more effectively.
Neuromodulation techniques, such as spinal cord stimulation and transcranial magnetic stimulation, are also being investigated. These methods aim to alter nerve activity and provide relief from chronic pain symptoms associated with CRPS.
Additionally, regenerative medicine approaches like platelet-rich plasma therapy and stem cell treatment show promise. They may help repair nerve damage or modulate inflammatory responses within affected tissues.
Researchers are increasingly emphasizing multidisciplinary strategies in their trials. Combining physical therapy with psychological support can enhance overall outcomes for individuals suffering from CRPS. Continuous advancements in technology and understanding of the disorder pave the way for innovative solutions tailored to individual needs.
Long-term Prognosis and Quality of Life
Long-term prognosis for individuals with Complex Regional Pain Syndrome (CRPS) can be quite variable. Some patients may experience significant improvement over time, while others may face persistent pain and disability. The key factors influencing outcomes include the timing of diagnosis and intervention, as well as individual patient characteristics.
Research suggests that early treatment is associated with better outcomes. Promptly addressing CRPS symptoms often leads to a higher likelihood of achieving relief from pain and restoring function. Patients who engage in a comprehensive management plan that combines medication, physical therapy, psychological support, and interventional techniques tend to report better quality of life.
Quality of life for those living with CRPS can be impacted significantly by the chronic nature of their condition. Chronic pain affects not only physical abilities but also emotional health and daily functioning. Many individuals grapple with feelings of frustration or isolation due to their experiences.
Support networks play an essential role in enhancing quality of life for those affected by CRPS. Connecting with healthcare providers who understand this complex disorder can empower patients on their journey toward recovery. Additionally, engaging in community resources or support groups provides valuable interactions that help alleviate feelings of loneliness.
As research progresses into novel treatments and interventions, there is hope for improving long-term results for people living with Complex Regional Pain Syndrome (CRPS). With proper care tailored to individual needs, many can find ways to manage symptoms effectively while maintaining an active lifestyle.