1. Introduction to Idiopathic Syndromes
Idiopathic syndromes often leave patients and healthcare providers alike scratching their heads. These mysterious conditions, characterized by an unknown cause or origin, can be challenging to diagnose and manage. With a name that literally means “of unknown origin,” idiopathic syndromes encompass a wide range of disorders affecting various systems in the body.
As medical science continues to advance, our understanding of these elusive conditions expands. This blog post aims to shed light on idiopathic syndromes—what they are, how they differ from other types of disorders, and what every patient should know about them.
Whether you’re dealing with symptoms yourself or simply seeking knowledge for someone who is, this comprehensive guide will provide valuable insights into the world of idiopathic conditions. Join us as we explore everything from common examples to emerging research trends that could illuminate these perplexing health issues.
1.1. Definition and Characteristics
Idiopathic syndromes are medical conditions characterized by an unknown cause. Unlike other disorders, where a specific origin can often be identified, idiopathic conditions leave healthcare professionals puzzled. This uncertainty poses significant challenges in diagnosis and treatment.
These syndromes can manifest across various systems within the body, affecting patients differently. Symptoms may range from mild to severe and can evolve over time. The unpredictability of these symptoms adds to the complexity faced by both patients and doctors.
“Why Does Chronic Fatigue Syndrome Cause Persistent Tiredness?”
Patients with idiopathic syndromes often experience frustration due to the lack of clear explanations for their health issues. As research continues, understanding these enigmatic disorders is vital for developing targeted therapies that address both symptoms and underlying mechanisms more effectively.
1.2. Historical Perspective on Idiopathic Disorders
The historical journey of idiopathic disorders reveals a fascinating evolution in medical understanding. Initially, many conditions were labeled as “idiopathic” simply due to insufficient knowledge. Early physicians often attributed unexplained illnesses to imbalances in bodily humors or mystical forces.
“What Triggers Cushing’s Syndrome? Complete Hormone Guide”
As science progressed, the advent of modern medicine began to shed light on these enigmatic syndromes. The 19th century saw significant advancements in pathology and microbiology, leading doctors to reconsider their approach to unknown diseases.
The introduction of diagnostic technologies further changed the landscape. Imaging techniques and lab tests allowed for more precise investigation into previously misunderstood symptoms.
Despite this progress, idiopathic disorders remain challenging; they emphasize the limits of current medical knowledge while highlighting an ongoing quest for answers within our biological systems. Each new discovery opens doors but also raises questions about what we still don’t know about these perplexing conditions.
2. Understanding Idiopathic Conditions
Idiopathic conditions are those for which the cause remains unknown. This classification can be perplexing, as even extensive medical evaluations may yield no definitive answers.
To qualify as idiopathic, a condition must meet specific criteria that exclude known causes. It requires thorough investigation to ensure other potential explanations have been ruled out.
“How Does Carpal Tunnel Syndrome Develop? Prevention Tips”
Distinguishing idiopathic syndromes from other types is crucial for proper diagnosis and treatment planning. While some conditions might seem similar, their underlying mechanisms can differ significantly.
The concept of unknown etiology plays an important role in medicine today. It highlights the need for ongoing research into these mysterious disorders, urging scientists and clinicians alike to explore new avenues for understanding and addressing them effectively.
2.1. Criteria for Idiopathic Classification
Identifying idiopathic syndromes involves specific criteria. First, a comprehensive medical history is crucial. This includes previous diagnoses and treatments that may or may not have worked.
Next, physicians must rule out known causes. This exclusion process helps ensure the syndrome genuinely lacks an identifiable etiology. Diagnostic tests play a significant role here; imaging studies and laboratory tests can assist in this effort.
“What Makes Cauda Equina Syndrome a Medical Emergency?”
Another important aspect is the consistency of symptoms over time. Idiopathic conditions typically exhibit stable manifestations despite varying circumstances.
Patient-reported outcomes are vital for classification. Understanding how symptoms affect daily life provides insights into the overall impact of the disorder on well-being.
Together, these criteria create a framework for accurately identifying idiopathic syndromes amidst complex clinical presentations.
2.2. Distinguishing Idiopathic from Other Syndrome Types
Idiopathic syndromes are often perplexing, primarily due to their classification. Unlike other syndrome types, idiopathic conditions arise without a clear cause or identifiable pathological mechanism. This absence of known etiology sets them apart.
“Why Does CHARGE Syndrome Affect Multiple Body Systems?”
Other syndromes might be linked to genetic factors, infections, or environmental triggers. For instance, autoimmune disorders have specific immune responses as their foundation. In contrast, idiopathic syndromes lack such defined origins.
Diagnosis also varies significantly between the two categories. Clinicians approach idiopathic cases through exclusionary methods since established tests may not yield conclusive results.
The implications for treatment can differ dramatically as well. While targeted therapies exist for conditions with known causes, treating idiopathic syndromes often focuses on symptom management and supportive care rather than addressing an underlying pathology that remains elusive. Understanding these distinctions helps patients navigate their diagnosis effectively and engage in meaningful discussions with healthcare providers.
2.3. The Role of Unknown Etiology in Medicine
Unknown etiology plays a crucial role in the field of medicine, particularly when it comes to idiopathic syndromes. These conditions often defy clear diagnosis and understanding, leaving both patients and healthcare providers at a loss.
“How Does Complex Regional Pain Syndrome Cause Chronic Pain?”
The mystery surrounding unknown causes can lead to extensive research efforts. Scientists delve into genetic, environmental, and lifestyle factors that may contribute to these unexplained health issues. Such investigations aim to uncover potential links that could pave the way for better treatment options.
However, dealing with unknown etiology also presents challenges. Patients frequently navigate uncertainty regarding their condition’s nature and prognosis. This lack of clarity can be frustrating and even anxiety-inducing as they seek answers without definitive explanations.
“What Causes Cri du Chat Syndrome? Understanding Cat Cry Disease”
Despite its complexities, studying unknown etiology is vital for advancing medical knowledge. It encourages innovation in diagnostic methods and fosters collaboration across various disciplines within healthcare research.
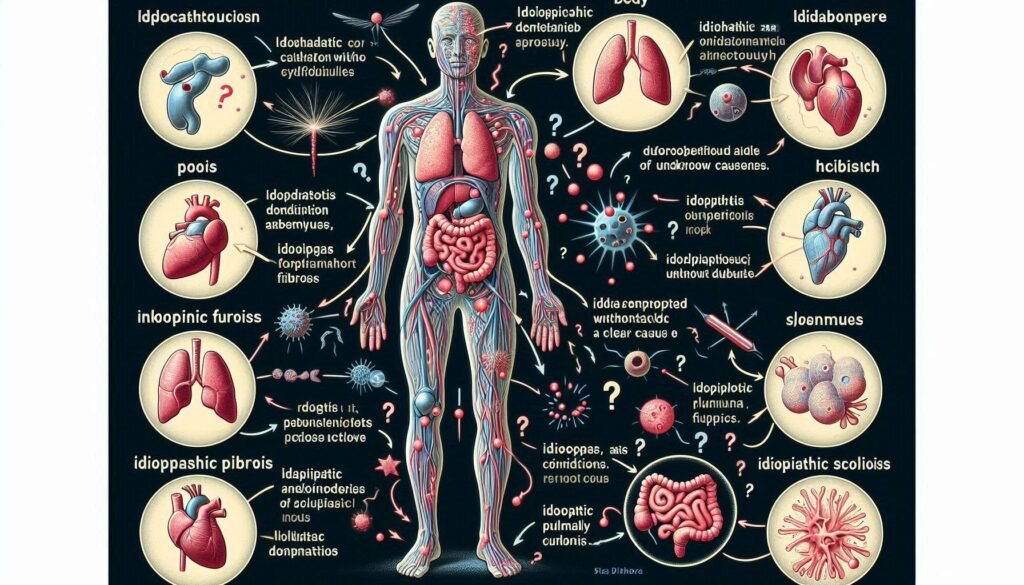
3. Common Idiopathic Syndromes
Idiopathic syndromes encompass various medical conditions with no identifiable cause. Among the most notable is Idiopathic Thrombocytopenic Purpura (ITP). This disorder manifests as low platelet counts, leading to easy bruising and bleeding. Patients often experience fatigue and may require treatments like corticosteroids or splenectomy.
Another common idiopathic condition is Idiopathic Pulmonary Fibrosis (IPF), a progressive lung disease characterized by scarring of lung tissue. Symptoms include persistent dry cough and difficulty breathing, significantly impacting quality of life. Treatment options focus on slowing progression through antifibrotic medications.
“How Does Dandy-Walker Syndrome Affect Brain Development?”
Chronic Fatigue Syndrome (CFS/ME) also falls under this category, presenting with profound fatigue that doesn’t improve with rest. Associated symptoms can include sleep disturbances and cognitive difficulties. Management strategies often incorporate lifestyle changes alongside supportive therapies to enhance daily functioning for those affected.
