What is Schwartz-Jampel Syndrome? An In-depth Introduction
Schwartz-Jampel Syndrome (SJS) is a rare genetic condition that often flies under the radar. Despite its uncommon nature, it poses significant challenges for those affected and their families. Characterized by muscle stiffness and skeletal abnormalities, SJS can lead to a complicated life journey filled with both physical hurdles and emotional resilience. Understanding this syndrome is crucial for improving quality of life and promoting awareness.
As we delve into the complexities of Schwartz-Jampel Syndrome, we’ll explore its genetic underpinnings, clinical features, diagnostic criteria, treatment options, and much more. Whether you’re a medical professional seeking knowledge or someone personally impacted by SJS, this comprehensive guide aims to illuminate the many facets of this unique disorder. Join us as we unravel the mysteries surrounding Schwartz-Jampel Syndrome!
Genetic Foundations: Understanding the HSPG2 Gene Mutations
Schwartz-Jampel Syndrome is primarily linked to mutations in the HSPG2 gene. This gene encodes a protein called perlecan, which plays a crucial role in maintaining the structure and function of connective tissues.
Mutations can disrupt normal muscle and skeletal development. They lead to characteristic symptoms such as myotonia and skeletal abnormalities. The severity of these mutations varies, influencing how each individual experiences the condition.
“How Does VATER Syndrome Affect Multiple Systems?”
Understanding these genetic foundations helps researchers identify potential therapeutic approaches. By studying HSPG2 gene variants, scientists gain insights into targeting treatment strategies effectively.
Genetic testing for HSPG2 mutations can provide clarity for families facing this rare condition. Knowing the underlying cause aids in prognosis and management planning for affected individuals throughout their lives.
Types of Schwartz-Jampel Syndrome: Neonatal and Classical Forms
Schwartz-Jampel Syndrome manifests primarily in two forms: neonatal and classical. Each type presents distinct features that can significantly influence diagnosis and management.
The neonatal form is characterized by severe muscle stiffness from birth. Affected infants may show myotonic contractions, which impede their ability to move freely. Early intervention is crucial for managing symptoms effectively.
“What Are The Signs of Waardenburg Syndrome?”
In contrast, the classical form typically emerges later in childhood or adolescence. Symptoms are less severe but still include muscular rigidity and facial abnormalities. Individuals often experience a gradual progression of motor difficulties over time.
Recognizing these variations is essential for accurate diagnosis and tailored treatment plans. Understanding the differences helps healthcare providers offer the best possible care for individuals with Schwartz-Jampel Syndrome, regardless of when symptoms appear.
Epidemiology of Schwartz-Jampel Syndrome: Prevalence and Risk Factors
Schwartz-Jampel Syndrome (SJS) is an extremely rare genetic disorder. Its prevalence is estimated to be less than 1 in a million births worldwide, making it challenging to gather comprehensive epidemiological data.
The disorder primarily affects individuals of European descent but can occur in any ethnic group. Genetic mutations associated with SJS often arise sporadically rather than through inherited patterns, complicating its study further.
“Why Does Walker-Warburg Syndrome Affect Brain Development?”
Certain risk factors may include family history of the condition and specific genetic backgrounds. However, due to its rarity, identifying definitive risk factors remains difficult. Research continues into potential environmental triggers that may contribute to the syndrome’s manifestation alongside genetic predispositions.
Awareness among healthcare providers is crucial for early diagnosis and management of Schwartz-Jampel Syndrome. This ensures patients receive timely support for their unique needs as symptoms present at various stages throughout life.
