Mayer-Rokitansky-Küster-Hauser syndrome, often referred to as MRKH, is a rare condition that affects the development of the female reproductive system. For those diagnosed with this syndrome, understanding its implications can be overwhelming. This guide aims to unravel the complexities surrounding MRKH and provide insight into its clinical presentation, diagnosis, and treatment options.
As we delve deeper into this topic, we’ll explore not just the medical aspects but also the emotional and psychological challenges faced by individuals navigating life with MRKH. From genetic factors to innovative research in regenerative medicine, our comprehensive overview will empower readers with knowledge and resources. Whether you are seeking information for yourself or supporting someone else on their journey, this guide is designed to inform and inspire hope in those affected by Mayer-Rokitansky-Küster-Hauser syndrome.
Mayer-Rokitansky-Küster-Hauser Syndrome: Understanding Müllerian Agenesis
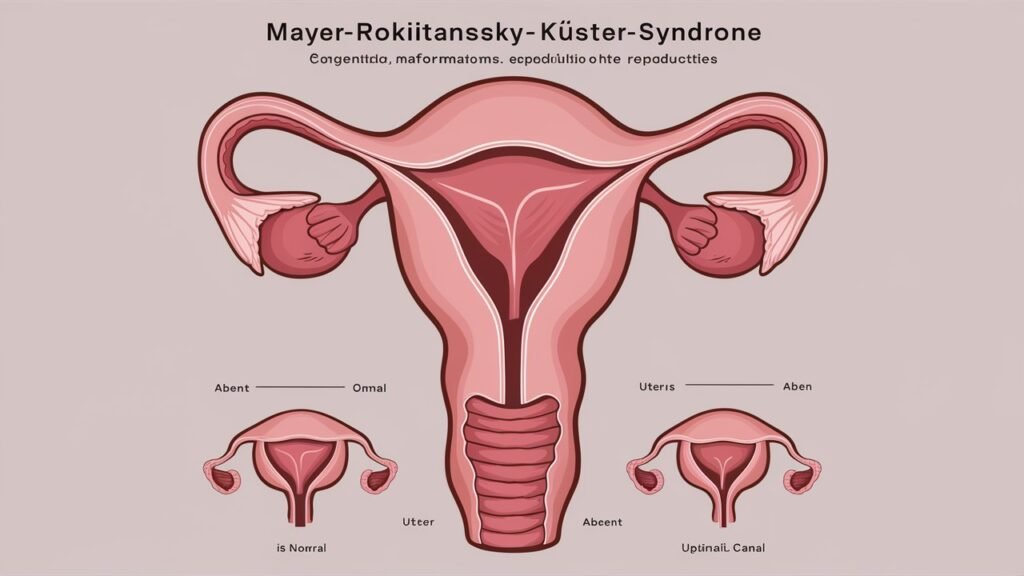
Mayer-Rokitansky-Küster-Hauser syndrome (MRKH) is primarily characterized by Müllerian agenesis, where the uterus and upper two-thirds of the vagina fail to develop. This condition affects individuals assigned female at birth and can lead to primary amenorrhea, as menstruation does not occur without a uterine structure.
While external genitalia are typically normal, MRKH often results in various physical and emotional challenges for those affected. The absence of reproductive organs can impact self-image, leading to feelings of isolation or confusion regarding identity.
“How Does Nager Syndrome Impact Facial Development?”
Understanding MRKH requires awareness of its impact on fertility and body autonomy. Individuals with this syndrome may explore options such as surrogacy or adoption when they wish to build families of their own.
Embryological Basis: Development of the Female Reproductive Tract
The development of the female reproductive tract is a complex process that begins during embryogenesis. This intricate system originates from the Müllerian ducts, which appear around six weeks of gestation. These paired structures play a crucial role in forming key components such as the uterus, fallopian tubes, and upper two-thirds of the vagina.
During fetal development, if there are disruptions in Müllerian duct formation or fusion, it can lead to conditions like Mayer-Rokitansky-Küster-Hauser syndrome. The complete or partial absence of these structures results in primary amenorrhea and vaginal agenesis.