3.1. Idiopathic Thrombocytopenic Purpura (ITP)
Idiopathic Thrombocytopenic Purpura (ITP) is a condition characterized by low platelet counts in the blood. This reduction can lead to easy bruising, bleeding gums, and tiny red or purple spots on the skin known as petechiae.
The exact cause of ITP remains unknown, which classifies it as “idiopathic.” The immune system mistakenly attacks and destroys platelets, contributing to this disorder. It can occur at any age but is more prevalent in adults and children.
Diagnosis typically involves blood tests to measure platelet levels alongside ruling out other potential causes. Treatment options vary based on severity, ranging from watchful waiting for mild cases to medications that suppress the immune response or procedures like splenectomy in more severe situations.
Living with ITP requires careful management and regular monitoring. Patients often adapt their lifestyles to avoid injuries while managing symptoms effectively with medical guidance.
3.2. Idiopathic Pulmonary Fibrosis (IPF)
Idiopathic Pulmonary Fibrosis (IPF) is a chronic lung disease characterized by progressive scarring of the lung tissue. This fibrosis thickens the lungs, making it increasingly difficult for oxygen to enter the bloodstream.
The exact cause of IPF remains unknown, which is why it’s classified as “idiopathic.” Factors like genetic predisposition and environmental exposures may contribute to its development.
Patients often experience symptoms such as shortness of breath and a persistent dry cough. These symptoms can worsen over time, significantly impacting quality of life.
Diagnosis typically involves imaging tests, such as high-resolution CT scans, along with pulmonary function tests. Early detection is crucial for managing this complex condition effectively. Treatment options include antifibrotic medications that help slow disease progression and improve survival rates in some patients.
3.3. Chronic Fatigue Syndrome (CFS/ME)
Chronic Fatigue Syndrome, also known as CFS or ME (Myalgic Encephalomyelitis), is a complex disorder characterized by extreme fatigue that doesn’t improve with rest. This persistent exhaustion often worsens after physical or mental exertion.
Patients may experience a range of symptoms, including sleep disturbances, muscle pain, and cognitive difficulties such as memory loss or difficulty concentrating. The unpredictability of symptoms can severely impact daily life and limit activities.
The exact cause remains unclear, complicating diagnosis and treatment. Some theories suggest a combination of factors might be involved—viral infections, immune system changes, hormonal imbalances, or even environmental triggers.
Management typically focuses on alleviating symptoms through lifestyle adjustments and supportive therapies rather than curative approaches. Understanding this syndrome is crucial for both patients seeking relief and healthcare providers aiming to offer appropriate care tailored to individual needs.
4. Neurological Idiopathic Syndromes
Neurological idiopathic syndromes present a unique challenge in medicine due to their unclear origins. These conditions often perplex both patients and healthcare providers alike.
Idiopathic Intracranial Hypertension (IIH) is one such syndrome, characterized by increased pressure within the skull without an identifiable cause. Symptoms include severe headaches and vision problems, making it critical for early diagnosis and management.
Bell’s Palsy affects facial muscles suddenly, leading to temporary paralysis on one side of the face. Although its exact cause remains unknown, stress or viral infections may trigger this condition.
Restless Legs Syndrome (RLS) disrupts sleep with uncomfortable sensations that create an irresistible urge to move the legs. Patients frequently describe RLS as a frustrating and exhausting experience that impacts daily life significantly.
Each of these neurological syndromes shares a common thread—their origins remain elusive—yet they highlight the complexity of human health and disease.
4.1. Idiopathic Intracranial Hypertension
Idiopathic Intracranial Hypertension (IIH) is a condition characterized by increased pressure within the skull without an obvious cause. This syndrome primarily affects young, overweight women but can occur in anyone.
Symptoms often include headaches, visual disturbances, and tinnitus. The headaches are typically severe and may mimic migraines. Vision changes can range from blurred vision to temporary loss of sight due to swelling of the optic nerve.
Diagnosis usually involves imaging studies such as MRI or CT scans to rule out other conditions that might increase intracranial pressure. A lumbar puncture may also be performed to measure cerebrospinal fluid pressure directly.
Treatment options for IIH aim at reducing intracranial pressure and alleviating symptoms. Weight loss has shown benefits, while medications like acetazolamide can help lower fluid production in the brain. In some cases, surgical interventions may be necessary if conservative measures fail.
4.2. Bell’s Palsy
Bell’s Palsy is a sudden, temporary weakness or paralysis of the facial muscles. It can affect one side of the face, causing drooping and difficulty with facial expressions. This condition manifests quickly, often overnight.
The exact cause remains uncertain, but it’s believed to be linked to viral infections like herpes simplex virus. Stress and genetic factors may also play a role in its onset.
Symptoms typically include loss of ability to close one eye, drooling, and altered taste sensations. Many patients report pain around the jaw or behind the ear before muscle weakness occurs.
Most people make a full recovery within weeks to months. Treatment options focus on symptom relief and may involve corticosteroids to reduce inflammation. Physical therapy can also aid in regaining muscle strength and function during recovery.
Understanding Bell’s Palsy helps demystify this syndrome for patients experiencing its distressing effects.
4.3. Restless Legs Syndrome
Restless Legs Syndrome (RLS) is a neurological disorder characterized by an irresistible urge to move the legs. This sensation often accompanies uncomfortable feelings, such as itching or crawling.
Symptoms typically worsen during periods of inactivity, particularly in the evenings and at night. Many individuals find relief through movement, making sleep elusive for those affected.
The exact cause of RLS remains unclear, but it may have genetic components and links to iron deficiency. Certain medications or underlying health conditions can also exacerbate symptoms.
Diagnosis usually involves a clinical evaluation based on patient history and symptom description. While there’s no cure, lifestyle changes and various treatments can help manage symptoms effectively.
Patients are encouraged to maintain regular sleep patterns and engage in moderate exercise. Consulting with healthcare professionals is essential for personalized management strategies tailored to individual needs.
5. Autoimmune and Inflammatory Idiopathic Syndromes
Autoimmune and inflammatory idiopathic syndromes are perplexing conditions where the immune system mistakenly attacks healthy tissues without a clear cause. This group highlights the body’s miscommunication, leading to various symptoms that can significantly impact daily life.
Sarcoidosis is one such syndrome characterized by granuloma formation in multiple organs, particularly the lungs. The origins remain uncertain, complicating diagnosis and treatment options.
Behçet’s disease presents with recurrent oral ulcers and skin lesions, often linked to systemic involvement. Its unpredictable nature poses challenges for patients seeking effective management strategies.
Kawasaki disease primarily affects children, triggering inflammation of blood vessels. It’s critical since it can lead to serious heart complications if not promptly addressed.
Understanding these autoimmune conditions requires ongoing research into their etiologies and better ways to support affected individuals as they navigate complex health landscapes.
5.1. Sarcoidosis
Sarcoidosis is an inflammatory disease characterized by the formation of tiny clusters of immune cells, known as granulomas. These can appear in various organs but most commonly affect the lungs, lymph nodes, skin, and eyes.
The exact cause remains unknown. Genetic predisposition and environmental factors may play a role in its development. Symptoms often vary widely among individuals and can range from mild to severe. Common manifestations include persistent cough, shortness of breath, fatigue, and skin rashes.
Diagnosis typically involves a combination of medical history review, imaging studies like chest X-rays or CT scans, and sometimes biopsies to confirm granuloma presence. Treatment focuses on managing symptoms; corticosteroids are frequently prescribed to reduce inflammation when necessary.
Though many people recover completely without treatment, some may experience chronic issues related to organ function or other complications over time. Ongoing research aims to uncover underlying mechanisms driving sarcoidosis.
5.2. Behçet’s Disease
Behçet’s Disease is a rare, chronic inflammatory condition characterized by recurrent oral and genital ulcers. It often also causes eye inflammation, leading to potential vision loss.
The disease is classified as an autoimmune disorder, meaning the body’s immune system mistakenly attacks its own tissues. Symptoms can vary widely among individuals and may include skin lesions, joint pain, and vascular complications.
Diagnosis typically involves clinical evaluation of symptoms alongside exclusion of other conditions. There are no definitive tests for Behçet’s; it relies heavily on patient history and symptom presentation.
Treatment usually focuses on managing flare-ups with anti-inflammatory medications or corticosteroids. In some cases, immunosuppressive drugs may be prescribed to reduce severity and frequency of episodes.
Research continues into the underlying mechanisms of Behçet’s Disease, aiming to uncover genetic factors that contribute to its development in certain populations.
5.3. Kawasaki Disease
Kawasaki Disease is an acute inflammatory condition primarily affecting children. Characterized by fever, rash, and swollen lymph nodes, it can lead to serious cardiovascular complications if not treated promptly.
The exact cause remains unknown, which classifies it as idiopathic. However, some theories suggest a possible viral or bacterial trigger that leads to inflammation of blood vessels throughout the body.
A hallmark symptom includes a distinctive rash and red eyes. Patients may also exhibit changes in their lips and mouth area. Early diagnosis is crucial for effective treatment options.
