Introduction to Ehlers–Danlos Syndrome
Ehlers–Danlos Syndrome (EDS) is a complex and often misunderstood group of genetic disorders that affect connective tissues, primarily collagen. For those navigating life with EDS, understanding this condition is crucial for managing its symptoms and improving quality of life.
This comprehensive guide aims to shed light on what EDS entails, from its diverse types and genetic underpinnings to the signs and symptoms you should look out for. Whether you are living with EDS or seeking to support someone who is, this resource will equip you with valuable knowledge about this intricate syndrome. Join us as we explore the multifaceted world of Ehlers-Danlos Syndrome together!

Ehlers–Danlos Syndrome Definition and Overview
Ehlers–Danlos Syndrome (EDS) is a group of connective tissue disorders characterized by hypermobility, skin elasticity, and tissue fragility. These conditions arise from defects in collagen, the protein that provides strength and flexibility to various tissues in the body.
There are several types of EDS, each with distinct features and inheritance patterns. Despite shared characteristics such as joint hypermobility, symptoms can vary widely among individuals. This variability makes diagnosis challenging.
“Why Does Lhermitte-Duclos Syndrome Affect The Cerebellum?”
People living with EDS often experience chronic pain and fatigue due to their unique physical challenges. Early recognition plays a crucial role in managing symptoms effectively. Understanding this syndrome is essential for those affected and their healthcare providers to ensure proper support and treatment options tailored to individual needs.
Historical Background
Ehlers-Danlos Syndrome (EDS) has a rich history that dates back to the early 20th century. The condition was first described by Dr. Edvard Ehlers in 1901 and later characterized further by Dr. Henri Danlos in the 1920s. Their work laid the foundation for understanding this complex genetic disorder.
Initially, EDS was recognized primarily for its joint hypermobility and skin abnormalities. Over time, medical experts identified various types of EDS, each with distinct characteristics and inheritance patterns.
Research into the genetic underpinnings began gaining momentum in the late 20th century, leading to significant advances in diagnosis and management strategies. As awareness grew, so did recognition of associated complications, prompting more comprehensive studies on patient experiences.
Today, individuals living with EDS benefit from improved diagnostic criteria and multidisciplinary care approaches that reflect decades of evolving understanding about this syndrome’s complexity.
Types of Ehlers–Danlos Syndrome
Ehlers–Danlos Syndrome (EDS) encompasses several distinct types, each with unique characteristics. Understanding these variations is crucial for accurate diagnosis and management.
Classical EDS is characterized by skin that stretches easily and joint hypermobility. Patients often experience bruising and scarring issues, making everyday activities challenging.
Hypermobile EDS primarily affects joint stability. Individuals may have frequent dislocations or chronic pain but usually lack the skin symptoms seen in other types.
“How Does Liddle Syndrome Impact Blood Pressure?”
Vascular EDS poses significant risks due to fragile blood vessels and organs. This type can lead to life-threatening complications, necessitating careful monitoring.
Other rare forms of EDS exist as well, including kyphoscoliotic and arthrochalasis types. Each variant has its own genetic underpinnings and clinical features, highlighting the need for specialized care tailored to individual needs within this diverse group of disorders.
Classical EDS
Classical Ehlers-Danlos Syndrome (cEDS) is one of the most recognized types of EDS. It primarily affects connective tissues, leading to distinctive features in skin and joints.
Individuals with classical EDS often exhibit highly elastic skin that has a velvety texture. This elasticity can also make the skin susceptible to bruising and scarring easily.
Joint hypermobility is another hallmark symptom. Many patients experience frequent joint dislocations or subluxations, which can lead to chronic pain over time.
Genetic mutations affecting collagen production are responsible for this condition. These defects cause structural weaknesses in connective tissue throughout the body.
“What Causes Maffucci Syndrome? Tumor Formation Guide”
Diagnosis typically involves clinical evaluation alongside family history assessments. Since symptoms can vary widely among individuals, proper recognition by healthcare providers is crucial for effective management strategies.
