Kelley-Seegmiller Syndrome is a rare genetic disorder that often goes unnoticed, yet it can significantly impact the lives of those affected. Characterized by a deficiency in the enzyme hypoxanthine-guanine phosphoribosyltransferase (HPRT), this condition disrupts purine metabolism and leads to various health challenges. Understanding Kelley-Seegmiller Syndrome is crucial for patients, families, and healthcare providers alike.
As we delve deeper into its biochemical basis, genetics, and clinical spectrum, you’ll discover not only what this syndrome entails but also how to manage its unique complications. With insights into neurological manifestations and renal issues, along with treatment options available today, our aim is to provide an informative resource for anyone impacted by or interested in Kelley-Seegmiller Syndrome. Join us as we break down the complexities of this condition and explore pathways toward better management and support.
Kelley-Seegmiller Syndrome: Understanding the HPRT Deficiency
Kelley-Seegmiller Syndrome arises from a deficiency of the enzyme hypoxanthine-guanine phosphoribosyltransferase (HPRT). This crucial enzyme is involved in purine metabolism, which plays a vital role in DNA and RNA synthesis. Without adequate HPRT activity, purines cannot be recycled effectively.
The resulting metabolic disruption leads to an accumulation of uric acid in the body. High levels of uric acid can cause various health problems, including kidney stones and gouty arthritis. The severity of symptoms varies among individuals due to differing degrees of enzyme deficiency.
“What Causes Eisenmenger Syndrome? Heart Defect Guide”
Understanding this syndrome is essential for early diagnosis and intervention. Awareness can lead to better management strategies tailored to each patient’s needs.
Biochemical Basis: Purine Metabolism and Its Disruption
Kelley-Seegmiller Syndrome arises from a deficiency in the enzyme hypoxanthine-guanine phosphoribosyltransferase (HPRT). This enzyme plays a crucial role in purine metabolism, which is essential for producing nucleotides. Nucleotides are vital building blocks for DNA and RNA.
“Why Does Facet Syndrome Cause Back Pain? Complete Guide”
When HPRT activity is low or absent, it disrupts the salvage pathway of purines. This leads to an accumulation of uric acid as purines are broken down into xanthine and hypoxanthine instead. Increased uric acid levels can result in various complications.
The disruption in this metabolic pathway has far-reaching effects on health. It not only impacts renal function but also affects neurological development and overall well-being. Understanding these biochemical mechanisms helps guide treatment strategies effectively.
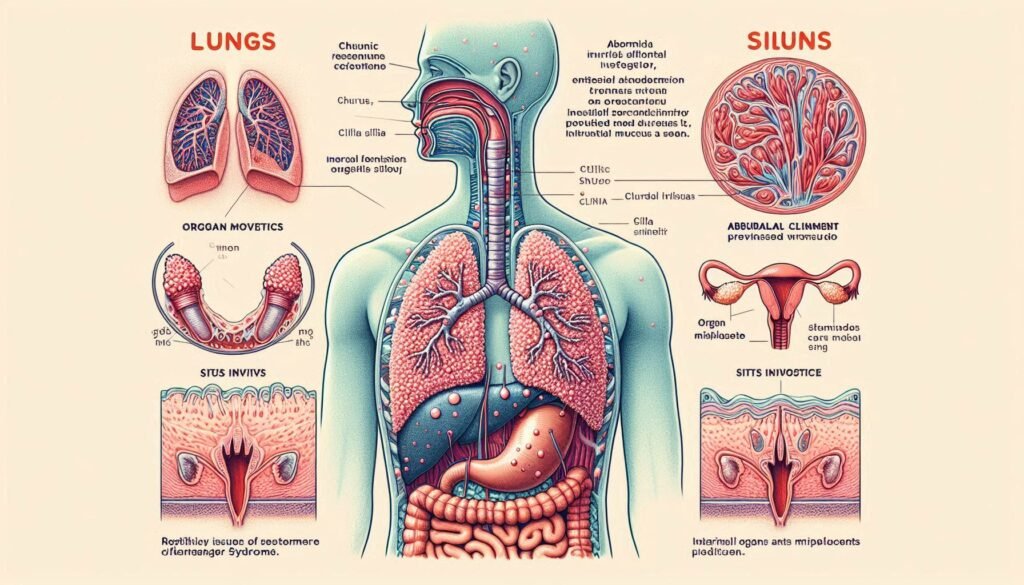
Genetics of Kelley-Seegmiller Syndrome: X-Linked Inheritance Pattern
Kelley-Seegmiller Syndrome (KSS) is primarily caused by mutations in the HPRT1 gene, which is located on the X chromosome. This genetic alteration leads to a deficiency in hypoxanthine-guanine phosphoribosyltransferase (HPRT), essential for purine metabolism.