Intravenous immunoglobulin (IVIG) therapy is commonly used to reduce inflammation and prevent heart issues. With prompt medical care, most children recover well without lasting effects on their health.
Ongoing research aims at understanding triggers better and improving early detection methods for this enigmatic disease. Awareness among parents about Kawasaki Disease symptoms can ensure timely intervention.
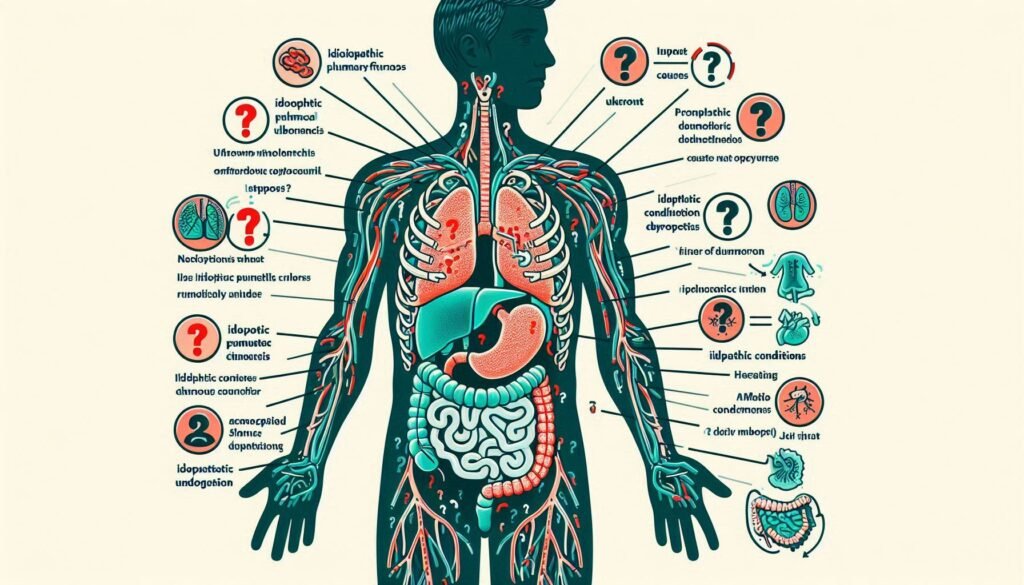
6. Gastrointestinal Idiopathic Syndromes
Gastrointestinal idiopathic syndromes encompass a range of conditions where the exact cause remains elusive. These disorders can significantly affect patients’ daily lives, often leading to chronic discomfort and unpredictability in symptoms.
Irritable Bowel Syndrome (IBS) is one common example. IBS presents with abdominal pain, bloating, and changes in bowel habits without any identifiable organic disease. Its management focuses on dietary modifications and symptom relief.
Functional Dyspepsia also falls into this category. Patients experience persistent stomach discomfort that doesn’t stem from any structural abnormalities or serious health issues.
Cyclic Vomiting Syndrome is another troubling condition characterized by recurrent episodes of severe vomiting that can last for hours to days. The absence of clear diagnostic markers complicates its treatment, requiring tailored approaches based on individual patient needs.
Understanding these syndromes remains critical for improving patient care and enhancing quality of life amidst uncertainty surrounding their origins.
6.1. Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder affecting millions worldwide. It primarily manifests as abdominal pain, bloating, and changes in bowel habits, including diarrhea or constipation.
The exact cause of IBS remains unclear, making its management challenging. However, various factors such as stress, diet, and gut microbiota imbalance often trigger symptoms. Individuals may find relief through lifestyle modifications like dietary adjustments and stress management techniques.
Diet plays a significant role in managing IBS symptoms. Many patients benefit from identifying food triggers—common culprits include gluten-containing grains and high-FODMAP foods. Keeping a food diary can be helpful for tracking these patterns.
While there is no definitive cure for IBS, treatment options range from dietary changes to medications aimed at alleviating specific symptoms. Support groups also provide valuable emotional support for those navigating this chronic condition.
6.2. Functional Dyspepsia
Functional dyspepsia is a common gastrointestinal disorder characterized by persistent or recurrent pain in the upper abdomen. Patients often report a feeling of fullness, bloating, and discomfort after meals. Unlike other digestive conditions, functional dyspepsia does not demonstrate any identifiable organic cause.
The exact mechanisms behind this syndrome remain unclear. Factors such as gastric motility issues, heightened sensitivity to stomach distension, and psychosocial stressors may contribute to its development.
Diagnosis typically involves ruling out other potential causes through endoscopy or imaging studies. Treatment options focus on symptom relief and may include dietary changes, medications to reduce acid production, and therapies aimed at managing anxiety or depression associated with the condition.
Living with functional dyspepsia can significantly impact quality of life. Understanding symptoms and triggers can empower patients to better manage their experiences and seek appropriate care when necessary.
6.3. Cyclic Vomiting Syndrome
Cyclic Vomiting Syndrome (CVS) is a complex disorder characterized by recurrent episodes of severe vomiting. These attacks can last for hours or even days, often occurring in cycles. Patients typically experience periods of intense nausea followed by intervals of relief.
The precise cause remains unclear, but it may be linked to genetic factors, migraines, and gastrointestinal dysregulation. Children are the most commonly affected demographic, though adults can also suffer from this debilitating condition.
Symptoms often include abdominal pain and extreme fatigue during vomiting episodes. Between these bouts, individuals usually feel perfectly healthy.
Diagnosis is challenging due to the episodic nature of CVS. Medical professionals rely on patient history and exclusion criteria to differentiate it from other gastrointestinal disorders. Treatment options focus on managing symptoms and preventing future episodes through lifestyle modifications and medications tailored to individual needs.
7. Musculoskeletal Idiopathic Syndromes
Musculoskeletal idiopathic syndromes encompass a range of conditions characterized by unexplained pain and dysfunction in the body’s musculoskeletal system. These syndromes can significantly impact daily life, often leaving patients with persistent discomfort.
Fibromyalgia is one prominent example, presenting widespread tenderness and fatigue without any identifiable cause. Those affected may experience disrupted sleep patterns and cognitive difficulties, commonly referred to as “fibro fog.”
Another notable condition is Complex Regional Pain Syndrome (CRPS), which usually arises after an injury but manifests with disproportionate pain levels that linger long after healing. This syndrome can also lead to changes in skin color, temperature, and swelling.
Juvenile Idiopathic Arthritis (JIA) primarily affects children and leads to joint inflammation. The causes remain unclear but can result in chronic pain and potential long-term disability if not managed effectively.
Understanding these musculoskeletal conditions requires ongoing research into their underlying mechanisms for better treatment options.
7.1. Fibromyalgia
Fibromyalgia is a chronic condition characterized by widespread musculoskeletal pain. It often comes with fatigue, sleep disturbances, and cognitive difficulties known colloquially as “fibro fog.”
The exact cause of fibromyalgia remains unclear, but it is believed to involve genetic, environmental, and psychological factors. Many patients report that stress or trauma can trigger symptoms.
Diagnosis typically includes ruling out other conditions through various tests since no definitive test exists for fibromyalgia. Healthcare providers rely on patient history and symptom evaluation.
Treatment usually focuses on managing symptoms rather than curing the disorder. A combination of medication, physical therapy, exercise programs, and lifestyle changes can help improve quality of life.
Support groups are beneficial for many individuals coping with this complex syndrome. They provide an opportunity to connect with others facing similar challenges and share effective coping strategies.
7.2. Complex Regional Pain Syndrome
Complex Regional Pain Syndrome (CRPS) is a chronic pain condition that usually affects a limb following an injury or surgery. The hallmark of this syndrome is prolonged and often severe pain, which is out of proportion to the initial injury.
Patients with CRPS may experience changes in skin color, temperature, and texture where the affected limb becomes hypersensitive. These symptoms can be accompanied by swelling and abnormal hair growth.
The exact cause remains unclear, but it’s believed to involve nerve dysfunction and inflammatory processes. This makes diagnosing CRPS particularly challenging since it mimics other conditions.
Treatment options vary widely and include physical therapy, medications for pain relief, and sometimes psychological support. Some patients find relief via nerve blocks or alternative therapies like acupuncture.
Living with CRPS can significantly impact daily life by affecting mobility and mental well-being. Understanding this complex disorder helps both patients and caregivers navigate its challenges more effectively.
7.3. Juvenile Idiopathic Arthritis
Juvenile Idiopathic Arthritis (JIA) is a chronic inflammatory condition affecting children under the age of 16. It manifests as joint swelling, pain, and stiffness that can significantly impact a child’s daily activities.
There are several subtypes of JIA, including oligoarticular, polyarticular, and systemic forms. The symptoms may vary depending on the subtype but often include fatigue and fever alongside joint issues.