“What Are The Signs of Nance-Horan Syndrome?”
Understanding this developmental pathway is vital for grasping how MRKH syndrome arises. It emphasizes the significance of early embryological events in defining female anatomy and reproductive capabilities.
Genetic Factors: Current Understanding and Ongoing Research
Research into Mayer-Rokitansky-Küster-Hauser syndrome (MRKH) has identified genetic factors that may contribute to its development. Studies suggest a potential link to variations in certain genes associated with the Müllerian duct’s formation during embryonic development. For instance, mutations in the WNT4 gene have been implicated.
Ongoing research is focusing on identifying additional genetic markers and pathways involved in MRKH. Researchers are also examining familial patterns, as some cases appear hereditary, hinting at an underlying genetic predisposition.
“Why Does Nephrotic Syndrome Cause Protein Loss?”
Advanced genomic techniques like whole-exome sequencing offer promising avenues for understanding MRKH more comprehensively. These methods could lead to breakthroughs in diagnosis and personalized treatment strategies for individuals affected by this condition.
Clinical Presentation: Primary Amenorrhea and Vaginal Agenesis
Mayer-Rokitansky-Küster-Hauser Syndrome primarily manifests through two significant clinical features: primary amenorrhea and vaginal agenesis. Individuals often experience the absence of menstruation by their late teens, which can be a source of confusion and distress.
Vaginal agenesis refers to the underdevelopment or absence of the vagina. This condition is not necessarily linked to other physical traits, making diagnosis challenging. Many females are unaware they have MRKH until they seek evaluation for absent periods or fertility concerns.
“How Does Nail-Patella Syndrome Affect Development?”
The psychological impact can be profound as patients navigate feelings about their bodies and reproductive health. Understanding these symptoms is crucial for timely diagnosis and management, offering paths toward support and treatment options tailored to individual needs.
Associated Congenital Anomalies: Renal and Skeletal Involvement
Mayer-Rokitansky-Küster-Hauser syndrome often presents with various associated congenital anomalies, particularly involving the renal and skeletal systems. Approximately 30-50% of individuals with MRKH experience renal abnormalities. These may include unilateral renal agenesis or ectopic kidneys, which can complicate overall health management.
Skeletal anomalies are also notable in MRKH patients. Conditions such as scoliosis and other vertebral malformations occur more frequently among those affected by this syndrome. This highlights the importance of comprehensive evaluations during diagnosis.
“What Causes Nasal Glioma Syndrome in Infants?”
Early identification of these associated conditions is crucial for effective treatment planning. Regular monitoring can help address potential complications and improve quality of life for those living with Mayer-Rokitansky-Küster-Hauser syndrome.
Diagnosis: Imaging Techniques and Hormonal Evaluation
Diagnosis of Mayer-Rokitansky-Küster-Hauser syndrome typically involves a combination of imaging techniques and hormonal evaluations. Ultrasound is often the first-line tool, allowing doctors to visualize the absence of the uterus and assess ovarian presence.
Magnetic resonance imaging (MRI) can provide detailed images, confirming anatomical anomalies in the reproductive tract. It helps identify associated renal or skeletal abnormalities that may accompany MRKH.
“Why Does Neurocutaneous Melanosis Syndrome Occur?”
Hormonal evaluation plays a crucial role too. Doctors measure hormone levels to assess ovarian function. An elevated level of luteinizing hormone (LH) alongside low estrogen can indicate primary amenorrhea due to Müllerian agenesis. Together, these diagnostic methods form a comprehensive approach for effective assessment and management of MRKH syndrome.
Psychological Impact: Body Image and Gender Identity Considerations
Mayer-Rokitansky-Küster-Hauser syndrome can significantly impact a person’s body image and gender identity. Many individuals face challenges in accepting their bodies, particularly when they are aware of anatomical differences from peers. This discrepancy can lead to feelings of inadequacy or shame.
Gender identity is also influenced by the condition. Some may struggle with societal expectations regarding femininity and reproductive roles, leading to confusion about their own identity. The absence of certain physical attributes often tied to female experiences complicates this further.
