Introduction to XMEA Syndrome: Defining the Condition
XMEA Syndrome, or X-linked Myopathy with Excessive Autophagy, is a rare genetic disorder that primarily affects muscle function. Despite its intricate name, this condition presents profound challenges for those diagnosed and their families. Understanding XMEA Syndrome is crucial as it sheds light on the interplay between genetics and muscular health.
As researchers delve deeper into its complexities, they uncover fascinating insights about how specific gene mutations lead to excessive autophagy—a process where cells self-digest harmful components. This blog will explore what XMEA Syndrome entails, from its genetic underpinnings to clinical symptoms and treatment options. Join us as we unravel the mysteries of this unique syndrome and equip ourselves with knowledge that could make a difference in patient care and support.

Genetic Underpinnings of XMEA Syndrome
XMEA Syndrome is primarily linked to mutations in the VMA21 gene located on the X chromosome. This gene plays a critical role in muscle function and cellular processes.
When there are alterations or disruptions in the VMA21 gene, it can lead to improper protein folding. This misfolding affects muscle cell integrity and overall performance.
Since XMEA is an X-linked condition, it predominantly impacts males, with females potentially being carriers. The inheritance pattern contributes significantly to its prevalence among affected individuals.
“Why Does CHARGE Syndrome Affect Multiple Body Systems?”
Research continues to explore other genetic factors that may influence disease severity and presentation. Understanding these genetic underpinnings helps researchers develop targeted interventions for those living with this syndrome.
The Role of VMA21 Gene Mutations in XMEA Syndrome
VMA21 gene mutations play a critical role in the development of XMEA Syndrome. This gene is essential for the proper functioning of the endosomal-lysosomal system within cells. When mutations occur, they disrupt normal protein folding and trafficking processes.
The malfunctioning VMA21 leads to abnormal autophagy—a process that cleans out damaged cellular components. In XMEA Syndrome, excessive autophagy exacerbates muscle degeneration and weakness.
“How Does Complex Regional Pain Syndrome Cause Chronic Pain?”
Studies have shown that these genetic variations can result in various clinical presentations among affected individuals. Some may experience more severe symptoms than others due to specific mutation types.
Understanding the impact of VMA21 mutations helps clinicians tailor treatment approaches for patients with XMEA Syndrome, making genetic testing an invaluable tool in managing this complex condition.
Pathophysiology of Excessive Autophagy in XMEA Syndrome
Excessive autophagy plays a pivotal role in the pathophysiology of XMEA Syndrome. Autophagy is a natural cellular process that degrades and recycles damaged organelles, proteins, and other cellular debris. In individuals with XMEA Syndrome, this mechanism becomes dysregulated.
When autophagy runs amok, it can lead to muscle fiber degeneration. This excessive degradation creates an imbalance between protein synthesis and breakdown within muscle cells. Consequently, patients may experience significant muscle wasting over time.
“What Causes Cri du Chat Syndrome? Understanding Cat Cry Disease”
Furthermore, the accumulation of dysfunctional cellular components contributes to inflammation and oxidative stress. These factors exacerbate symptoms like weakness and fatigue. Understanding these processes provides insight into potential therapeutic targets for managing this complex condition effectively.
Research continues to explore how modulating autophagy could restore balance in affected cells, potentially improving outcomes for those living with XMEA Syndrome.
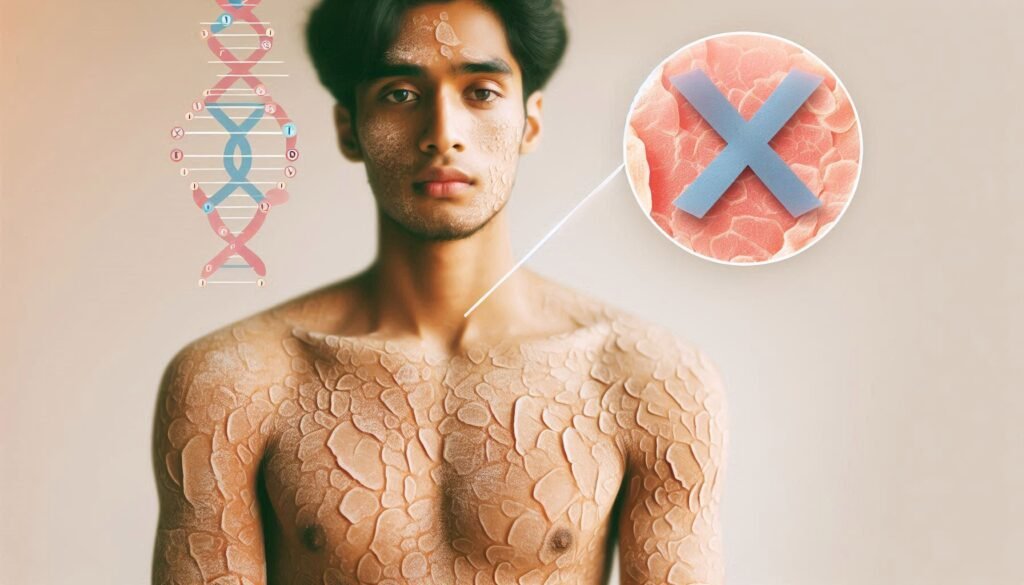
Clinical Presentation and Symptoms of XMEA Syndrome
XMEA Syndrome typically manifests in early childhood. Muscle weakness is a prominent symptom, often becoming noticeable as children struggle with common activities like climbing stairs or running.