“What Is Fazio-Londe Syndrome? Understanding Motor Neuron Disease”
Due to its X-linked inheritance pattern, KSS predominantly affects males. Females may be carriers and can exhibit mild symptoms or remain asymptomatic. The severity of the condition often correlates with the degree of HPRT enzyme function present.
In affected males, one mutated copy of the gene results in significant biochemical disruptions. Understanding this inheritance pattern aids family planning and genetic counseling for those at risk.
Clinical Spectrum: From Mild to Severe Presentations
Kelley-Seegmiller Syndrome presents a diverse range of clinical manifestations. Some individuals experience mild symptoms, which may include subtle behavioral issues or occasional joint discomfort. These patients often lead relatively normal lives with few health complications.
“How Does Femoral Acetabular Impingement Affect Hip Movement?”
Conversely, others face severe presentations that significantly impact daily functioning. Severe cases can involve profound cognitive impairment and significant neurological challenges, affecting quality of life.
This variability highlights the unpredictable nature of Kelley-Seegmiller Syndrome. Early diagnosis is essential for tailoring interventions to meet individual needs and managing symptoms effectively over time. Understanding this spectrum helps caregivers and healthcare professionals provide appropriate support for affected individuals.
Neurological Manifestations: Cognitive Impairment and Behavioral Issues
Kelley-Seegmiller Syndrome often presents with neurological manifestations that can significantly affect a person’s daily life. Cognitive impairment is common, ranging from mild learning difficulties to moderate intellectual disability. This variability complicates the diagnosis and management of affected individuals.
“What Triggers Fibromyalgia Syndrome? Pain Management Guide”
Behavioral issues frequently accompany cognitive challenges. Patients may experience mood swings, anxiety, or even aggressive behavior. These psychological symptoms can stem from both biochemical imbalances and social pressures faced by those living with the disorder.
Early intervention through behavioral therapy and educational support plays a crucial role in improving outcomes. Tailored strategies can help address individual needs while fostering independence and enhancing quality of life for patients and their families.
