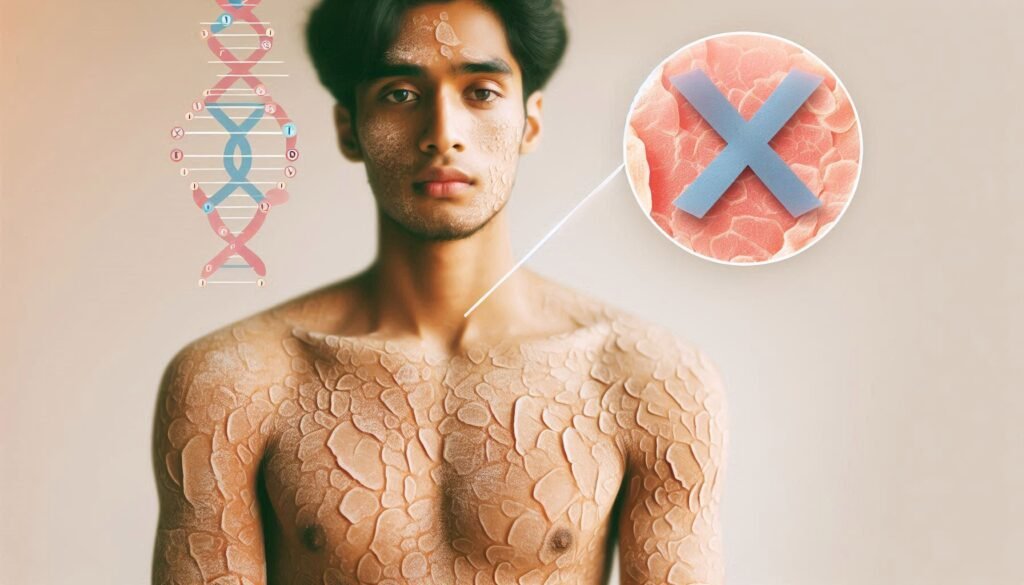
X-linked Ichthyosis is a rare genetic skin disorder that affects many individuals worldwide. Characterized by dry, scaly skin and often misunderstood, this condition can significantly impact daily life. Many people are unaware of its underlying causes, unique symptoms and effective management strategies.
In this blog post, we will explore the various facets of X-linked Ichthyosis—from its genetic roots to practical treatment options—aiming to shed light on an often-overlooked condition that deserves more attention. Whether you’re seeking information for yourself or a loved one, understanding X-linked Ichthyosis is the first step toward better management and quality of life. Let’s dive deeper into this intriguing topic together!
Understanding X-linked Ichthyosis: An Overview of the Genetic Skin Disorder
X-linked Ichthyosis is a genetic skin disorder primarily affecting males. It arises from mutations in the STS gene, which plays a crucial role in breaking down steroid sulfate compounds. The deficiency of this enzyme leads to an accumulation of substances that disrupt normal skin function.
“What Causes Alport Syndrome? Understanding Hereditary Kidney Disease”
Individuals with this condition often present with thickened, dry patches on their skin, commonly found on the elbows and knees. These symptoms can vary widely in severity among affected individuals.
The onset usually occurs at birth or shortly thereafter, making early diagnosis essential for effective management. While predominantly seen in males due to its X-linked inheritance pattern, female carriers may also experience milder manifestations.
Awareness of X-linked Ichthyosis is vital not only for those diagnosed but also for families considering genetic counseling and testing options. Understanding this condition fosters better support systems for patients navigating daily challenges associated with their unique skin needs.
Genetic Basis of X-linked Ichthyosis: The STS Gene and Steroid Sulfatase Deficiency
X-linked ichthyosis is primarily caused by a mutation in the STS gene. This gene encodes the enzyme steroid sulfatase, which plays a crucial role in metabolizing cholesterol sulfate.
“Allan-Herndon-Dudley Syndrome: How Does It Impact Brain Development?”
When there’s a deficiency of steroid sulfatase due to mutations in the STS gene, it leads to an accumulation of cholesterol sulfate on the skin’s surface. This buildup disrupts normal skin barrier function and results in severe dryness and scaling typically seen with this condition.
The disorder follows an X-linked recessive inheritance pattern, meaning that males are more significantly affected while females may be carriers without showing symptoms. Understanding this genetic basis helps healthcare providers offer better diagnostic and management strategies for those impacted by X-linked ichthyosis.
Early identification can lead to appropriate interventions tailored to individual needs, improving quality of life for patients living with this genetic skin disorder.