Early diagnosis is crucial for effective management. Pediatric rheumatologists typically lead treatment plans that focus on reducing inflammation and preserving joint function. Medications like nonsteroidal anti-inflammatory drugs (NSAIDs) or disease-modifying antirheumatic drugs (DMARDs) are commonly prescribed.
Physical therapy plays an essential role in maintaining flexibility and strength in affected joints. Support from family and schools also helps children cope with this challenging condition while pursuing their everyday life goals.
8. Dermatological Idiopathic Syndromes
Dermatological idiopathic syndromes present unique challenges for both patients and healthcare providers. These conditions often lack a clear cause, making diagnosis and treatment complex.
Idiopathic guttate hypomelanosis leads to small white spots on the skin. It typically affects sun-exposed areas and is more common in older adults. Although it’s harmless, many seek cosmetic solutions due to its appearance.
Lichen planus is another intriguing condition characterized by purplish, itchy lesions on the skin or mucous membranes. Its exact origin remains uncertain but may involve immune system responses triggered by stress or medications.
Erythema nodosum manifests as painful red nodules under the skin, commonly on shins. While it’s often linked to infections or medications, many cases remain unexplained, highlighting the need for further research into dermatological idiopathic syndromes. Understanding these diseases can empower patients with knowledge about their health journey.
8.1. Idiopathic Guttate Hypomelanosis
Idiopathic Guttate Hypomelanosis (IGH) is a dermatological condition characterized by small, white spots on the skin. These spots typically appear on sun-exposed areas, such as the arms and legs. The exact cause remains elusive, hence the term “idiopathic.”
Although IGH primarily affects older adults, it can present in younger individuals too. The white patches arise from a reduction in melanin production but do not indicate any harm or underlying disease.
Patients often seek treatment for cosmetic reasons rather than health concerns. While topical treatments may be suggested to camouflage these spots, there’s no definitive cure available.
Understanding this syndrome requires awareness that it is harmless and does not progress to more severe conditions. However, regular skin checks remain essential for monitoring overall skin health and ruling out other dermatological issues.
8.2. Lichen Planus
Lichen Planus is a chronic inflammatory condition that primarily affects the skin and mucous membranes. It manifests as purplish, itchy lesions with a distinct lacy pattern. These lesions can appear anywhere on the body but are often found on the wrists, ankles, and lower back.
The exact cause remains unclear, which places it firmly in the idiopathic category. However, some researchers suggest it may involve an autoimmune response where the body’s immune system mistakenly attacks its own cells.
In addition to skin symptoms, Lichen Planus can also affect oral health. Patients may experience painful sores or white patches inside their mouths. Treatment options typically focus on managing discomfort through topical corticosteroids or other immunosuppressive agents to reduce inflammation.
Regular dermatological evaluations play a crucial role in monitoring this condition’s progression and preventing potential complications like scarring or secondary infections.
8.3. Erythema Nodosum
Erythema nodosum is a skin condition characterized by painful, red nodules that typically develop on the lower legs. These raised lesions can be tender to touch and may vary in size from small bumps to larger plaques.
The exact cause of erythema nodosum often remains unknown, classifying it as an idiopathic syndrome. However, it can be associated with various underlying conditions such as infections, medications, or autoimmune diseases. Common triggers include streptococcal infections and certain drugs like sulfonamides.
Diagnosis usually involves a thorough medical history and physical examination. Sometimes a biopsy is performed for confirmation. Treatment primarily focuses on alleviating symptoms through pain relief measures and addressing any underlying causes when identified.
Patients may also benefit from rest and elevation of affected limbs during flare-ups. While most cases resolve spontaneously within weeks, recurrences are possible depending on individual risk factors.
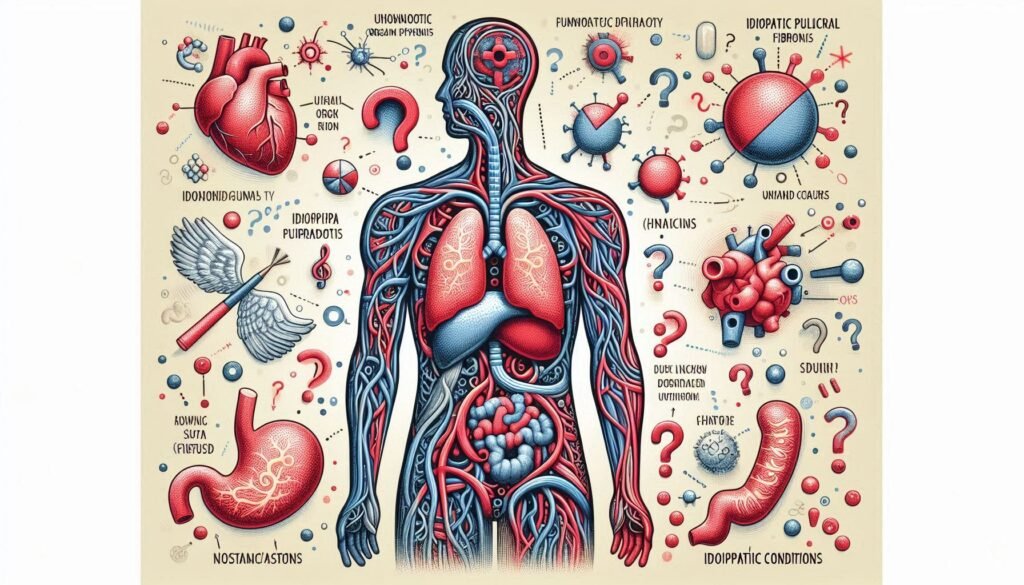
9. Cardiovascular Idiopathic Syndromes
Cardiovascular idiopathic syndromes encompass a range of conditions where the underlying cause remains unknown. They can significantly impact heart and vascular health, leading to various symptoms that often challenge both patients and healthcare providers.
Idiopathic Pulmonary Arterial Hypertension (IPAH) is one such syndrome. It involves high blood pressure in the pulmonary arteries without any identifiable cause. This condition can lead to serious complications if not managed appropriately.
Postural Orthostatic Tachycardia Syndrome (POTS) presents as an abnormal increase in heart rate when transitioning from lying down to standing up. Patients may experience dizziness, palpitations, and fatigue, which can disrupt daily activities.
Idiopathic Ventricular Fibrillation poses another concern; it triggers life-threatening arrhythmias with no clear origin. Understanding these syndromes is crucial for effective management and improving patient outcomes in cardiovascular health.
9.1. Idiopathic Pulmonary Arterial Hypertension
Idiopathic Pulmonary Arterial Hypertension (IPAH) is a rare and progressive condition characterized by high blood pressure in the pulmonary arteries. This elevation can lead to significant strain on the heart, ultimately resulting in heart failure.
The exact cause of IPAH remains unknown, which adds complexity to its diagnosis and treatment. Patients often experience symptoms such as shortness of breath, fatigue, chest pain, and lightheadedness. These symptoms may initially be mistaken for other conditions.
Diagnosis typically involves a series of tests including echocardiograms and right heart catheterization to measure pressure within the pulmonary arteries directly.
While there is no cure for IPAH, various treatments aim to alleviate symptoms and improve quality of life. Options include vasodilators that help widen blood vessels and enhance blood flow. Regular monitoring is essential due to potential disease progression over time.
9.2. Postural Orthostatic Tachycardia Syndrome (POTS)
Postural Orthostatic Tachycardia Syndrome, commonly referred to as POTS, is a condition that significantly impacts daily life. It typically affects individuals when they change positions, particularly from lying down to standing.
Patients often experience an abnormal increase in heart rate—usually over 30 beats per minute—within ten minutes of standing. This sudden spike can lead to symptoms like dizziness, fatigue, and even fainting episodes.
POTS is more prevalent among young women but can affect anyone at any age. The underlying causes remain varied and may include autonomic nervous system dysfunction or after viral infections.
Management of POTS focuses on lifestyle changes such as increased fluid intake and salt consumption. Medications may also be prescribed to help regulate heart rate and improve blood circulation for better quality of life.
9.3. Idiopathic Ventricular Fibrillation
Idiopathic Ventricular Fibrillation (IVF) is a rare but serious cardiac condition characterized by erratic electrical activity in the heart’s ventricles. This disorganized rhythm can lead to sudden cardiac arrest if not treated immediately.
The term “idiopathic” indicates that the exact cause of IVF remains unknown, complicating diagnosis and treatment. Patients typically present with palpitations or syncope without any clear underlying heart disease or structural anomalies.
Risk factors may include genetic predispositions, especially among younger individuals. Some studies suggest a link between IVF and hereditary arrhythmia syndromes, though definitive connections are still being explored.
Management often involves implantable cardioverter-defibrillators (ICDs) to prevent fatal arrhythmic events. Further research into genetic testing and advanced imaging techniques aims to improve understanding and care for those affected by this perplexing syndrome.
10. Endocrine and Metabolic Idiopathic Syndromes
Endocrine and metabolic idiopathic syndromes encompass a range of conditions with unclear origins. These disorders can disrupt normal hormonal functions, leading to various health complications.