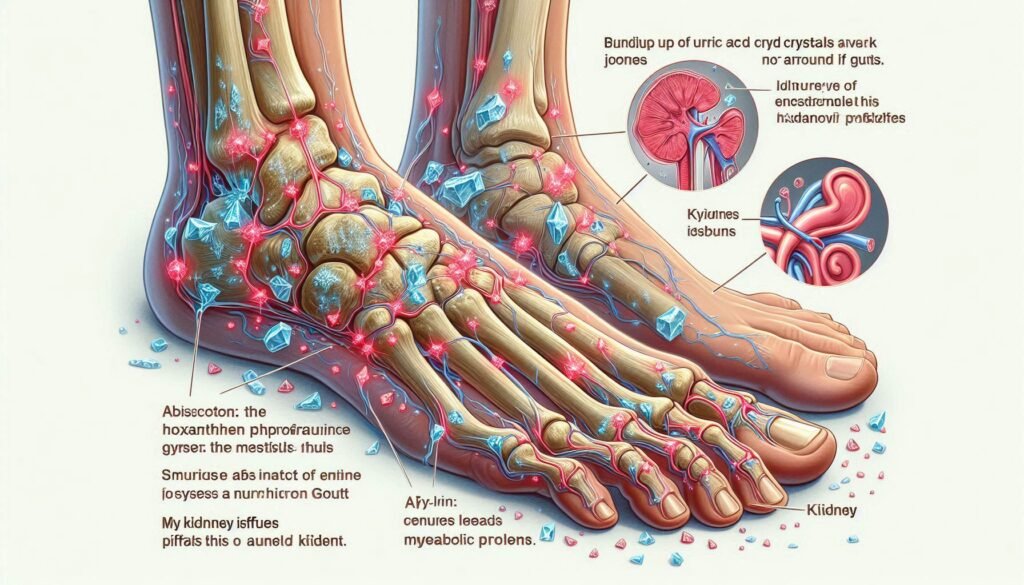
Renal Complications: Uric Acid Nephrolithiasis and Renal Failure
Renal complications are significant in Kelley-Seegmiller Syndrome, primarily due to elevated uric acid levels. Uric acid nephrolithiasis, or kidney stones, frequently occurs. These stones can lead to severe pain and urinary obstruction.
As the condition progresses, renal failure becomes a concern. The kidneys struggle to filter waste effectively when overwhelmed by excessive uric acid. This impairment may require more intensive medical management.
Early identification of these issues is crucial for preventing long-term damage. Regular monitoring of kidney function helps guide treatment decisions and maintain quality of life for affected individuals. Effective management strategies can significantly reduce the risk of serious renal complications.
Gouty Arthritis in Kelley-Seegmiller Syndrome: Mechanisms and Management
Gouty arthritis is a common complication in individuals with Kelley-Seegmiller Syndrome. This condition arises due to the accumulation of uric acid crystals in the joints, leading to painful inflammation. The underlying issue is an enzymatic deficiency that disrupts purine metabolism, causing elevated levels of uric acid.
Management of gouty arthritis focuses on reducing uric acid levels and alleviating pain. Allopurinol, a xanthine oxidase inhibitor, is often prescribed to help lower uric acid production. Additionally, nonsteroidal anti-inflammatory drugs (NSAIDs) can effectively manage acute flare-ups.
Lifestyle modifications also play a crucial role in treatment strategies. Patients are encouraged to stay hydrated and adopt a purine-restricted diet to minimize future episodes.
Diagnosis: Biochemical Tests and Genetic Analysis
Diagnosing Kelley-Seegmiller Syndrome begins with biochemical tests that measure levels of uric acid and other metabolites in the blood. Elevated uric acid levels are commonly observed, providing a preliminary indication of HPRT deficiency.
Genetic analysis plays a crucial role in confirming the diagnosis. Testing for mutations in the HPRT1 gene can identify specific changes linked to this syndrome. This genetic evaluation often involves techniques like sequencing or deletion/duplication analysis.
Healthcare providers may recommend these diagnostic approaches when clinical symptoms align with Kelley-Seegmiller Syndrome. Early identification is vital for appropriate management and treatment strategies tailored to each patient’s needs.
Prenatal Testing and Genetic Counseling for At-Risk Families
Prenatal testing plays a crucial role for families at risk of Kelley-Seegmiller Syndrome. It allows parents to assess the likelihood of passing on the disorder, particularly if there is a known family history.
Genetic counseling offers essential support during this process. A genetic counselor can provide information about testing options and help interpret results, ensuring that families make informed decisions.
Families may consider various tests, including chorionic villus sampling (CVS) or amniocentesis. These procedures analyze fetal DNA to identify potential HPRT gene mutations associated with Kelley-Seegmiller Syndrome early in pregnancy, enabling proactive care planning if needed.