“How Does Sleep Apnea Syndrome Affect Your Health?”
Support from mental health professionals is crucial for those affected by MRKH syndrome. Therapy can foster acceptance and help navigate the emotional complexities surrounding body image and gender identity, promoting healthier self-esteem and overall well-being.
Treatment Options: Non-surgical and Surgical Approaches
Treatment options for Mayer-Rokitansky-Küster-Hauser syndrome vary based on individual needs. Non-surgical approaches often include hormone replacement therapy to address the absence of menstruation and promote secondary sexual characteristics. This can help alleviate some physical symptoms and improve overall well-being.
For those seeking a more permanent solution, surgical interventions may be considered. Surgical methods aim to create a functional vagina, which can enhance sexual function and quality of life. Techniques such as vaginoplasty use donor tissue or biological materials to construct a neovagina.
The choice between non-surgical and surgical treatment is deeply personal. Patients should consult with healthcare providers specializing in MRKH syndrome to explore tailored solutions that align with their unique situations and preferences.
Vaginal Dilation Therapy: Techniques and Success Rates
Vaginal dilation therapy is a primary treatment for individuals with Mayer-Rokitansky-Küster-Hauser syndrome. This non-surgical method involves using graduated dilators to gradually expand the vaginal canal. Regular use of these dilators helps create and maintain vaginal depth, which can enhance both physical comfort and intimate relationships.
The success rates of vaginal dilation therapy are encouraging. Many patients achieve adequate vaginal depth within several months of consistent practice. Success can vary based on individual factors such as age and adherence to the regimen.
Patients often report positive outcomes in terms of sexual function and self-esteem following dilation therapy. Support from healthcare providers plays a crucial role in helping individuals navigate this process effectively.
Surgical Creation of Neovagina: Methods and Outcomes
Surgical creation of a neovagina is an option for those with Mayer-Rokitansky-Küster-Hauser syndrome. Various methods exist, including the McIndoe procedure and the Davydov technique. Each approach aims to provide functional vaginal depth while minimizing complications.
The McIndoe method involves using skin grafts to create a vaginal canal, ensuring adequate blood supply for healing. Meanwhile, the Davydov technique utilizes rectus abdominis muscle flaps, offering additional support and stability.
Outcomes vary among individuals but are generally positive. Many patients report satisfaction with their neovagina in terms of both function and aesthetics. Surgical intervention can significantly enhance quality of life by addressing physical concerns and improving sexual health options.
Reproductive Options: Surrogacy and Uterine Transplantation
For those with Mayer-Rokitansky-Küster-Hauser syndrome seeking to build a family, reproductive options include surrogacy and uterine transplantation. Surrogacy allows individuals to have a biological connection through their eggs or partner’s sperm while utilizing another woman’s uterus for gestation.
Uterine transplantation is an emerging option that enables women born without a functional uterus to carry their own pregnancies. This procedure involves transplanting a donor uterus, which can be from living or deceased donors.
While both methods present unique challenges, they offer hope for parenthood. Each choice requires thorough consideration of ethical, medical, and emotional factors before embarking on the journey toward family building.
Ovarian Function and Hormone Replacement Therapy
Ovarian function in individuals with Mayer-Rokitansky-Küster-Hauser syndrome is typically preserved, even when the uterus and vagina are absent. This means that while menstruation does not occur, ovarian hormones like estrogen and progesterone are still produced.
Hormone replacement therapy (HRT) becomes essential for managing symptoms related to estrogen deficiency. Symptoms may include hot flashes, mood swings, and vaginal dryness. HRT can help regulate these hormonal imbalances effectively.
Doctors often recommend initiating HRT around the age of expected menarche to support physical development and emotional well-being. This treatment enables those affected by MRKH to maintain a healthier quality of life as they navigate their unique reproductive challenges.
Long-term Health Implications of MRKH Syndrome
Women with Mayer-Rokitansky-Küster-Hauser syndrome may face various long-term health implications. One area of concern is renal function, as approximately 30-50% of patients have associated kidney anomalies. Regular monitoring is crucial to identify any potential complications early.