Inheritance Patterns and Carrier Status in X-linked Ichthyosis
X-linked Ichthyosis follows an X-linked recessive inheritance pattern. This means the disorder is primarily expressed in males, who have only one X chromosome. If that X chromosome carries the mutated STS gene, normal steroid sulfatase production is disrupted, leading to skin symptoms.
“What Are The Early Signs of AIDS? Understanding HIV Progression”
Females can also be carriers of this condition. They possess two X chromosomes and generally do not exhibit severe symptoms due to a second healthy copy of the gene. However, carrier females may experience milder manifestations or none at all.
Carrier status in women can be determined through genetic testing. Identifying a carrier allows for better family planning and informed decisions regarding potential offspring’s health risks. Understanding these patterns sheds light on how genetics play a crucial role in managing and anticipating issues related to this skin disorder.
Clinical Presentation: Characteristic Skin Manifestations
X-linked Ichthyosis prominently features unique skin manifestations that are crucial for diagnosis. Patients typically exhibit dry, scaly skin with a characteristic thickening known as hyperkeratosis.
These scales often appear on the extensor surfaces of limbs, such as elbows and knees. Additionally, they may be more pronounced on the trunk and neck areas. The texture can vary from fine to coarse, resembling fish scales in appearance.
“How Does Babinski-Nageotte Syndrome Affect The Brainstem?”
Infants may present with red or inflamed patches at birth, which later evolve into the classic scaling pattern. Unlike other dermatological conditions, X-linked Ichthyosis is usually asymptomatic regarding itching or pain.
Over time, some individuals develop darker pigmentation in affected areas due to chronic irritation or sun exposure. Understanding these clinical presentations aids healthcare providers in identifying this genetic disorder early and initiating appropriate management strategies promptly.
Extracutaneous Manifestations of X-linked Ichthyosis
X-linked Ichthyosis primarily affects the skin, but it can also present with various extracutaneous manifestations. These include ocular issues and potential neurological impacts that may not be immediately associated with the condition.
One notable ocular complication is corneal opacities. This occurs due to a buildup of cholesterol in the eye, affecting vision over time. Regular ophthalmological check-ups are essential for early detection and management of these changes.
“What Causes Baller-Gerold Syndrome? Guide to Rare Cranial Disorder”
Neurologically, some individuals might experience learning difficulties or developmental delays, particularly if they have more severe forms of the disorder. While this aspect varies widely among patients, supportive educational strategies can greatly enhance their quality of life.
Additionally, there may be endocrine implications related to steroid sulfatase deficiency. Hormonal imbalances could necessitate monitoring by healthcare professionals familiar with X-linked Ichthyosis and its broader effects on health beyond just skin symptoms.
Diagnostic Approaches: Clinical, Biochemical, and Genetic Testing
When diagnosing X-linked Ichthyosis, a combination of clinical evaluation, biochemical analysis, and genetic testing is essential. Physicians begin with a thorough physical examination to identify the characteristic skin manifestations associated with this disorder.
Biochemical tests are crucial for assessing steroid sulfatase activity in the patient’s blood or skin samples. A significant reduction in enzyme levels can indicate steroid sulfatase deficiency.
Genetic testing provides definitive confirmation of X-linked Ichthyosis. This involves analyzing DNA for mutations in the STS gene, which directly causes this condition. Such testing not only confirms diagnosis but also helps determine carrier status among family members.
Together, these diagnostic approaches ensure accurate identification and pave the way for tailored management strategies that address individual patient needs effectively.
Prenatal Diagnosis and Genetic Counseling for X-linked Ichthyosis
Prenatal diagnosis plays a crucial role for families at risk of X-linked Ichthyosis. Through advanced techniques such as amniocentesis or chorionic villus sampling, healthcare providers can analyze the fetal DNA for mutations in the STS gene.
Genetic counseling is essential in this context. It provides parents with valuable insights about inheritance patterns and potential outcomes. A genetic counselor helps families understand their risks and options, including whether to proceed with testing.
These discussions often explore emotional aspects too. Parents may experience anxiety regarding possible diagnoses. Counselors guide them through these feelings, ensuring they feel supported throughout the process.
Identifying carrier status among family members also aids in decision-making. This information enables informed choices about future pregnancies and necessary monitoring strategies after birth if an infant is diagnosed with X-linked Ichthyosis.
Differential Diagnosis: Distinguishing X-linked Ichthyosis from Other Ichthyoses
Differentiating X-linked Ichthyosis from other forms of ichthyosis is crucial for appropriate management. Clinicians often rely on clinical features and family history to make an accurate diagnosis.