Idiopathic hypogonadotropic hypogonadism is one such syndrome. It results in low levels of sex hormones due to insufficient stimulation from the pituitary gland. Patients often experience delayed puberty or infertility without any identifiable cause.
Central diabetes insipidus presents another challenge. This condition involves improper regulation of water balance in the body, resulting in excessive thirst and urination. Despite extensive testing, many cases remain idiopathic.
Idiopathic hypercalciuria highlights another complexity within this category. Characterized by high calcium levels in urine, it may lead to kidney stones over time. Its underlying mechanisms are frequently elusive, complicating effective treatment strategies.
Understanding these syndromes is crucial for developing targeted therapies that improve patient outcomes while addressing their unique challenges.
10.1. Idiopathic Hypogonadotropic Hypogonadism
Idiopathic Hypogonadotropic Hypogonadism (IHH) is a condition characterized by low levels of sex hormones due to insufficient stimulation from the pituitary gland. This lack of hormone secretion leads to delayed puberty and reproductive issues in both males and females.
Patients often present with symptoms such as reduced libido, infertility, and physical changes associated with underdeveloped sexual characteristics. Diagnosis typically involves hormonal evaluations alongside imaging studies to assess pituitary gland function.
The etiology remains unclear for many diagnosed cases, hence the term “idiopathic.” Genetic factors may play a role; however, environmental influences are also under investigation.
Treatment usually focuses on hormone replacement therapy. This approach helps restore normal physiological functions and alleviate symptoms. Regular monitoring is essential to adjust dosages effectively based on individual patient needs.
10.2. Central Diabetes Insipidus
Central Diabetes Insipidus (CDI) is a rare disorder characterized by an inability to concentrate urine due to insufficient production of the hormone vasopressin. This condition stems from damage to the hypothalamus or pituitary gland, often following trauma, surgery, or tumors.
Patients with CDI experience excessive thirst and urination as their kidneys struggle to retain water. As a result, they may consume large volumes of fluids in attempts to stave off dehydration.
Diagnosis typically involves water deprivation tests and measuring levels of vasopressin in the blood. Treatment usually focuses on replacing missing hormones through desmopressin, which helps regulate kidney function and reduce urinary output.
Managing Central Diabetes Insipidus requires regular monitoring and adjustments in therapy based on individual needs. Understanding this syndrome can significantly enhance patient quality of life when addressed effectively by healthcare providers.
10.3. Idiopathic Hypercalciuria
Idiopathic Hypercalciuria is a condition characterized by elevated levels of calcium in the urine without an identifiable cause. It often leads to kidney stone formation and can be quite distressing for patients.
The kidneys play a crucial role in maintaining calcium balance. When functioning normally, they excrete excess calcium efficiently. However, in cases of idiopathic hypercalciuria, this regulation fails, resulting in high urinary calcium levels.
Symptoms may include flank pain due to stones or recurrent urinary tract infections. Diagnosis typically involves urine tests that measure calcium concentration over 24 hours.
Management focuses on dietary modifications and increased fluid intake to dilute urine concentrations. In some cases, medications that lower urinary calcium excretion are prescribed. Regular follow-ups with healthcare providers are essential to monitor the condition effectively and prevent complications related to kidney health.
11. Diagnostic Challenges in Idiopathic Syndromes
Diagnosing idiopathic syndromes presents unique challenges for healthcare providers. Often, these conditions evade straightforward identification due to their elusive nature and lack of clear causative factors.
Physicians frequently rely on exclusion diagnosis methodology. This involves systematically ruling out other potential disorders before concluding a condition is idiopathic. Such an approach can be time-consuming and may lead to patient frustration.
Advanced diagnostic techniques are becoming more prevalent in this domain. Imaging studies, genetic testing, and biomarker analysis help refine the diagnostic process by providing additional insights into underlying mechanisms.
Despite technological advances, many patients still experience prolonged uncertainty regarding their diagnosis. The ongoing quest for biomarkers continues to hold promise but has yet to yield universally applicable solutions across all idiopathic syndromes. Understanding these complexities is essential for both clinicians and patients navigating the intricate landscape of unknown diagnoses.
11.1. Exclusion Diagnosis Methodology
Exclusion diagnosis methodology plays a critical role in identifying idiopathic syndromes. This approach involves ruling out other potential causes for the symptoms presented by patients. By systematically eliminating conditions with known etiologies, healthcare professionals can focus on what remains unexplained.
This process often starts with a comprehensive clinical assessment and diagnostic testing. Physicians look closely at medical history, family background, and environmental factors that might contribute to the patient’s condition.
Laboratory tests and imaging studies are commonly employed to exclude various diseases. These methods help ensure an accurate diagnosis while minimizing misinterpretation of results.
The complexity of idiopathic syndromes makes exclusion diagnosis essential. It requires careful consideration of overlapping symptomatology across different disorders. This method paves the way for better understanding and management of these elusive conditions.
11.2. Advanced Diagnostic Techniques
Advanced diagnostic techniques play a crucial role in identifying idiopathic syndromes. As these conditions often lack clear etiologies, innovative methods are essential for accurate diagnosis.
One promising approach is the use of advanced imaging technologies such as MRI and PET scans. These tools provide detailed insights into brain activity and structural changes that may indicate an underlying syndrome.
Another technique gaining traction is metabolomic profiling. This method examines metabolites in biological samples, offering a glimpse into metabolic disturbances associated with certain idiopathic conditions.
Genetic testing has also become increasingly relevant. By analyzing DNA sequences, clinicians can identify potential genetic predispositions to specific syndromes, even when symptoms are vague or absent.
Machine learning algorithms are being utilized to analyze large datasets from various sources. This technology enhances pattern recognition and aids in predicting disease trajectories based on clinical presentations and historical data.
11.3. Biomarker Research and Development
Biomarker research and development is gaining momentum in the field of idiopathic syndromes. These markers play a crucial role in understanding disease mechanisms, diagnosis, and treatment responses.
Identifying specific biomarkers can help clinicians differentiate between various idiopathic conditions. They offer insights into underlying biological processes that remain elusive through traditional diagnostic methods. As researchers delve deeper, they uncover potential links to genetic predispositions or environmental triggers.
Advancements in technology have bolstered biomarker discovery. Techniques such as genomics, proteomics, and metabolomics enable scientists to analyze complex biological samples with greater precision. This progress holds promise for more personalized approaches to treatment.
Moreover, biomarkers may assist in tracking disease progression and therapeutic effectiveness over time. By providing measurable indicators of health status or response to therapy, they pave the way for tailored interventions that enhance patient outcomes significantly.
12. Treatment Approaches for Idiopathic Syndromes
Treatment approaches for idiopathic syndromes often focus on managing symptoms rather than targeting a specific underlying cause. This can involve various strategies tailored to individual patient needs.
Symptomatic management remains a cornerstone of treatment. Patients may receive medications to alleviate pain, improve sleep, or enhance quality of life. These interventions are crucial in providing relief and restoring functionality.
Immunomodulatory therapies are also explored. These treatments aim to regulate the immune response, particularly in autoimmune-related idiopathic conditions, with varying degrees of success based on the syndrome’s nature.
Emerging experimental treatments show promise as well. Ongoing research investigates novel drugs and therapies that could potentially address the complexities associated with idiopathic syndromes more effectively than current options do.
This evolving landscape highlights the need for personalized care plans that adapt as new insights into these challenging disorders emerge.
12.1. Symptomatic Management
Symptomatic management is crucial for patients dealing with idiopathic syndromes, where the underlying cause remains elusive. This approach focuses on alleviating symptoms rather than curing the condition itself.
For instance, medications may target specific symptoms such as pain, fatigue, or inflammation. Nonsteroidal anti-inflammatory drugs (NSAIDs) are often prescribed to help manage discomfort associated with various syndromes.
Physical therapy can also play a significant role in improving mobility and function. Tailored exercise regimens enhance strength and flexibility while reducing stiffness.
Psychological support is equally important. Counseling or cognitive-behavioral therapy can provide coping strategies for managing chronic symptoms and emotional distress related to these unpredictable conditions.
Integrating lifestyle modifications—such as dietary changes and stress management techniques—can further improve quality of life for individuals living with idiopathic syndromes, promoting a holistic approach to care that addresses both physical and mental well-being.
12.2. Immunomodulatory Therapies
Immunomodulatory therapies have emerged as vital tools in managing idiopathic syndromes. These treatments aim to restore balance within the immune system, which can often be dysregulated in these conditions.
For instance, corticosteroids are commonly used to reduce inflammation and suppress overactive immune responses. This approach is beneficial for various idiopathic autoimmune disorders.
Biological agents targeting specific pathways of the immune system represent another innovative strategy. They can inhibit particular cytokines or cells involved in inflammatory processes, offering more tailored interventions.
Moreover, newer therapies like monoclonal antibodies show promise for patients who do not respond well to traditional options. By precisely modulating the immune response, these therapies provide hope for improved outcomes.