Treatment Approaches: Allopurinol and Other Uric Acid-Lowering Therapies
Allopurinol is a cornerstone in managing Kelley-Seegmiller Syndrome. It works by inhibiting xanthine oxidase, an enzyme involved in uric acid production. This helps to lower serum uric acid levels and reduce the risk of gout attacks.
Other uric acid-lowering therapies may include febuxostat, which also targets xanthine oxidase but has different pharmacological properties. These alternatives can be beneficial for patients who do not tolerate allopurinol well.
Regular monitoring of uric acid levels is essential during treatment. Adjustments to medication dosages may be necessary based on individual responses and any potential side effects experienced by the patient.
Dietary Modifications: Role of Purine-Restricted Diets
Dietary modifications play a crucial role in managing Kelley-Seegmiller Syndrome. A purine-restricted diet significantly aids in controlling uric acid levels. By limiting foods high in purines, patients can reduce the risk of gout and related complications.
Key dietary sources to avoid include red meats, organ meats, and certain seafood. These foods contribute to elevated uric acid production, exacerbating symptoms associated with this condition.
Instead, individuals can benefit from focusing on low-purine alternatives like fruits, vegetables, and whole grains. Staying hydrated is also essential for kidney health and preventing stone formation as part of an effective management strategy for Kelley-Seegmiller Syndrome.
Managing Neurological Symptoms: Behavioral and Pharmacological Interventions
Managing neurological symptoms in Kelley-Seegmiller Syndrome involves a blend of behavioral strategies and pharmacological treatments. Behavioral interventions may include cognitive-behavioral therapy (CBT) to help address anxiety, attention deficits, and mood fluctuations. These therapies can foster coping mechanisms that empower patients.
Pharmacological options often focus on mood stabilization and managing impulsivity. Medications such as stimulants or selective serotonin reuptake inhibitors (SSRIs) are commonly employed based on individual needs. Regular monitoring by healthcare professionals ensures optimal dosage adjustments.
Collaboration among neurologists, psychologists, and caregivers is vital for effective management. This multidisciplinary approach enhances the quality of care and supports better outcomes for those affected by Kelley-Seegmiller Syndrome.
Renal Protection Strategies in Kelley-Seegmiller Syndrome
Renal protection is crucial for individuals with Kelley-Seegmiller Syndrome due to the risk of kidney damage from elevated uric acid levels. Regular monitoring of renal function helps detect early signs of impairment, allowing prompt intervention.
Hydration plays a key role in protecting kidney health. Drinking plenty of fluids can dilute uric acid concentrations and prevent crystal formation in the kidneys. This simple strategy significantly reduces the likelihood of nephrolithiasis.
Additionally, medications like allopurinol are effective in managing high uric acid levels. By lowering urate concentration, these treatments help preserve kidney function and minimize complications associated with this rare metabolic disorder.
Long-term Prognosis and Quality of Life Considerations
Long-term prognosis for individuals with Kelley-Seegmiller Syndrome varies widely. Some patients may experience mild symptoms, while others face significant health challenges. Early diagnosis and intervention can greatly improve outcomes.
Quality of life is influenced by various factors. Regular medical management, including medication adherence and lifestyle modifications, plays a crucial role in minimizing complications. Supportive care helps mitigate the impact of neurological and renal issues.
Emotional well-being is equally important. Access to psychological support can enhance coping strategies for both patients and families. Building a strong support network fosters resilience, allowing affected individuals to lead fulfilling lives despite their condition.
Psychological Support for Patients and Caregivers
Coping with Kelley-Seegmiller Syndrome can be emotionally taxing for both patients and caregivers. Psychological support plays a critical role in managing the mental health challenges that arise from living with a rare disorder. Access to counseling or therapy can provide essential coping strategies and emotional relief.
Support groups offer an invaluable resource, allowing individuals to connect with others facing similar struggles. Sharing experiences fosters understanding, reducing feelings of isolation.