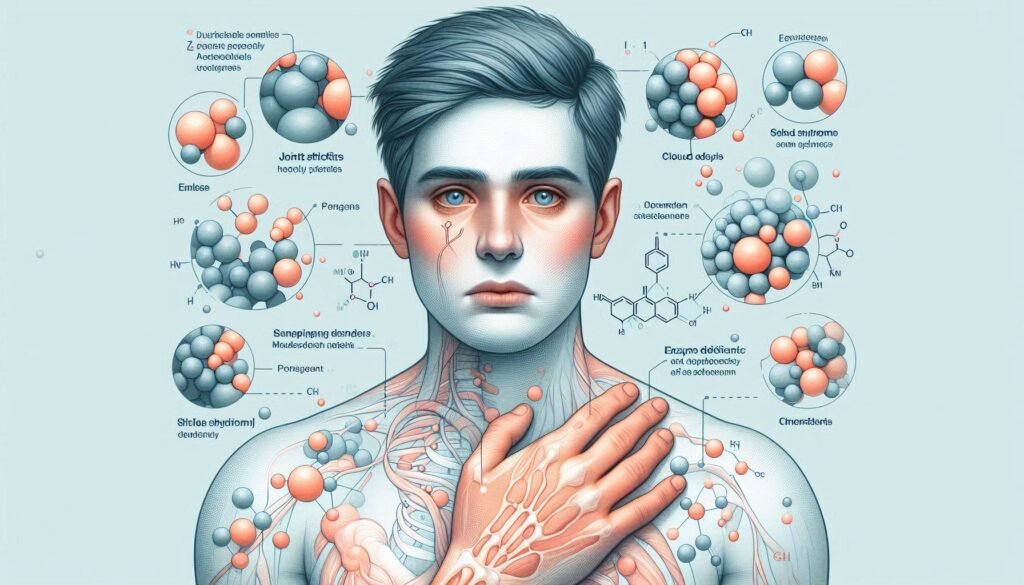
Clinical Features: Identifying the Hallmarks of Schwartz-Jampel Syndrome
Schwartz-Jampel Syndrome presents a range of distinct clinical features that help in its identification. One of the most notable characteristics is myotonia, which causes muscle stiffness and delayed relaxation after contraction. This can significantly impact daily activities.
“How Does Weaver Syndrome Impact Growth?”
Patients may also exhibit skeletal abnormalities such as short stature and deformities in bones, particularly affecting the limbs and spine. These physical manifestations often become apparent during childhood.
Facial features are another hallmark of this syndrome. Individuals frequently display a characteristic appearance with prominent eyes, a flat nasal bridge, and elongated facial structures.
Additionally, affected individuals may experience episodes of muscle spasms or cramps. These symptoms vary from mild to severe and contribute to mobility challenges throughout their lives. Recognizing these clinical signs is crucial for timely diagnosis and management of Schwartz-Jampel Syndrome.
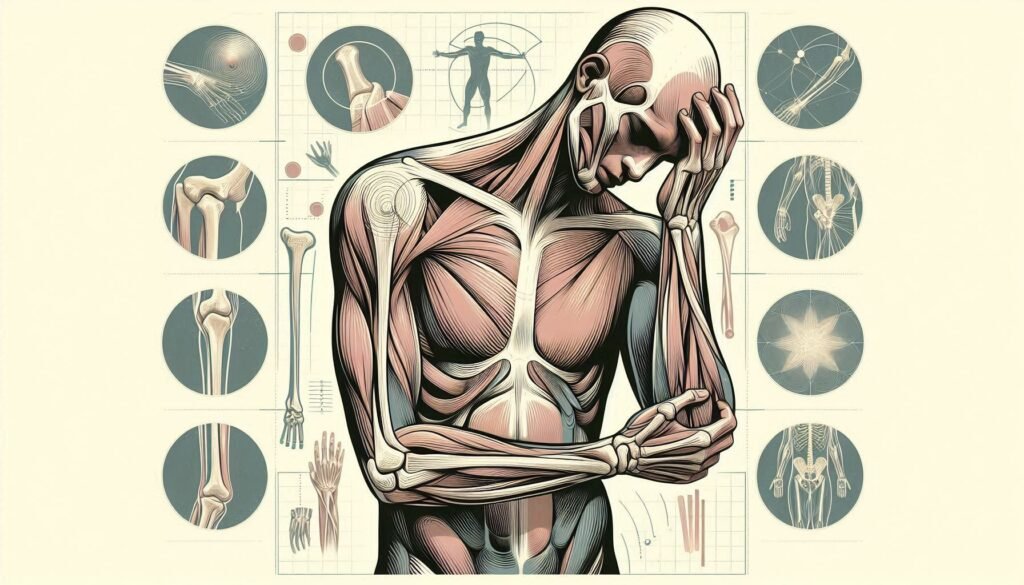
Musculoskeletal Manifestations: Myotonia and Skeletal Abnormalities
Musculoskeletal manifestations are prominent features of Schwartz-Jampel Syndrome. Myotonia, or prolonged muscle contractions, is a common symptom. Patients often experience stiffness and difficulty relaxing their muscles after use. This can lead to challenges in daily activities.