Hypermobile EDS
Hypermobile Ehlers-Danlos Syndrome (hEDS) is one of the most common forms of EDS. It primarily affects joint flexibility, leading to hypermobility that can cause pain and instability.
Individuals with hEDS often experience frequent dislocations or subluxations. These occurrences are not only painful but can also lead to long-term joint damage if left unaddressed.
“Why Does MRKH Syndrome Affect Female Development?”
Unlike other types, hEDS may not present clear skin changes or vascular issues. This makes diagnosis more challenging and reliant on clinical assessment rather than genetic testing.
Chronic pain is a hallmark symptom, affecting daily activities and overall quality of life. Patients report fatigue due to constant discomfort and the effort required for mobility.
Awareness about hypermobile EDS has grown, emphasizing the need for appropriate management strategies tailored to each individual’s specific symptoms and challenges.
Vascular EDS
Vascular Ehlers-Danlos Syndrome (vEDS) is one of the more severe types of EDS. It primarily impacts the body’s connective tissues, particularly blood vessels. Individuals with vEDS often experience fragile arteries that can lead to life-threatening complications.
One of the hallmark features of this condition is a tendency for spontaneous arterial ruptures. This risk elevates significantly during pregnancy or physical exertion. People affected may also notice thin, translucent skin that bruises easily.
“How Does Meige Syndrome Cause Facial Spasms?”
Additionally, those with vascular EDS may face other issues like organ rupture and joint hypermobility, though it’s generally less pronounced than in other forms of EDS. Genetic mutations affecting collagen synthesis are responsible for these symptoms.
Awareness and early diagnosis are crucial for managing risks associated with this syndrome effectively. Regular monitoring by healthcare professionals can help mitigate potential complications related to vascular health.
Other Rare Types
Ehlers-Danlos Syndrome comprises several rare types beyond the more common classifications. These atypical forms can present unique challenges and symptoms.
For instance, Kyphoscoliotic EDS is characterized by severe curvature of the spine and muscle weakness. Individuals may also experience joint problems from a young age.
Another rare variant is Arthrochalasia EDS, which involves extreme joint laxity coupled with a risk of hip dislocation. It necessitates careful management to prevent injuries.
“What Are The Signs of Metabolic Syndrome? Prevention Guide”
Dermatosparaxis EDS affects collagen production, leading to fragile skin that bruises easily. Patients often have slow-healing wounds due to compromised tissue integrity.
There are other even less common subtypes identified in ongoing research. Each type requires tailored approaches for effective treatment and support based on its specific characteristics and patient needs.
Genetic Basis of Ehlers–Danlos Syndrome
Ehlers–Danlos Syndrome (EDS) primarily stems from genetic mutations affecting collagen production. Collagen is a crucial protein that provides structure and strength to the skin, joints, and blood vessels.
Most types of EDS follow an autosomal dominant inheritance pattern. This means just one mutated copy of the gene can lead to the disorder. However, some rarer forms have different inheritance patterns.
The primary defects in EDS are found in genes responsible for making various collagen types. These defects result in weaker connective tissues, leading to the hallmark symptoms associated with this syndrome.
Genetic testing plays a vital role in confirming diagnoses. It helps identify specific mutations linked to particular EDS types. Early identification through genetic evaluation can guide effective management strategies tailored to individual needs.
Inheritance Patterns
Ehlers-Danlos Syndrome (EDS) is primarily inherited in an autosomal dominant manner. This means that only one copy of the mutated gene from an affected parent can lead to the condition in offspring.
However, certain types of EDS follow different inheritance patterns. For instance, some variants may exhibit autosomal recessive traits. In these cases, both parents must carry a mutation for their child to be affected.
Genetic diversity also contributes to unique presentations of EDS within families. Even if multiple family members have the syndrome, symptoms and severity can vary significantly among individuals.
Understanding these patterns is crucial for genetic counseling and risk assessment in families with a history of EDS. Proper knowledge aids in making informed decisions about family planning and management strategies moving forward.