Understanding each patient’s unique immunological profile allows healthcare providers to customize treatment plans effectively. With ongoing research and innovation, immunomodulatory therapies continue evolving to address the complexities of idiopathic syndromes.
12.3. Emerging Experimental Treatments
Emerging experimental treatments for idiopathic syndromes hold promise for patients seeking relief from unexplained symptoms. Researchers are exploring various innovative approaches, including gene therapy and regenerative medicine.
Gene therapy aims to address the underlying genetic components that may contribute to these conditions. By modifying specific genes, scientists hope to alter disease progression or even reverse symptoms.
Regenerative medicine focuses on repairing damaged tissues through stem cell therapies. This approach is particularly relevant in conditions like idiopathic pulmonary fibrosis and autoimmune disorders.
Biologics, which target specific pathways in the immune system, are also being investigated. These treatments can provide tailored options that might effectively manage symptoms without broad immunosuppression.
Ongoing clinical trials continue to assess the efficacy of these emerging therapies. The future holds potential as researchers work diligently to enhance treatment modalities for those affected by idiopathic syndromes.
13. Patient Quality of Life and Psychosocial Aspects
Living with idiopathic syndromes can significantly affect a patient’s quality of life. The uncertainty surrounding these conditions often leads to anxiety and frustration. Patients may feel isolated, unsure of how to manage their symptoms or find support.
Psychosocial aspects play a vital role in coping strategies. Many individuals benefit from connecting with support groups where they share experiences and learn from one another. This support fosters resilience and helps combat feelings of loneliness.
Mental health is another crucial factor. Anxiety and depression frequently accompany chronic illness, making it essential for patients to prioritize mental well-being alongside physical health. Accessing counseling services or engaging in mindfulness practices can prove beneficial.
Furthermore, educating friends and family about these syndromes enhances understanding and empathy, creating a supportive home environment that aids recovery and emotional stability.
13.1. Coping with Diagnostic Uncertainty
Living with an idiopathic syndrome can be particularly challenging due to the uncertainty surrounding diagnosis. Patients often find themselves navigating a maze of tests and consultations, leaving them feeling frustrated and anxious.
The lack of a clear cause means that understanding their condition becomes complex. This uncertainty can lead to feelings of isolation as individuals struggle to explain their symptoms or seek validation from others.
Finding support is crucial. Many patients benefit from connecting with communities, both online and offline, where they can share experiences and coping strategies. Engaging in therapy may also provide emotional relief by helping individuals process their feelings related to the unknown.
Developing self-advocacy skills is essential too. Being informed about one’s symptoms empowers patients when communicating with healthcare providers, fostering a more collaborative relationship focused on exploration rather than mere diagnosis.
13.2. Mental Health in Idiopathic Conditions
Living with idiopathic syndromes can lead to significant mental health challenges. The uncertainty surrounding symptoms often creates anxiety and stress for patients. Without a clear diagnosis, individuals may feel isolated or misunderstood.
Many experience fluctuations in their emotional well-being due to chronic pain or fatigue. This unpredictability can impact daily life and make it difficult to maintain relationships or work commitments.
Support systems are vital. Connecting with others facing similar challenges can foster a sense of community. Therapy options, such as cognitive-behavioral therapy (CBT), have proven beneficial for managing anxiety and depression linked to these conditions.
Mindfulness practices also play an essential role in coping strategies. Techniques like meditation and deep-breathing exercises help ground patients during particularly tough moments, promoting resilience amidst the chaos of undiagnosed illnesses.
14. Research Frontiers in Idiopathic Syndromes
Research on idiopathic syndromes is rapidly evolving, focusing on uncovering the underlying mechanisms of these enigmatic conditions. Genetic and epigenetic studies are at the forefront, exploring how inherited factors contribute to susceptibility. These investigations aim to identify specific gene variations linked to various syndromes.
Another promising area involves environmental factor assessments. Researchers are examining how external elements like toxins or infections may trigger idiopathic conditions in susceptible individuals. Understanding these interactions could lead to better prevention strategies.
Systems biology approaches bring a holistic view into play by analyzing complex biological networks related to idiopathic syndromes. This method enables scientists to integrate data from multiple levels—genomic, proteomic, and metabolomic—to unravel the intricate web of factors influencing disease manifestation.
These research directions offer hope for more effective diagnostics and targeted therapies tailored specifically for patients grappling with idiopathic syndromes.
14.1. Genetic and Epigenetic Studies
Genetic and epigenetic studies are critical in understanding idiopathic syndromes. These approaches provide insights into how genetic variations may contribute to disease risk.
Researchers analyze DNA sequences to identify mutations or polymorphisms associated with specific conditions. This can lead to the discovery of potential biomarkers for diagnosis and treatment.
Epigenetics adds another layer of complexity. It examines how environmental factors influence gene expression without altering the underlying DNA sequence. Factors such as stress, diet, and toxins can modify gene activity, potentially triggering or exacerbating idiopathic disorders.
Both fields hold promise for personalized medicine. By integrating genetic data with lifestyle influences, tailored treatment strategies could emerge. Ongoing research continues to unveil intricate relationships between genetics, epigenetics, and idiopathic syndromes. These findings pave the way for innovative therapeutic options that address individual patient needs more effectively.
14.2. Environmental Factor Investigations
Environmental factors have gained significant attention in the study of idiopathic syndromes. Researchers aim to uncover how exposure to various elements may trigger or exacerbate these conditions.
Air pollution, for instance, has been linked to respiratory and neurological disorders. Investigations focus on specific pollutants and their potential roles in disease onset.
Moreover, lifestyle choices such as diet and physical activity are also under scrutiny. These factors can influence overall health and potentially contribute to the development of idiopathic conditions.
Genetic predisposition interacts with environmental exposures too. Understanding this interplay is vital for identifying at-risk populations.
Ongoing studies utilize innovative methodologies like geographic information systems (GIS). This technology helps map disease prevalence against environmental data, offering new insights into causative relationships between environment and health outcomes.
14.3. Systems Biology Approaches
Systems biology approaches are revolutionizing the understanding of idiopathic syndromes. By integrating biological data from various sources, researchers can create comprehensive models that reflect complex interactions within living systems.
These approaches utilize high-throughput technologies and computational tools to analyze large datasets. This enables scientists to identify patterns and relationships that may not be visible through traditional methods.
One key aspect is the focus on network analysis. Systems biology examines how genes, proteins, and cellular pathways interact in health and disease. This perspective helps to uncover potential underlying mechanisms of idiopathic disorders.
Furthermore, systems biology fosters collaboration across disciplines. Biologists work alongside computer scientists and bioinformaticians to interpret data more effectively. As a result, this multidisciplinary strategy holds promise for unveiling new insights into the enigmatic nature of these conditions.
15. Epidemiology of Idiopathic Syndromes
The epidemiology of idiopathic syndromes reveals intriguing patterns that warrant further investigation. Prevalence rates can vary significantly across different regions and populations. Some conditions, like Idiopathic Pulmonary Fibrosis, show increased incidence in specific demographics.
Age and sex are crucial factors influencing susceptibility to these syndromes. For instance, certain autoimmune idiopathic conditions tend to affect women more frequently than men. Meanwhile, age-related differences can affect the presentation and management of symptoms.
Geographic variations also play a role in understanding these disorders. Environmental exposures may contribute to the development or exacerbation of idiopathic syndromes in some locations compared to others.
Risk factor analysis is essential for identifying potential triggers tied to genetic predispositions or lifestyle choices. This growing body of research continues to shed light on the complexities surrounding idiopathic syndromes, emphasizing the need for tailored approaches based on population-specific data.
15.1. Prevalence and Incidence Patterns
Understanding the prevalence and incidence of idiopathic syndromes is vital for healthcare professionals and researchers. These conditions can vary widely in their occurrence across different populations.
Research indicates that some idiopathic syndromes, like Irritable Bowel Syndrome (IBS), affect a significant portion of the adult population. Estimates suggest prevalence rates can range from 10% to 15%. Others, such as Idiopathic Pulmonary Fibrosis (IPF), are less common but still impactful, with incidence rates around 3 per 100,000 individuals annually.
Geographical factors also play a role in these patterns. Certain autoimmune idiopathic conditions may show higher prevalence in specific regions due to environmental triggers or genetic predispositions.
Age is another critical factor influencing these syndromes’ incidence. Many conditions emerge during adulthood but have manifestations that begin earlier or later in life, further complicating understanding their true impact on public health.
15.2. Demographic and Geographic Variations
Demographic and geographic variations play a critical role in understanding idiopathic syndromes. These conditions can manifest differently across various populations, influenced by factors like age, sex, ethnicity, and lifestyle.
For instance, certain idiopathic disorders may show higher prevalence rates in specific ethnic groups. This highlights the importance of cultural awareness in diagnosis and treatment.
Geographically, environmental influences such as climate or pollution levels can contribute to differences in syndrome occurrence. Urban areas might exhibit varying patterns compared to rural settings due to lifestyle habits and healthcare access.