“What Causes Williams Syndrome? Complete Guide”
Skeletal abnormalities also play a crucial role in this condition. Individuals may present with distinctive bone malformations, such as scoliosis or kyphosis. These structural changes can impact mobility and overall function.
Additionally, patients might have disproportionate limb sizes or joint deformities that hinder movement further. The combination of myotonia and skeletal issues creates unique hurdles for those living with Schwartz-Jampel Syndrome.
Understanding these musculoskeletal aspects is vital for effective management and support strategies tailored to each individual’s needs.
Facial Characteristics: Distinctive Features in Schwartz-Jampel Syndrome
Individuals with Schwartz-Jampel Syndrome often present specific facial characteristics that can aid in identification. A prominent feature is the distinctive oval-shaped face, which may appear elongated.
The eyes are typically wide-set and can exhibit a slight droop. This subtle ptosis contributes to the unique appearance of those affected by this condition. Additionally, individuals may have a flat nasal bridge, giving their profile an atypical contour.
“Why Does WAGR Syndrome Affect Multiple Systems?”
Another notable aspect includes thin lips and a small chin, enhancing the overall facial features associated with SJS. Some patients also show signs of dental abnormalities, such as misalignment or delayed tooth eruption.
These facial traits are not merely cosmetic; they often serve as important indicators for clinicians when diagnosing Schwartz-Jampel Syndrome early on in patients’ lives. Recognizing these characteristics can significantly impact treatment approaches and patient care strategies.
Diagnostic Criteria: How Schwartz-Jampel Syndrome is Identified
Diagnosing Schwartz-Jampel Syndrome (SJS) requires a comprehensive approach. Clinicians typically begin with a detailed medical history and physical examination. Observing the distinctive features associated with SJS is crucial for identification.
Key clinical indicators include myotonia, characterized by muscle stiffness, and skeletal abnormalities like scoliosis or joint deformities. Facial characteristics such as prominent forehead and narrow eyes often present early in life.
“How Does Warfarin Embryopathy Syndrome Develop?”
Genetic testing plays an essential role in confirming the diagnosis. Identifying mutations in the HSPG2 gene can provide clarity on whether a patient has SJS.
Furthermore, electromyography (EMG) may be employed to assess electrical activity in muscles, helping differentiate SJS from other neuromuscular disorders. This combination of clinical assessment and advanced diagnostic techniques ensures accurate identification of Schwartz-Jampel Syndrome.
Genetic Testing: The Role of Molecular Diagnosis in SJS
Genetic testing plays a crucial role in diagnosing Schwartz-Jampel Syndrome (SJS). This molecular approach allows for the identification of mutations within the HSPG2 gene, which is responsible for this rare condition.
Through blood samples or saliva tests, clinicians can pinpoint specific genetic alterations. These findings not only confirm a diagnosis but also help differentiate SJS from other neuromuscular disorders.
Patients and families benefit significantly from understanding their genetic background. It aids in assessing risks for future generations and guides personalized treatment plans. Moreover, genetic counseling becomes an integral part of managing expectations and preparing for potential challenges.
As research continues to advance, new insights into genotype-phenotype correlations may emerge. Such developments could enhance early detection methods, paving the way for timely interventions that improve patient outcomes over time.
Electromyography (EMG): A Key Diagnostic Tool for Schwartz-Jampel Syndrome
Electromyography (EMG) plays a crucial role in diagnosing Schwartz-Jampel Syndrome. This technique assesses the electrical activity of muscles, revealing important insights into their function.
During an EMG test, small electrodes are inserted into specific muscles. These electrodes measure the electrical signals generated when muscles contract and relax. For individuals with Schwartz-Jampel Syndrome, abnormal patterns often emerge during testing.
The results help differentiate between myotonia—a key feature of SJS—and other neuromuscular disorders. Identifying these unique muscle responses is essential for accurate diagnosis.
Additionally, EMG can guide treatment strategies by highlighting which muscles may require targeted interventions. Understanding muscle responsiveness can significantly influence rehabilitation approaches for patients living with this rare genetic condition.