X-linked Ichthyosis typically presents with dry, scaly skin that resembles a “fish scale” appearance. However, conditions like lamellar ichthyosis feature more generalized scaling and may include thicker plaques.
A key distinguishing factor is the absence of ectropion or palmar/plantar involvement in X-linked Ichthyosis, which can be present in other types such as harlequin ichthyosis.
Biochemical testing plays a vital role too. Deficiency of steroid sulfatase confirms X-linked Ichthyosis while enzyme activity levels differ in other ichthyoses like congenital ichthyosiform erythroderma.
Genetic analysis further aids differentiation by revealing mutations specific to each condition, ensuring patients receive tailored care based on their unique needs.
Topical Treatments for Managing Skin Symptoms
Topical treatments play a crucial role in managing the skin symptoms associated with X-linked Ichthyosis. These therapies aim to hydrate and exfoliate the skin, alleviating dryness and scaling.
Emollients are often the first line of defense. They help lock in moisture and create a protective barrier on the skin’s surface. Regular application is essential for maintaining hydration levels.
Keratinolytic agents like urea or lactic acid can aid in reducing thickened patches. These ingredients work by breaking down excess keratin, allowing for smoother skin texture.
Corticosteroids may also be used judiciously to address inflammation or irritation during flare-ups. However, it’s vital to follow medical guidance when using these medications to avoid potential side effects.
Incorporating gentle cleansers into daily routines can prevent further irritation while supporting overall skin health. Each patient’s regimen should be tailored based on individual needs and sensitivities.
Systemic Therapies in X-linked Ichthyosis Management
Systemic therapies for X-linked ichthyosis aim to address the underlying biochemical imbalances rather than just alleviating skin symptoms. One approach involves the use of retinoids, which are derivatives of vitamin A. These compounds can enhance skin cell turnover and help normalize skin texture.
In some cases, hormone therapy may be considered due to potential hormonal influences on skin health. Estrogen or other hormonal treatments might provide relief from certain manifestations of the disorder.
Patients often benefit from immunomodulatory agents as well. These medications can manage inflammation associated with severe forms of ichthyosis, improving overall comfort and appearance.
Close monitoring is essential while using systemic therapies since they can have side effects. Regular follow-ups with dermatologists ensure optimal management strategies tailored to individual needs and responses to treatment.
Lifestyle Modifications and Skincare Routines for Patients
Lifestyle modifications play a crucial role in managing X-linked Ichthyosis. Patients should focus on keeping their skin well-hydrated and protected. Daily moisturizing is essential to combat dryness. Use thick creams or ointments, especially after bathing.
Bathing practices also make a difference. Opt for lukewarm water rather than hot, as it can strip the skin of natural oils. Limit bath time to avoid excessive drying.
Wearing breathable fabrics helps reduce irritation caused by friction. Cotton clothing is often preferable over synthetic materials that can trap heat and moisture.
Dietary choices can influence skin health too. A balanced diet rich in omega-3 fatty acids may promote better hydration from within.
Staying hydrated by drinking plenty of water supports overall skin condition as well. Regular visits to dermatologists ensure that patients receive tailored skincare advice specific to their needs and challenges associated with X-linked Ichthyosis.
Ocular Complications and Ophthalmological Care
Ocular complications can arise in individuals with X-linked Ichthyosis, primarily due to the skin barrier’s impact on eye health. Patients often experience dry eyes or conjunctivitis, leading to discomfort and potential vision issues.
Regular ophthalmological care is essential for early detection of these problems. Eye specialists may recommend artificial tears or lubricating ointments to alleviate dryness and irritation.
Additionally, patients should be monitored for any signs of keratitis or other corneal abnormalities. Addressing these concerns promptly can help prevent long-term damage.
Education about proper eyelid hygiene can also play a crucial role in maintaining ocular health. Keeping eyelids clean reduces inflammation and irritation around the eyes.
Incorporating regular check-ups into healthcare routines ensures that any emerging ocular issues are managed effectively, promoting better overall well-being for those living with X-linked Ichthyosis.
Neurological Aspects of X-linked Ichthyosis
X-linked Ichthyosis primarily affects the skin, but its impact can extend to neurological aspects. Although not as commonly discussed, there are reports of subtle neurodevelopmental challenges associated with this genetic disorder.
Some individuals may experience learning disabilities or mild developmental delays. These issues can manifest in various ways, such as difficulties in attention or social interactions.
Research suggests that these neurological implications might stem from underlying metabolic disturbances related to steroid sulfatase deficiency. This deficiency influences certain hormonal pathways that could affect brain development and function.