Collagen Defects
Collagen defects are at the core of Ehlers–Danlos Syndrome (EDS). Collagen is a crucial protein that provides structure and strength to our skin, joints, and connective tissues. In individuals with EDS, mutations in genes responsible for collagen production lead to weakened tissue integrity.
These defects can manifest in various forms depending on the type of EDS. For example, classical EDS features skin that’s stretchy and fragile due to faulty collagen. Hypermobile EDS primarily affects joint stability because of irregularities in connective tissues.
The impact of these defects goes beyond physical symptoms; they can also contribute to chronic pain and other complications. Understanding the role of collagen is essential for managing this complex condition effectively.
Research continues into how these genetic abnormalities disrupt normal bodily functions, offering hope for better treatments and interventions tailored specifically for those affected by Ehlers–Danlos Syndrome.
Genetic Testing
Genetic testing plays a crucial role in diagnosing Ehlers–Danlos Syndrome. It identifies specific mutations in genes associated with collagen production and function. These genetic variations help determine the type of EDS present.
Healthcare providers may recommend different testing methods based on clinical symptoms. Targeted mutation analysis is common for identifying known gene defects, while whole exome sequencing can uncover novel mutations in more complex cases.
Understanding the genetic basis of EDS aids not only in diagnosis but also informs treatment decisions and family planning. Genetic counseling often accompanies these tests, offering insights into inheritance patterns and potential outcomes for relatives.
While testing provides valuable information, it’s essential to interpret results within the broader context of clinical findings. Each individual’s experience with EDS varies widely, making personalized care approaches vital for effective management.
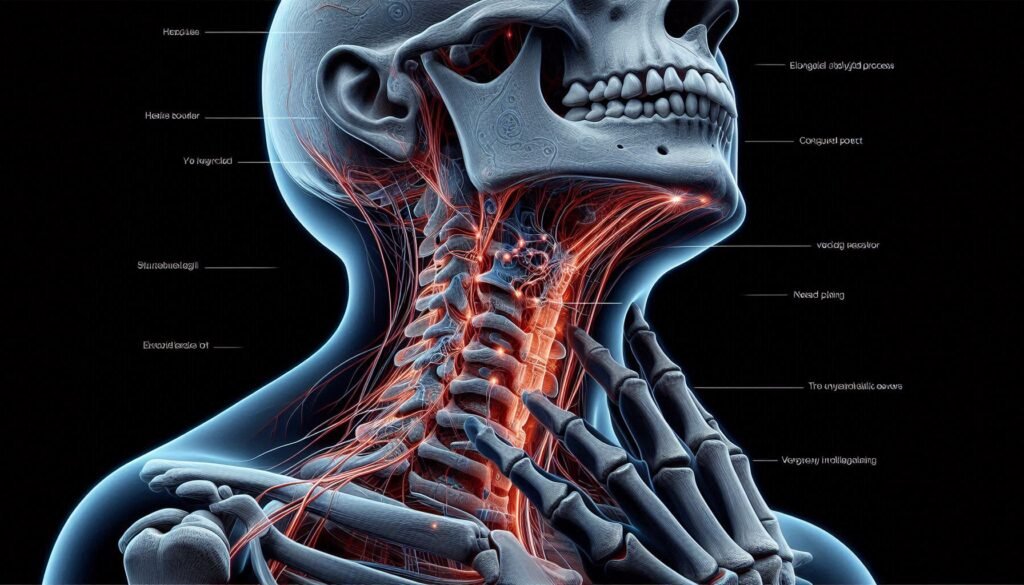
Ehlers–Danlos Syndrome Signs and Symptoms
Ehlers–Danlos Syndrome presents a variety of signs and symptoms that can significantly impact daily life. One of the most notable features is joint hypermobility. Individuals often experience joints that move beyond the normal range, leading to frequent dislocations or sprains.
Skin hyperextensibility is another hallmark trait. People with EDS may notice their skin feels unusually stretchy or fragile, making it susceptible to bruising and injury.
Tissue fragility can cause complications in healing processes. Wounds may take longer to mend, increasing the risk of scarring.