Differential Diagnosis: Distinguishing SJS from Similar Conditions
Differential diagnosis is crucial for accurately identifying Schwartz-Jampel Syndrome (SJS). This condition shares symptoms with several neuromuscular disorders, making precise evaluation essential.
Myotonic dystrophy often presents similar muscle stiffness and weakness. However, it typically involves other systemic manifestations that are absent in SJS.
Congenital myopathy may also mimic some features of SJS. While both conditions can exhibit muscular abnormalities, congenital myopathy tends to show a more generalized weakness without the characteristic facial features seen in SJS.
Another condition to consider is arthrogryposis multiplex congenita. Although this disorder leads to joint contractures and skeletal deformities like those found in SJS, it lacks the specific muscle hypertonicity associated with Schwartz-Jampel Syndrome.
Careful clinical assessment combined with genetic testing helps clinicians differentiate these conditions effectively. A comprehensive understanding of patient history further aids in reaching an accurate diagnosis.
Treatment Strategies: Managing Symptoms of Schwartz-Jampel Syndrome
Managing Schwartz-Jampel Syndrome requires a multifaceted approach tailored to individual symptoms. Treatment strategies often focus on alleviating myotonic symptoms and improving overall mobility.
Medications play a crucial role in symptom management. Muscle relaxants can help reduce stiffness and discomfort, while anticonvulsants may be prescribed for muscle spasms. Addressing pain is essential for enhancing daily functioning.
Physical and occupational therapy are vital components of treatment plans. These therapies target strength building and flexibility, thereby fostering independence in daily activities.
Surgical interventions might be necessary for skeletal deformities or severe joint issues that impede movement. Orthopedic specialists often collaborate with the healthcare team to determine appropriate surgical options.
Moreover, close monitoring by healthcare professionals ensures that any emerging complications are addressed promptly. This comprehensive care strategy helps those affected lead more fulfilling lives amidst the challenges posed by Schwartz-Jampel Syndrome.
Pharmacological Interventions: Medications Used in SJS Management
Pharmacological interventions play a vital role in managing Schwartz-Jampel Syndrome (SJS). Medications aim to alleviate symptoms and improve the quality of life for affected individuals.
One common approach involves using muscle relaxants. Drugs like baclofen can help reduce myotonia, offering relief from muscle stiffness.
Anticonvulsants such as lamotrigine may also be employed. These can assist with controlling involuntary movements and improving overall muscle function.
Pain management is crucial due to associated musculoskeletal discomfort. Non-steroidal anti-inflammatory drugs (NSAIDs) are often prescribed to manage pain effectively.
Additionally, certain agents might target specific complications related to SJS, including skeletal abnormalities or growth issues. Each treatment plan remains tailored to the individual’s needs.
Regular monitoring by healthcare professionals ensures that therapy adjustments occur as necessary, optimizing patient outcomes in their journey with Schwartz-Jampel Syndrome.
Surgical Options: Addressing Skeletal and Muscular Complications
Surgical options for Schwartz-Jampel Syndrome focus on alleviating skeletal and muscular complications. These interventions aim to improve mobility and enhance the quality of life.
Orthopedic surgery is often considered for patients with significant skeletal deformities. Procedures like corrective osteotomies can realign bones, providing better function and reducing discomfort.
In cases of severe myotonia or muscle stiffness, surgical techniques such as tendon lengthening may be employed. This approach helps to relieve tension in affected muscles, allowing for smoother movement.
Additionally, some patients might require interventions to address joint issues that arise from muscle imbalances. Stabilization surgeries can enhance joint function while minimizing pain during daily activities.
Collaboration between surgeons and rehabilitation specialists is essential for optimal patient outcomes. Tailoring each surgical plan according to individual needs ensures a comprehensive approach toward managing Schwartz-Jampel Syndrome effectively.
Physical and Occupational Therapy: Improving Function and Quality of Life
Physical and occupational therapy play crucial roles in the management of Schwartz-Jampel Syndrome. These therapies focus on enhancing mobility and functional independence for patients.
Physical therapy aims to strengthen muscles and improve coordination. Tailored exercises help manage myotonia, allowing individuals to engage more freely in daily activities. Therapists use various techniques, including stretching and resistance training, to address musculoskeletal challenges.
Occupational therapy complements physical interventions by focusing on everyday tasks. It assists patients in adapting their environments, enabling them to perform self-care routines with greater ease. Techniques may include the use of specialized tools or modifications that enhance accessibility.