Regular assessments by healthcare professionals familiar with X-linked Ichthyosis are crucial for early detection of any neurodevelopmental concerns. Tailored educational strategies and supportive therapies can significantly enhance the quality of life for affected individuals, ensuring they receive appropriate resources as needed.
Endocrine Considerations in X-linked Ichthyosis
X-linked Ichthyosis can have several endocrine implications that are important for patients and healthcare providers to recognize. One of the key concerns is a potential association with steroid hormone imbalances due to the deficiency in steroid sulfatase.
This enzyme plays a critical role in metabolizing various steroids, which can lead to altered levels of hormones such as testosterone and estradiol. These changes may result in varying degrees of pubertal development issues or fertility concerns later in life.
Additionally, some studies suggest a possible link between X-linked Ichthyosis and thyroid dysfunction. Monitoring thyroid function tests could be beneficial for early detection of any abnormalities.
Patients should also consider regular follow-ups with an endocrinologist familiar with the disorder. This proactive approach ensures timely management of any emerging endocrine issues related to their condition.
Psychosocial Impact and Quality of Life Issues
Living with X-linked Ichthyosis can significantly affect an individual’s psychosocial well-being. The visible skin symptoms often lead to feelings of self-consciousness and social isolation. Many patients may struggle with body image issues, impacting their confidence and interactions.
Families also navigate complex emotional landscapes. Parents may experience anxiety about their child’s future and health outcomes, while siblings might feel overlooked or burdened by caregiving responsibilities.
Support networks play a crucial role in managing these challenges. Connecting with others facing similar experiences fosters understanding and provides valuable resources. Counseling services can help individuals express feelings and cope with societal pressures.
Quality of life concerns extend beyond physical symptoms, affecting mental health as well. Ensuring access to therapy or support groups is essential for holistic care, promoting resilience amidst the struggles associated with this genetic condition.
Management of X-linked Ichthyosis in Infants and Children
Managing X-linked Ichthyosis in infants and children requires a tailored approach to address their unique needs. Early intervention is key, as it can significantly improve skin health and overall comfort.
Gentle cleansing routines are essential. Use mild, fragrance-free cleansers that do not strip the skin of its natural oils. Following bath time, apply thick emollients or moisturizers while the skin is still damp to lock in moisture.
Regular monitoring by healthcare providers helps assess the progression of symptoms and adjust treatment plans accordingly. Dermatologists may recommend specific topical therapies to reduce scaling and alleviate itchiness.
Parents should also be educated about potential complications associated with X-linked Ichthyosis. This knowledge enables proactive management of any issues that arise, ensuring better outcomes for their child’s quality of life. Engaging support groups can provide valuable insights and emotional support throughout this journey.
Transitioning to Adult Care: Long-term Management Strategies
Transitioning from pediatric to adult care for individuals with X-linked Ichthyosis is crucial. As patients grow, their healthcare needs evolve. Establishing a comprehensive management plan tailored to adulthood can enhance quality of life.
Finding a dermatologist experienced in adult ichthyoses is essential. This specialist will understand the unique challenges that arise as skin conditions change over time. Regular follow-ups ensure timely adjustments in treatment strategies.
Education plays a significant role during this transition. Patients should be encouraged to take an active role in managing their condition, including understanding potential complications and proper skincare routines.
Support networks also become increasingly important. Connecting with support groups can provide emotional assistance and shared experiences among adults living with X-linked Ichthyosis.
Addressing any emerging health concerns related to neurological or endocrine functions should not be overlooked, as these aspects may require specific attention during adulthood.
Emerging Therapies and Research Directions in X-linked Ichthyosis
Emerging therapies and ongoing research are paving the way for enhanced management of X-linked Ichthyosis. Scientists are exploring innovative gene therapy techniques aimed at correcting the underlying genetic defect caused by steroid sulfatase deficiency. These groundbreaking approaches hold promise for long-term solutions that could significantly improve skin health and overall quality of life.
Additionally, advancements in topical formulations are being studied to provide better hydration and barrier protection for affected individuals. Researchers are also investigating new systemic treatments that target broader aspects of the disorder, including its extracutaneous manifestations.
As our understanding of X-linked Ichthyosis deepens, collaboration between dermatologists, geneticists, and researchers will be crucial. This multidisciplinary effort aims to not only improve existing treatment protocols but also develop novel therapies tailored to individual patient needs.
Keeping abreast with these developments is vital for patients and families coping with this condition. Engaging with clinical trials or specialized centers can offer access to cutting-edge treatments before they become widely available. The future looks promising as hope continues to grow alongside scientific progress in managing X-linked Ichthyosis effectively.