Patients may experience progressive muscle atrophy, particularly affecting proximal muscles. This can lead to difficulty lifting arms and legs.
“How Does Dandy-Walker Syndrome Affect Brain Development?”
Fatigue is another frequent complaint, impacting daily life and overall quality of life. Some individuals might also exhibit respiratory issues due to weakened diaphragm muscles.
In addition to physical symptoms, there could be cognitive impacts stemming from associated neurological manifestations. Parents and caregivers should monitor any unusual behaviors or challenges in learning.
Skin abnormalities are not uncommon either; dermatological signs can sometimes accompany the muscular symptoms of XMEA Syndrome, making diagnosis more intricate. Recognizing these varied presentations early on is crucial for effective management and care planning.
Muscle Weakness Patterns in XMEA Syndrome
Muscle weakness in XMEA Syndrome presents with distinct patterns that can help clinicians identify the condition. Typically, it affects proximal muscles more than distal ones. This means individuals may struggle with actions like lifting their arms or climbing stairs.
Patients often experience muscle fatigue after minimal exertion. This fatigue is not just a result of physical activity; it can also occur during routine daily tasks.
“What Causes De Quervain Syndrome? Wrist Pain Guide”
Another notable feature is the asymmetrical nature of weakness in some cases. One side of the body might show more pronounced symptoms compared to the other, adding complexity to diagnosis and management.
In addition to these patterns, patients may exhibit myalgia or discomfort alongside muscle weakness. These symptoms contribute to an overall decline in mobility and quality of life for those affected by XMEA Syndrome, emphasizing the need for tailored therapeutic approaches.
Diagnostic Criteria and Approaches for XMEA Syndrome
Diagnosing XMEA Syndrome involves a comprehensive assessment strategy. Clinicians typically begin with a detailed medical history and physical examination to evaluate muscle strength and functionality.
Blood tests are crucial for measuring creatine kinase (CK) levels, often elevated in myopathies. Genetic testing then plays a pivotal role, specifically looking for mutations in the VMA21 gene associated with this syndrome.
“Why Does Delayed Sleep Phase Syndrome Disrupt Sleep Patterns?”
MRI imaging can reveal muscle atrophy or inflammation patterns that aid diagnosis. Muscle biopsies may also be conducted to assess morphological changes indicative of excessive autophagy.
A multidisciplinary approach is essential, involving neurologists, geneticists, and physiotherapists. This collaboration ensures accurate diagnosis and tailored management plans for affected individuals, paving the way for effective intervention strategies.
Muscle Biopsy Findings in XMEA Syndrome
Muscle biopsy is a crucial diagnostic tool in evaluating XMEA Syndrome. The histopathological analysis often reveals distinct features that aid in confirming the diagnosis.
Typically, biopsies show myofibrillar degeneration and loss of muscle fibers. This can be accompanied by increased connective tissue, which indicates chronic muscle injury.
One notable finding is the presence of autophagic vacuoles within muscle fibers. These structures are indicative of excessive autophagy, characteristic of XMEA Syndrome.
Additionally, immunohistochemical staining may reveal abnormal protein accumulation due to impaired degradation processes. Such findings help differentiate this condition from other myopathies.
Understanding these biopsy results plays a vital role in guiding treatment strategies and patient management for those affected by XMEA Syndrome.