Caregivers often experience their own set of stressors as they navigate responsibilities while supporting loved ones. Mental health resources tailored specifically for caregivers can help them maintain resilience and well-being amidst the challenges they face daily.
Educational Adaptations for Affected Individuals
Individuals with Kelley-Seegmiller Syndrome often face unique learning challenges. Tailored educational adaptations can greatly enhance their academic experience. Teachers should be aware of these needs and provide appropriate support.
Implementing individualized education plans (IEPs) is crucial. These plans can include modified assignments, additional time for tests, or the use of technology to assist in learning. A structured environment helps students focus better.
Peer support and social interaction are vital too. Encouraging group activities fosters collaboration while building self-esteem. With the right adaptations, affected individuals can thrive academically and socially, paving the way for a brighter future.
Latest Research: Enzyme Replacement and Gene Therapy Prospects
Recent research on Kelley-Seegmiller syndrome has unveiled promising avenues in enzyme replacement therapy (ERT) and gene therapy. Scientists are investigating how ERT can restore the missing function of hypoxanthine-guanine phosphoribosyltransferase (HPRT), potentially alleviating some biochemical deficits.
Gene therapy is also gaining traction as a transformative approach. By delivering functional copies of the HPRT gene, researchers aim to correct the underlying genetic defect responsible for this condition. Early animal models have shown encouraging results, with improvements in metabolic profiles and behavioral outcomes.
These innovative therapies could revolutionize treatment options for individuals affected by Kelley-Seegmiller syndrome, providing hope for better management strategies in the near future.
Differential Diagnosis: Distinguishing from Other Purine Metabolism Disorders
Diagnosing Kelley-Seegmiller Syndrome can be complex due to its overlap with other purine metabolism disorders. Conditions like Lesch-Nyhan syndrome and adenine phosphoribosyltransferase deficiency share similar biochemical pathways and clinical features.
Clinicians must assess symptoms, family history, and perform specific biochemical tests to differentiate these disorders effectively. For instance, elevated uric acid levels are common in both Kelley-Seegmiller Syndrome and gout.
Genetic testing plays a crucial role in clarifying the diagnosis. Identifying mutations in the HPRT1 gene confirms Kelley-Seegmiller Syndrome while ruling out mimicking conditions. Proper differential diagnosis ensures patients receive appropriate management tailored to their unique needs.
Living with Kelley-Seegmiller Syndrome: Patient Experiences and Coping Strategies
Living with Kelley-Seegmiller Syndrome can be challenging. Patients often face a myriad of symptoms that affect their daily lives, from cognitive difficulties to renal issues. Each individual’s experience varies widely, making personal coping strategies essential.
Many patients find support through peer groups and online communities. Sharing experiences helps them feel less isolated. These networks provide practical advice on managing symptoms and navigating healthcare challenges.
Coping strategies may include stress management techniques, such as mindfulness or yoga. Additionally, maintaining regular communication with healthcare providers ensures better symptom control and understanding of the condition’s evolving nature.
Support Organizations and Resources for Rare Metabolic Disorders
Navigating the complexities of Kelley-Seegmiller Syndrome can be daunting for patients and families. Thankfully, numerous support organizations provide valuable resources tailored to rare metabolic disorders. Organizations like the National Organization for Rare Disorders (NORD) offer guidance on accessing care, financial aid, and community connections.
The Genetic Alliance is another excellent resource, focusing on genetic conditions. They provide information on research developments and patient advocacy. Local support groups often foster a sense of belonging among families affected by similar challenges.
Additionally, online forums allow individuals to connect with others facing Kelley-Seegmiller Syndrome. These platforms enable sharing experiences and coping strategies in real-time.
Accessing these resources can empower patients and caregivers as they navigate their journeys with this condition. Support networks play a crucial role in enhancing quality of life for those impacted by Kelley-Seegmiller Syndrome.