Chronic pain also affects many individuals with Ehlers–Danlos Syndrome, stemming from joint instability and muscle strain over time.
Cardiovascular complications are common as well; some might experience issues like orthostatic intolerance or arrhythmias due to blood vessel irregularities. Each symptom varies among patients but collectively underscores the complexity of living with this condition.
Joint Hypermobility
Joint hypermobility refers to the ability of joints to move beyond their normal range of motion. It is a common feature in individuals with Ehlers–Danlos Syndrome (EDS). This condition can lead to increased flexibility but may also cause discomfort and instability.
People with joint hypermobility often experience frequent joint dislocations or subluxations. These occurrences can result in pain, swelling, and reduced mobility over time. The laxity in connective tissues makes the joints vulnerable during physical activities.
It’s important for those affected by joint hypermobility to engage in exercises that strengthen surrounding muscles. Targeted physical therapy can help improve stability and reduce injury risks. Additionally, awareness of one’s limitations is crucial for managing daily tasks effectively without exacerbating symptoms linked to EDS.
Skin Hyperextensibility
Skin hyperextensibility is one of the hallmark features of Ehlers-Danlos Syndrome. Individuals with this condition often notice that their skin stretches more than what is typical. This characteristic can be both fascinating and troublesome.
The excessive stretchiness can lead to an increased risk of injury, as the skin may not provide adequate support or protection. Minor bumps or scratches could result in unusual tearing or bruising.
This trait also contributes to cosmetic concerns for many affected individuals. The appearance of wrinkles and sagging skin may develop earlier than expected due to its inherent fragility.
Moreover, maintaining healthy skin becomes essential for those with EDS. Specialized skincare routines are often recommended to minimize damage and manage sensitivity effectively.
Tissue Fragility
Tissue fragility is a hallmark symptom of Ehlers–Danlos Syndrome. Individuals with this condition often experience skin and connective tissues that are more prone to damage than those without it. This increased susceptibility can lead to frequent bruising, cuts, or tears.
The fragile nature of the tissues stems from defects in collagen production. Collagen serves as the body’s structural protein, providing strength and elasticity. When collagen is impaired, it compromises the integrity of various body systems.
People may notice signs of tissue fragility manifesting as slow-healing wounds or excessive scarring after injuries. Everyday activities can become daunting when simple bumps or falls result in serious injuries.
Managing tissue fragility involves being mindful about physical activities and taking precautions to protect vulnerable areas. Awareness plays a crucial role in minimizing risk and ensuring safety during daily routines.
Chronic Pain
Chronic pain is a prevalent symptom for many individuals with Ehlers–Danlos Syndrome (EDS). It can arise from joint instability, soft tissue injuries, or inflammation related to the condition. This pain often varies in intensity and may shift locations.
People with EDS frequently describe their chronic pain as sharp, aching, or throbbing. The unpredictability of this discomfort can be particularly challenging to manage. Simple activities might become daunting due to the fear of exacerbating symptoms.
Moreover, chronic pain impacts mental health significantly. Anxiety and depression are common among those dealing with persistent physical discomfort. Seeking effective strategies for coping becomes essential.
Pain management plans tailored specifically for EDS are crucial. These may involve medication, physical therapy, and lifestyle modifications aimed at improving overall quality of life while addressing specific symptoms associated with the syndrome.
Cardiovascular Complications
Ehlers–Danlos Syndrome can lead to various cardiovascular complications due to the structural weaknesses in connective tissues. One significant concern is the risk of arterial rupture, particularly in individuals with vascular EDS. This condition increases susceptibility to serious cardiovascular events.
Patients may also experience orthostatic intolerance, characterized by difficulty standing up without feeling faint or dizzy. This occurs because blood vessels may not constrict effectively, leading to poor circulation.
A common companion condition is Postural Orthostatic Tachycardia Syndrome (POTS), which involves an abnormal increase in heart rate when transitioning from lying down to standing up. POTS can exacerbate fatigue and limits daily activity levels significantly.