Bone density can also be affected due to hormonal imbalances linked with MRKH. Estrogen deficiency might lead to osteoporosis and increase fracture risks later in life, making it essential for medical professionals to address these concerns proactively.
Additionally, psychological aspects are significant; many women experience anxiety or depression related to body image and reproductive choices. Mental health support plays a vital role in managing these feelings and enhancing overall well-being throughout their lives.
Sexuality and Relationships: Addressing Intimate Concerns
Navigating sexuality and relationships can be particularly challenging for those with Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. Individuals may grapple with feelings of inadequacy or fear of rejection due to their unique anatomy. Open communication with partners is essential in fostering understanding and intimacy.
Many MRKH patients find that discussing their condition can reduce anxiety surrounding sexual experiences. Building trust allows couples to explore alternative ways to connect physically and emotionally, which can enhance the relationship dynamics.
Additionally, seeking support from therapists familiar with MRKH can provide invaluable insights. These professionals help individuals address intimate concerns while promoting self-acceptance and healthy relational patterns, leading to more fulfilling connections.
Genetic Counseling: Implications for Family Planning
Genetic counseling plays a crucial role for individuals with Mayer-Rokitansky-Küster-Hauser syndrome, especially regarding family planning. It helps prospective parents understand the genetic aspects of MRKH and its potential inheritance patterns.
During these sessions, counselors provide information on risks associated with having children. They discuss options such as surrogacy or adoption if natural conception is not feasible due to anatomical differences.
Counselors also guide patients through available reproductive technologies like uterine transplantation, which could open new possibilities for motherhood. This support ensures that families can make informed decisions tailored to their unique circumstances.
Quality of Life: Emotional and Social Challenges
Living with Mayer-Rokitansky-Küster-Hauser syndrome (MRKH) presents unique emotional and social challenges. Many individuals experience feelings of isolation, confusion, and anxiety regarding their body image. The absence of a uterus can lead to concerns about femininity and societal expectations.
Social interactions may also be affected. Questions about relationships, dating, and intimacy can create barriers in connecting with others. The fear of judgment or misunderstanding often complicates these experiences further.
Support networks become crucial for navigating these challenges. Connecting with peers who understand MRKH fosters a sense of belonging and provides vital emotional support. Open discussions about feelings can empower those affected to embrace their identities while addressing the complexities surrounding this condition.
Support Groups and Peer Counseling for MRKH Patients
Support groups play a crucial role for individuals with Mayer-Rokitansky-Küster-Hauser syndrome. They offer a safe space to share experiences and feelings, fostering understanding among peers. The sense of community can alleviate feelings of isolation often felt by those affected.
Peer counseling provides additional support through one-on-one interactions. Individuals who have navigated similar challenges can offer guidance and encouragement. This personalized approach can be immensely beneficial in addressing emotional concerns.
Many organizations focus on MRKH awareness and support networks, connecting patients globally. These resources empower individuals to advocate for themselves while building relationships within the community. Engaging with others facing similar journeys fosters resilience and hope for a fulfilling life ahead.
Latest Research: Tissue Engineering and Regenerative Medicine Approaches
Recent advancements in tissue engineering and regenerative medicine offer promising avenues for those affected by Mayer-Rokitansky-Küster-Hauser syndrome. Researchers are exploring innovative methods to create functional vaginal tissues using stem cells. These developments aim to enhance surgical outcomes and improve the quality of life for individuals with MRKH.
Emerging techniques utilize 3D bioprinting, which allows precise modeling of biological structures. This technology has the potential to develop personalized grafts tailored specifically for patients’ needs. Additionally, studies on bioengineered scaffolds show promise in supporting tissue regeneration.
As research progresses, it is crucial for patients to stay informed about new treatment options and participate in clinical trials when possible. Collaboration between scientists, healthcare providers, and advocates will continue driving progress in this field. The future holds hope not only for improved medical interventions but also enhanced emotional well-being for those impacted by MRKH syndrome.