Genetic Testing and Counseling for XMEA Syndrome
Genetic testing plays a crucial role in diagnosing XMEA Syndrome. Identifying mutations in the VMA21 gene helps confirm the condition. This process involves analyzing a blood sample to look for specific genetic alterations associated with excessive autophagy.
Counseling is equally important for families affected by this syndrome. Genetic counselors provide valuable information about inheritance patterns, risks of recurrence, and implications for family members. They help individuals understand what the results mean and guide them through difficult decisions.
Additionally, counseling can assist in emotional support during diagnosis and management of XMEA Syndrome. Families often face uncertainty, making it essential to address their concerns and questions comprehensively.
Access to resources that educate patients about living with XMEA Syndrome can empower families as they navigate treatment options and coping strategies together.
Differential Diagnosis: XMEA vs. Other Myopathies
Differential diagnosis is crucial when evaluating XMEA Syndrome. Clinicians must distinguish it from other myopathies that present similar symptoms.
One common condition to consider is Duchenne Muscular Dystrophy (DMD). While both disorders lead to muscle weakness, DMD primarily affects boys and has a different genetic basis.
Another potential differential is Facioscapulohumeral Muscular Dystrophy (FSHD). FSHD typically involves facial and shoulder girdle muscle weakness, unlike the broader muscular involvement seen in XMEA.
Myotonic dystrophy presents with delayed relaxation of muscles. Symptoms can overlap with those of XMEA, complicating accurate diagnosis.
Polymyositis should also be assessed. It features inflammatory muscle damage but may have distinct lab findings and response to treatment compared to XMEA Syndrome.
Careful evaluation through clinical presentation and diagnostic tests helps differentiate these conditions effectively.
Treatment Strategies for XMEA Syndrome
Treatment strategies for XMEA Syndrome focus on alleviating symptoms and improving quality of life. Each patient’s needs may vary, so personalized approaches are essential.
Physical therapy plays a crucial role in enhancing muscle strength and function. Tailored exercise programs can help maintain mobility while reducing the risk of contractures.
Nutritional support is another vital component. A balanced diet rich in proteins, vitamins, and minerals aids muscle health and overall well-being.
In some cases, medications may be prescribed to manage associated symptoms such as pain or inflammation. These pharmacological interventions should always be closely monitored by healthcare professionals.
Managing respiratory complications is equally important. Regular assessments can identify issues early, allowing timely interventions that improve respiratory function.
Additionally, psychosocial support helps address emotional challenges faced by patients and their families. Connecting with support groups fosters resilience and shared experiences among individuals battling this condition.
Physical Therapy and Rehabilitation in XMEA Syndrome
Physical therapy plays a crucial role in the management of XMEA Syndrome. It focuses on improving muscle strength and function, which can be significantly impacted by this condition. Tailored exercise programs help patients maintain mobility and prevent further deterioration.
Rehabilitation strategies often include resistance training and aerobic exercises. These activities are designed to enhance endurance while minimizing fatigue. A skilled therapist assesses individual needs, ensuring that each program is appropriate for the patient’s capabilities.
Therapists also emphasize flexibility and range-of-motion exercises. Such activities can alleviate stiffness in affected muscles, promoting better overall movement patterns.
Education about energy conservation techniques is essential as well. Patients learn how to manage their daily tasks without overexerting themselves, thus optimizing their quality of life.
Furthermore, consistent follow-ups with healthcare providers allow for adjustments based on progress or changes in symptoms, facilitating ongoing support through rehabilitation efforts.
Nutritional Considerations for Patients with XMEA Syndrome
Nutritional considerations play a vital role in managing XMEA Syndrome. Patients often experience muscle weakness, which can impact their ability to maintain a balanced diet. Ensuring adequate nutrition is crucial for supporting muscle function and overall health.
A high-protein diet may be beneficial, as it aids muscle repair and growth. Including lean meats, fish, dairy products, legumes, and nuts can help meet protein requirements.
Additionally, incorporating antioxidants through fruits and vegetables supports cellular health. Foods rich in omega-3 fatty acids are essential too; they may reduce inflammation and promote recovery.
Hydration cannot be overlooked either. Proper fluid intake helps maintain energy levels and improves physical performance during therapy sessions.
Consulting with a registered dietitian familiar with XMEA Syndrome can provide personalized dietary strategies tailored to individual needs. This approach enhances treatment outcomes while empowering patients on their journey toward better health.