Ongoing monitoring of heart health and regular check-ups are crucial for those affected by Ehlers–Danlos Syndrome. Early intervention can help manage symptoms and reduce risks associated with these cardiovascular complications.
Ehlers–Danlos Syndrome Diagnosis of Ehlers–Danlos Syndrome
Diagnosing Ehlers–Danlos Syndrome (EDS) involves a careful approach. Physicians rely on established clinical criteria to identify the condition effectively. This includes an assessment of symptoms and physical examination findings.
One critical tool is the Beighton Score, which evaluates joint hypermobility through specific maneuvers. A higher score indicates greater flexibility, a hallmark of many EDS types.
Genetic testing also plays an essential role in confirming diagnoses. By identifying mutations in collagen genes, healthcare providers can determine the specific type of EDS present.
Differential diagnosis is crucial as well. Conditions like Marfan syndrome and osteogenesis imperfecta may share similar signs but require different management strategies. Careful evaluation ensures that patients receive accurate diagnoses for optimal care pathways, tailored specifically to their needs and symptoms.
Clinical Criteria
The clinical criteria for diagnosing Ehlers-Danlos Syndrome (EDS) involve a detailed evaluation of symptoms and physical findings. Medical professionals often use specific guidelines to assess the likelihood of EDS in patients.
A key component is evaluating joint hypermobility, which can be assessed using the Beighton Score. This score quantifies how many joints demonstrate increased flexibility.
Physicians also look for skin features characteristic of EDS, such as elasticity and bruising tendency. These signs help differentiate between various types of this syndrome.
Family history plays an essential role too. Many patients share information about relatives with similar health issues, aiding in diagnosis.
A thorough assessment often includes ruling out other conditions that mimic EDS symptoms to ensure accurate identification of the syndrome.
Beighton Score
The Beighton Score is a simple and widely used tool for assessing joint hypermobility. It consists of a series of five tests that evaluate how flexible certain joints are.
Each test scores either one or zero points, depending on whether the criteria are met. For example, bending forward to touch your toes without bending your knees earns you a point.
A higher score indicates greater hypermobility, with a total score ranging from zero to nine. A score of four or more typically suggests generalized joint hypermobility.
Healthcare providers often utilize the Beighton Score as part of the diagnostic process for Ehlers-Danlos Syndrome and related disorders. Its simplicity makes it accessible for both professionals and patients alike, allowing for straightforward assessments in clinical settings.
Genetic Testing Methods
Genetic testing for Ehlers–Danlos Syndrome (EDS) is crucial in confirming a diagnosis. Several methods are available to identify the specific genetic mutations associated with different types of EDS.
One common approach is targeted gene sequencing. This method focuses on specific genes known to be linked to EDS, allowing for quick identification of abnormalities. It’s efficient and less costly than other comprehensive tests.
Another option is whole exome sequencing, which analyzes all coding regions of DNA. While more extensive, it can uncover rare or previously unidentified mutations that contribute to the disorder.
Next-generation sequencing techniques have revolutionized how we approach genetic testing by providing rapid results and high accuracy.
Carrier testing may be offered for family members when a mutation has been identified in an affected individual. This helps assess the risk of passing on the condition to future generations.
Differential Diagnosis of Ehlers–Danlos Syndrome
Differential diagnosis of Ehlers–Danlos Syndrome (EDS) can be complex due to symptom overlap with various other conditions. Healthcare providers consider several disorders that could mimic the signs of EDS.
Conditions like Marfan syndrome share similar features, particularly regarding joint hypermobility and cardiovascular complications. Identifying these distinctions is crucial for appropriate management.
Other connective tissue disorders, such as osteogenesis imperfecta and Loeys-Dietz syndrome, also present challenges in diagnosis. Each condition has unique characteristics that must be carefully evaluated during clinical assessments.
Additionally, factors such as family history and patient-reported symptoms play a vital role in differentiating EDS from related syndromes. Comprehensive genetic testing may be necessary when uncertainty remains after physical examinations.
Thorough investigations ensure accurate diagnoses and effective treatment plans tailored to each individual’s needs. This careful approach helps optimize the quality of life for those affected by Ehlers–Danlos Syndrome or similar conditions.