Age also significantly impacts these syndromes. Children might experience different symptoms than adults facing similar conditions. Monitoring these variations is essential for developing targeted interventions that address the unique needs of affected communities effectively. Recognizing these dynamics aids researchers and clinicians alike in improving patient outcomes across diverse populations.
15.3. Risk Factor Analysis
Risk factor analysis in idiopathic syndromes is crucial for understanding these complex conditions. Identifying potential risk factors can help researchers and healthcare providers develop preventive strategies.
Genetic predisposition plays a significant role. Certain inherited traits may increase susceptibility to various idiopathic syndromes. Family history often points to patterns that warrant further investigation.
Environmental influences are another key aspect. Exposure to toxins, allergens, or infections can trigger symptoms in genetically predisposed individuals. This highlights the need for comprehensive studies examining environmental interactions.
Lifestyle choices also contribute significantly to risk profiles. Factors such as diet, exercise, and stress management can affect disease onset and progression.
By analyzing these elements, researchers strive to create a clearer picture of how different variables interact within idiopathic syndromes. This information could lead to better-targeted therapies and improved patient outcomes over time.
16. Pathophysiological Theories in Idiopathic Syndromes
Pathophysiological theories in idiopathic syndromes explore the underlying mechanisms of these mysterious conditions. One prominent hypothesis involves autoimmune responses, where the body mistakenly targets its own tissues. This theory is supported by observed markers of inflammation in various idiopathic disorders.
Neurodegenerative models also contribute to understanding these syndromes. They suggest that disruptions in neuronal communication might play a role in conditions like Chronic Fatigue Syndrome and Restless Legs Syndrome. Such disruptions can lead to symptoms that significantly impact daily life.
Metabolic dysfunction theories propose alterations in metabolic pathways may be at play as well. Conditions such as Idiopathic Pulmonary Fibrosis may involve changes in cellular metabolism, affecting tissue repair processes and leading to progressive disease states.
Research continues to evolve, shedding light on these complex interactions within the body, paving the way for more effective treatment strategies for those affected by idiopathic syndromes.
16.1. Autoimmune Hypotheses
Autoimmune hypotheses suggest that idiopathic syndromes may arise from the body’s immune system mistakenly attacking its own tissues. This misdirected response can lead to inflammation and damage, contributing to a variety of unexplained symptoms.
Research indicates that certain genetic factors might predispose individuals to these autoimmune reactions. These are often triggered by environmental influences or infections, complicating the understanding of idiopathic conditions.
In many cases, patients present with a collection of signs and symptoms without a clear diagnostic path. The challenge lies in pinpointing whether an autoimmune process is at play when traditional markers of autoimmunity do not yield definitive results.
This area remains active in research as scientists explore how immune dysregulation could be linked to various idiopathic disorders. Understanding these connections may one day shed light on effective treatment strategies for those affected by these complex syndromes.
16.2. Neurodegenerative Models
Neurodegenerative models offer crucial insights into idiopathic syndromes. These models help researchers understand how certain conditions develop and progress in the nervous system.
For instance, Alzheimer’s disease and Parkinson’s disease have been studied extensively to identify common pathways of neurodegeneration. Such studies often reveal underlying mechanisms that may also apply to idiopathic syndromes with neurological components.
In many cases, these models highlight the role of protein misfolding and aggregation—common features seen across various disorders. This understanding fosters a better grasp of potential therapeutic targets.
Additionally, neuroinflammation is another critical area examined within these frameworks. It provides evidence suggesting that immune responses could contribute to neuronal damage in idiopathic conditions.
By leveraging findings from established neurodegenerative diseases, scientists seek innovative ways to diagnose and treat more obscure idiopathic syndromes effectively.
16.3. Metabolic Dysfunction Theories
Metabolic dysfunction theories suggest that disturbances in metabolism play a crucial role in the development of various idiopathic syndromes. These theories focus on how cellular and systemic metabolic processes can lead to unexplained symptoms.
Researchers are exploring how altered energy production, nutrient utilization, and waste elimination contribute to these conditions. For instance, mitochondrial dysfunction may disrupt energy supply in cells, leading to fatigue and other health issues commonly reported by patients.
Additionally, imbalances in hormones or metabolites could trigger inflammatory responses within the body. This inflammation might exacerbate existing symptoms or initiate new ones without any identifiable cause.
Investigating metabolic pathways offers potential avenues for treatment. By understanding these underlying mechanisms, healthcare providers can better address patient needs with targeted strategies tailored to individual metabolic profiles.
17. Imaging and Biomarkers in Idiopathic Syndromes
Advancements in imaging techniques are transforming our understanding of idiopathic syndromes. Methods like MRI and PET scans provide detailed insights into brain structure and function. These tools help identify abnormalities that may contribute to symptoms, even when the underlying cause remains unknown.
Biomarkers offer another layer of exploration in these conditions. Researchers are investigating molecular signatures that could indicate specific idiopathic disorders. By analyzing blood samples or tissue biopsies, scientists hope to uncover patterns associated with various syndromes.
This combination of advanced imaging and biomarker research holds promise for earlier diagnosis and targeted treatments. As discoveries unfold, it becomes increasingly clear how crucial these approaches are in unraveling the complexities surrounding idiopathic syndromes. Enhanced detection methods can pave the way for more personalized care tailored to individual patient needs.
17.1. Advanced Neuroimaging Techniques
Advanced neuroimaging techniques are revolutionizing the understanding of idiopathic syndromes. These methods provide detailed insights into brain structure and function.
Functional Magnetic Resonance Imaging (fMRI) allows researchers to observe brain activity in real-time. By detecting changes in blood flow, fMRI reveals how different areas of the brain communicate during various tasks.
Positron Emission Tomography (PET) offers another layer of depth by visualizing metabolic processes. This technique can highlight abnormal activity patterns associated with neurological disorders, aiding in the identification of underlying causes for conditions that were previously deemed idiopathic.
Diffusion Tensor Imaging (DTI), a specialized form of MRI, maps white matter tracts within the brain. It provides valuable information about connectivity and integrity, helping to uncover potential disruptions related to unexplained symptoms.
These advanced neuroimaging approaches are essential for unraveling complex idiopathic syndromes and paving the way for targeted interventions.
17.2. Molecular and Genetic Biomarkers
Molecular and genetic biomarkers play a crucial role in understanding idiopathic syndromes. These markers provide insights into the underlying biological processes involved in various conditions.
By analyzing DNA, RNA, or proteins, researchers can identify specific changes associated with certain syndromes. This information helps in distinguishing idiopathic cases from those with known causes.
For instance, genetic testing may reveal mutations that predispose individuals to specific disorders. Similarly, molecular profiling can shed light on inflammatory responses linked to autoimmune conditions.
The development of these biomarkers is essential for advancing personalized medicine. Tailoring treatments based on an individual’s unique biomarker profile improves outcomes and enhances therapeutic strategies.
Current research continues to explore novel biomarkers across different idiopathic syndromes. This growing body of knowledge holds promise for improved diagnosis and management in the future.
17.3. Metabolomic Profiling
Metabolomic profiling is a cutting-edge approach that analyzes metabolites in biological samples. It provides insights into the metabolic state of an individual, revealing how various conditions affect metabolism.
In idiopathic syndromes, this technique can identify unique biomarkers related to disease processes. By comparing metabolite profiles between affected individuals and healthy controls, researchers can uncover potential pathways involved in these complex disorders.
This method facilitates early detection and may guide treatment decisions tailored to the patient’s specific metabolic responses. As technology advances, metabolomic profiling holds promise for improving our understanding of idiopathic conditions.
Integrating this data with other omics approaches could pave the way for personalized medicine. The goal is to create targeted therapies based on an individual’s unique biochemical landscape, enhancing therapeutic efficacy while minimizing side effects.
18. Clinical Trials and Research Ethics
Clinical trials for idiopathic syndromes present unique challenges. Researchers often struggle to design studies that yield meaningful results, particularly due to the vague nature of these conditions.
One significant issue is participant recruitment. Many patients with idiopathic disorders may feel uncertain about entering a study when their diagnosis lacks clarity. This can lead to underrepresentation in clinical trials.
Ethical considerations also play a crucial role. Informed consent is vital, especially since many participants are already navigating complex health issues. Ensuring they understand potential risks and benefits is paramount.
Placebo use raises additional ethical dilemmas in these cases. Patients might worry about receiving no treatment while dealing with poorly understood conditions, which complicates trial acceptance among this vulnerable population.
Balancing scientific rigor and ethical responsibility remains essential as researchers seek innovative solutions for idiopathic syndromes through well-structured clinical trials.
18.1. Challenges in Designing Clinical Trials
Designing clinical trials for idiopathic syndromes presents unique challenges. The primary hurdle is the lack of a clear understanding of these conditions’ underlying mechanisms. Without established etiologies, researchers struggle to identify suitable endpoints and outcome measures.