Both therapies foster confidence and self-sufficiency. They provide supportive environments where patients can explore their limits while developing new skills. Engaging consistently in these therapeutic practices can significantly elevate quality of life for individuals living with Schwartz-Jampel Syndrome.
Anesthesia Considerations: Special Precautions for SJS Patients
Anesthesia management for patients with Schwartz-Jampel Syndrome (SJS) requires careful planning. Due to myotonia, muscle stiffness can pose challenges during intubation and postoperative recovery.
Anesthesiologists should be aware of the potential for prolonged neuromuscular block in SJS patients. This condition may lead to increased sensitivity to certain anesthetics. Therefore, a thorough assessment prior to any procedure is crucial.
Monitoring should include continuous evaluation of respiratory function and muscle tone. Adjustments in medication dosages might be necessary based on individual responses.
The risk of complications increases when considering skeletal abnormalities commonly associated with SJS. Positioning during surgery must prioritize comfort and stability.
Collaboration among specialists is vital for optimizing patient safety throughout the anesthesia process. Open communication between the surgical team and anesthesiologist enhances preparedness for unexpected occurrences related to this rare genetic condition.
Living with Schwartz-Jampel Syndrome: Daily Challenges and Adaptations
Living with Schwartz-Jampel Syndrome presents a variety of daily challenges. Individuals may experience muscle stiffness and myotonia, which can affect mobility. Simple tasks like walking or climbing stairs often require extra effort and planning.
Daily routines might need adjustments to accommodate these physical limitations. Activities that involve prolonged standing or extensive use of muscles can be particularly taxing.
Social interactions can also be influenced by the syndrome’s distinctive facial features. This may lead to feelings of self-consciousness in certain situations, necessitating support from family and friends.
Adaptations at home are vital for enhancing quality of life. Installing grab bars in bathrooms or using specialized utensils can make everyday activities easier.
Moreover, establishing a consistent routine supports emotional well-being. Regular check-ins with healthcare providers help manage symptoms effectively while ensuring that individuals feel empowered in their journey.
Pediatric SJS: Special Considerations in Childhood
Pediatric patients with Schwartz-Jampel Syndrome (SJS) face unique challenges as they grow. The condition can impact their physical development and daily activities significantly.
Early diagnosis is crucial. Physicians often monitor growth patterns closely to identify any deviations that might indicate complications related to SJS. Regular assessments help tailor interventions appropriately.
Children may experience muscle stiffness, which affects movement and coordination. This can lead to difficulties in participating in typical childhood activities, such as sports or playtime with peers.
Emotional support is vital for these young patients. They may feel isolated due to their symptoms or differences from other children. Building a supportive environment at home and school encourages social interaction and helps foster resilience.
Collaboration among healthcare providers, educators, and families ensures that pediatric SJS patients receive comprehensive care tailored specifically for their developmental needs.
Research Horizons: Current Studies and Future Directions in SJS Treatment
As the understanding of Schwartz-Jampel Syndrome (SJS) continues to evolve, researchers are actively exploring innovative approaches to treatment and management. Current studies focus on gene therapy as a potential long-term solution for addressing the underlying genetic mutations associated with SJS. By targeting the HSPG2 gene, scientists hope to provide more effective interventions that could mitigate symptoms significantly.
Another area of research is centered around pharmacological advancements. New medications are being tested for their efficacy in managing myotonia and other neuromuscular symptoms characteristic of SJS. Collaborative efforts among clinicians and geneticists aim to create comprehensive treatment plans that can improve patient outcomes across various age groups.
Clinical trials are also underway investigating physical therapies tailored specifically for individuals with SJS. These therapies not only address muscle strength but also enhance mobility and quality of life through personalized rehabilitation programs.
Moreover, increased awareness about Schwartz-Jampel Syndrome is fostering community support initiatives aimed at providing resources for affected families. This grassroots approach ensures that patients receive holistic care while advancing our collective knowledge about this rare condition.
The future looks promising as ongoing research endeavors strive toward unlocking new insights into Schwartz-Jampel Syndrome’s complexities while improving therapeutic options available today. As we stand on the brink of these exciting developments, it’s clear that collaboration between researchers, healthcare professionals, and patient communities will play an integral role in shaping the landscape of SJS treatment moving forward.