Managing Respiratory Complications in XMEA Syndrome
Respiratory complications are a significant concern for individuals with XMEA Syndrome. The muscle weakness associated with this condition can affect the diaphragm and other muscles involved in breathing. As a result, patients may experience difficulties in respiratory function.
Regular monitoring of lung capacity and oxygen levels is essential. Pulmonary function tests can help track any decline over time. Early intervention is crucial to prevent severe complications.
Patients may benefit from respiratory therapies such as incentive spirometry or positive pressure ventilation techniques. These methods can support effective breathing patterns and enhance lung expansion.
For those experiencing persistent issues, home health care providers can assist with daily management strategies. Educating family members about recognizing signs of respiratory distress can also be beneficial.
Collaboration between healthcare professionals, including pulmonologists and physical therapists, ensures a comprehensive approach to managing these challenges effectively.
Psychosocial Aspects of Living with XMEA Syndrome
Living with XMEA Syndrome can be a challenging journey. Patients often face not only physical limitations but also emotional and social hurdles. The unpredictability of symptoms can lead to anxiety and frustration.
Support networks play a crucial role in managing these psychosocial aspects. Family, friends, and support groups provide essential emotional backing. Connecting with others who share similar experiences fosters understanding and reduces feelings of isolation.
Education is vital for patients and their families. Understanding the condition helps in coping with its complexities. Knowledge empowers individuals to advocate for themselves within healthcare systems.
Mental health resources are equally important. Therapy sessions can equip patients with strategies to handle stressors associated with chronic illness. This holistic approach ensures that both physical health and mental well-being are prioritized in treatment plans.
Maintaining open communication about fears or concerns helps strengthen relationships, creating a supportive environment conducive to healing and adaptation.
Prognosis and Disease Progression in XMEA Syndrome
The prognosis for individuals with XMEA Syndrome can vary significantly based on several factors. The severity of symptoms and the age at which they present often influence disease progression.
Many patients experience muscle weakness that gradually worsens over time, impacting mobility and daily activities. Regular assessments are crucial to monitor changes in muscle function and overall health.
Some individuals may retain a degree of independence for years, while others might face increased challenges earlier in life. Respiratory complications can arise as the condition progresses, necessitating careful management.
Research into genetic variants provides insight into potential outcomes, but predicting individual trajectories remains complex. Continuous advancements in understanding this syndrome hold promise for more tailored approaches to care and support for those affected.
Research Advances in Understanding XMEA Syndrome
Recent research has made significant strides in understanding XMEA Syndrome. Scientists are delving deeper into the genetic causes and implications of this complex condition. Advanced genomic techniques have identified specific mutations within the VMA21 gene, highlighting their role in disease manifestation.
Studies using animal models have illuminated how excessive autophagy contributes to muscle degeneration associated with XMEA Syndrome. This knowledge opens doors for targeted interventions aimed at regulating cellular processes implicated in muscle health.
Moreover, ongoing clinical trials are evaluating potential therapies that could modify disease progression. Researchers are also exploring biomarkers for earlier diagnosis and better monitoring of treatment efficacy.
Collaborative efforts across global research institutions aim to share findings and accelerate discoveries in this rare myopathy area. As a result, patients may soon benefit from more personalized care strategies tailored to their unique genetic profiles.
Emerging Therapies and Clinical Trials for XMEA Syndrome
As research continues, the landscape of treatment for XMEA Syndrome is slowly evolving. Various clinical trials are underway to explore new therapies aimed at addressing the genetic and physiological challenges posed by this condition. Researchers are investigating innovative approaches that could potentially modify disease progression or improve muscle function.
Gene therapy is one promising area of investigation. By targeting the specific mutations in the VMA21 gene, scientists hope to restore normal protein function and mitigate excessive autophagy. Additionally, pharmacological interventions focusing on modulating autophagic processes may offer another pathway for therapeutic development.
Participation in clinical trials can provide patients access to cutting-edge treatments not yet available through standard care—potentially leading to significant improvements in quality of life. It also contributes valuable data that helps enhance our understanding of XMEA Syndrome over time.
For families affected by this syndrome, staying informed about ongoing research is crucial. Engaging with support networks and medical professionals who specialize in neuromuscular diseases can facilitate access to resources and information regarding emerging therapies.
Continued advocacy for funding and awareness around conditions like XMEA Syndrome will play a vital role in propelling future discoveries forward, paving the way towards better treatment options for those impacted by this complex disorder.