Moreover, patient recruitment can be difficult due to the diverse nature of symptoms associated with idiopathic syndromes. Many individuals may not receive timely diagnoses or might be misclassified under other disorders.
Another significant challenge involves ethical considerations. Informed consent becomes complex when patients have vague or unknown prognoses related to their conditions. Researchers must ensure that participants understand potential risks and benefits without overwhelming them with uncertainty.
Funding is also crucial yet challenging to secure, as many idiopathic syndromes are less understood compared to more common diseases. This poses limitations on resources available for comprehensive studies aimed at discovering effective treatments or management strategies.
18.2. Placebo Use in Idiopathic Syndrome Studies
Placebo use in idiopathic syndrome studies raises important ethical considerations. Researchers often include a placebo group to assess the effectiveness of new treatments. This helps determine if changes in symptoms are due to the treatment or simply a result of psychological factors.
Patients with idiopathic syndromes frequently experience uncertainty about their condition, which can influence their response to treatment. The expectation of improvement can lead to significant symptom relief even when no active medication is taken.
However, using a placebo must be carefully considered. Informed consent is crucial, as patients should understand the potential for receiving a non-active treatment instead of an actual intervention. Balancing scientific rigor with patient well-being becomes critical in this context.
Researchers strive for transparency and ethical integrity while designing these studies, ensuring that participants are adequately informed about what they might experience during clinical trials involving placebos.
19. Personalized Medicine in Idiopathic Syndromes
Personalized medicine is transforming how idiopathic syndromes are approached. By focusing on the unique genetic makeup of each patient, treatments can be tailored to individual needs. This approach enhances efficacy and minimizes side effects.
Pharmacogenomics plays a crucial role in this strategy. It studies how genes affect a person’s response to medications. Understanding these variations allows healthcare providers to select therapies that align with a patient’s specific biological profile.
Moreover, personalized treatment plans consider lifestyle factors and environmental influences. This comprehensive view ensures more effective management of symptoms associated with idiopathic conditions.
As research continues to evolve, the integration of advanced technologies will refine these approaches even further. Patients may soon benefit from targeted therapies designed specifically for their unique health scenarios, leading to improved outcomes and quality of life.
19.1. Tailoring Treatments to Individual Patients
Personalized medicine is revolutionizing the approach to treating idiopathic syndromes. Each patient presents a unique puzzle, and tailored treatments can lead to better outcomes.
Physicians now consider genetic, environmental, and lifestyle factors when designing treatment plans. This individualized strategy moves beyond a one-size-fits-all model, enabling more effective interventions.
For example, understanding how specific medications interact with a patient’s genetic makeup can enhance efficacy while minimizing side effects. Pharmacogenomics plays an essential role in this process by analyzing variations in genes that affect drug metabolism.
Additionally, ongoing monitoring allows for adjustments based on patient responses. This dynamic approach ensures that the treatment evolves alongside the patient’s condition.
Tailoring treatments not only addresses symptoms but also empowers patients through involvement in their healthcare journey. By prioritizing individuality within medical care, providers foster improved quality of life for those facing idiopathic syndromes.
19.2. Pharmacogenomics in Idiopathic Conditions
Pharmacogenomics plays a crucial role in the treatment of idiopathic syndromes. This field studies how an individual’s genetic makeup influences their response to medications. For patients with idiopathic conditions, understanding these genetic factors can lead to more effective therapies.
By analyzing specific genes, healthcare providers can identify which drugs are likely to work best for a patient. This approach minimizes trial-and-error prescribing and reduces the risk of adverse drug reactions.
For instance, certain genetic variations may affect drug metabolism rates. By knowing this information, physicians can tailor dosages that optimize therapeutic outcomes while minimizing side effects.
As research advances, pharmacogenomic testing is becoming more accessible. With ongoing studies focusing on various idiopathic disorders, there’s potential for personalized medicine to revolutionize care in this area and improve patient experiences significantly.
20. Pediatric Idiopathic Syndromes
Pediatric idiopathic syndromes present unique challenges in diagnosis and management. These conditions often emerge during crucial developmental stages, making early detection essential.
Children may exhibit symptoms that are puzzling to healthcare providers. Idiopathic features can lead to delays in appropriate treatment. Parents might feel overwhelmed as they navigate this uncertainty.
Developmental considerations play a significant role. Symptoms in children can differ from adults, requiring specialized knowledge for accurate assessments. Some syndromes may evolve or change presentation over time.
Long-term follow-up is vital for pediatric patients with idiopathic conditions. Transitioning care into adulthood poses its own set of challenges, including continuity of treatment and support systems.
Research continues to explore the genetic underpinnings and environmental influences on these syndromes. Understanding these factors could pave the way for tailored therapies aimed at improving outcomes for young patients.
20.1. Developmental Considerations
When addressing pediatric idiopathic syndromes, developmental considerations play a crucial role. Children experience rapid physical and cognitive growth, making it essential to monitor their unique needs closely.
The manifestation of symptoms can often differ significantly from adults. This variation complicates diagnosis and may lead to delays in treatment. Parents should be vigilant about changes in behavior or development that seem unusual.
Additionally, the psychosocial aspect cannot be overlooked. Children with unexplained health issues may struggle with emotional well-being due to uncertainty around their condition. Engaging with supportive networks can help alleviate some anxiety.
Healthcare providers must adopt a holistic approach when evaluating children for idiopathic syndromes. Regular assessments will ensure that any emerging challenges are addressed promptly, paving the way for healthier futures as they transition into adulthood.
20.2. Long-term Follow-up and Transition to Adult Care
Transitioning from pediatric to adult care can be a challenging journey for patients with idiopathic syndromes. This shift often occurs during adolescence, a time filled with personal development and change.
Young adults may feel overwhelmed by the responsibility of managing their health independently. They must become familiar with new healthcare providers and protocols in an adult setting.
It’s crucial for parents and caregivers to facilitate this transition. Supporting young people in understanding their conditions fosters confidence as they navigate medical appointments alone.
Establishing effective communication between pediatricians and adult specialists is vital. A collaborative approach ensures continuity of care, minimizing disruptions that could affect treatment plans.
Patients should also advocate for themselves during this phase, asking questions about treatments or lifestyle adjustments essential for their well-being. By actively participating in their own healthcare decisions, these individuals can lay the groundwork for healthier futures.
21. Geriatric Aspects of Idiopathic Syndromes
Geriatric patients often present unique challenges when it comes to idiopathic syndromes. Age-related physiological changes can alter the way these conditions manifest and progress. For example, symptoms may be more subtle or masked by other age-related disorders.
Polypharmacy is another concern in older adults. Many geriatric patients take multiple medications, which complicates diagnosis and treatment of idiopathic syndromes. Interactions between drugs can also exacerbate or mimic syndrome symptoms.
Additionally, comorbidities are prevalent in this population. Conditions like hypertension or diabetes can interfere with the management of idiopathic syndromes, requiring a comprehensive approach tailored to individual needs.
Long-term follow-up becomes crucial for older individuals with these conditions. Regular monitoring helps address any complications that arise as they navigate their health journey through aging while dealing with unexplained medical issues.
21.1. Age-Related Changes in Presentation
As people age, the presentation of idiopathic syndromes can change significantly. Older adults may exhibit symptoms differently than younger patients due to various physiological changes.
For instance, neurological disorders might manifest with more subtle signs in seniors. Cognitive decline or memory issues could overshadow initial symptoms, making diagnosis challenging.
Additionally, chronic pain conditions like fibromyalgia may be perceived as normal aging discomfort. This misinterpretation can delay proper treatment and management.
Moreover, comorbidities common in older populations often complicate the clinical picture. These additional health concerns can mask or mimic idiopathic syndrome symptoms.
It’s vital for healthcare providers to recognize these age-related nuances during assessment and diagnosis. Understanding how idiopathic syndromes present differently in geriatric patients ensures that they receive appropriate care tailored to their unique needs.
21.2. Polypharmacy and Comorbidity Management
Managing idiopathic syndromes in geriatric patients requires a nuanced understanding of their unique needs. Many elderly individuals often present with multiple health conditions, leading to what is known as polypharmacy—the concurrent use of several medications.
This complexity can pose significant challenges for both the patient and healthcare providers. Each additional medication increases the risk of side effects and interactions, which may worsen existing symptoms or introduce new ones. Therefore, careful assessment is crucial to ensure that treatments are not only effective but also safe.
Geriatric care must prioritize comprehensive evaluations that consider all aspects of an individual’s health status. This includes regular reviews of prescribed medications and maintaining open lines of communication between different specialists involved in a patient’s care.
Effective management strategies might involve simplifying medication regimens where possible while still addressing each individual’s diverse medical issues adequately. Personalized treatment plans should focus on optimizing quality of life rather than solely targeting disease-specific outcomes.
By recognizing the complexities associated with aging and idiopathic syndromes, healthcare professionals can better navigate these challenges, ultimately improving patient outcomes and enhancing overall well-being for this vulnerable population.