Ehlers–Danlos Syndrome Management and Treatment
Managing Ehlers–Danlos Syndrome requires a comprehensive approach tailored to each individual’s needs. A multidisciplinary team often includes geneticists, rheumatologists, and physical therapists who work together to create personalized treatment plans.
Physical therapy plays a crucial role in improving joint stability and enhancing mobility. Targeted exercises can help strengthen muscles around hypermobile joints, reducing the risk of dislocations.
Pain management is another key component. Techniques may include medication, mindfulness practices, or alternative therapies like acupuncture to alleviate chronic discomfort.
Regular cardiovascular monitoring ensures that any issues related to heart health are identified early. This proactive approach can prevent complications associated with vascular EDS.
Surgical interventions might be necessary for severe cases but should always be approached cautiously due to potential healing difficulties linked with connective tissue disorders.
Multidisciplinary Approach
A multidisciplinary approach is essential for effectively managing Ehlers–Danlos Syndrome. This strategy involves collaboration among various healthcare professionals to address the diverse needs of patients.
Each specialist plays a distinct role. Rheumatologists focus on joint issues, while geneticists help understand the underlying genetic components. Physical therapists provide tailored exercises to enhance mobility and strength.
This collaborative effort ensures comprehensive care. Regular communication between team members fosters a holistic understanding of each patient’s unique challenges.
Additionally, mental health specialists are crucial in supporting emotional well-being, as living with Ehlers–Danlos can lead to anxiety or depression.
Patients benefit from this integrated model by receiving personalized treatment plans that encompass physical and psychological aspects of their condition. The goal is not only symptom management but also improving overall quality of life through coordinated support and education across disciplines.
Physical Therapy
Physical therapy plays a crucial role in managing Ehlers–Danlos Syndrome. It focuses on improving strength, flexibility, and stability.
Therapists often design personalized exercise programs that cater to individual needs and abilities. These exercises help support the joints and prevent injury.
Patients may also benefit from techniques like manual therapy or proprioceptive training. Such interventions enhance body awareness, which can reduce the risk of dislocations.
Balance training is another important aspect. Many individuals with EDS experience joint instability; therefore, working on balance can significantly improve their quality of life.
Education about proper movement patterns is essential as well. Understanding how to move safely throughout daily activities can empower patients to manage their condition more effectively.
Regular physical therapy sessions foster not only physical improvements but also emotional resilience, allowing those affected by Ehlers–Danlos Syndrome to lead fulfilling lives despite challenges.
Pain Management
Managing pain effectively is crucial for individuals with Ehlers–Danlos Syndrome. Chronic pain can significantly impact daily life, making it essential to adopt a tailored approach.
A multidisciplinary team often collaborates to create a comprehensive pain management plan. This may include medication such as non-steroidal anti-inflammatory drugs (NSAIDs) or opioids in certain cases. Always consult with healthcare providers before starting any medication.
Physical therapy plays an important role too. Targeted exercises can strengthen muscles and improve joint stability, helping reduce discomfort over time. Additionally, techniques like hydrotherapy might provide relief through gentle movement in water.
Complementary therapies, including acupuncture and massage therapy, have shown promise for some patients. These methods aim to alleviate tension and enhance overall well-being.
Cognitive-behavioral therapy (CBT) can aid in addressing the emotional aspects of chronic pain by teaching coping strategies and promoting resilience.
Cardiovascular Monitoring
Cardiovascular monitoring is crucial for individuals with Ehlers–Danlos Syndrome. This condition can lead to various cardiovascular complications, including vascular fragility and abnormalities in blood pressure regulation.
Regular evaluations by a healthcare provider are essential. They help assess heart function and monitor for signs of potential issues such as arrhythmias or valve problems.
Many patients experience orthostatic intolerance, which can manifest as dizziness upon standing. Monitoring heart rate and blood pressure during positional changes provides valuable insights into individual responses.
Some may benefit from wearing continuous heart rate monitors, offering real-time data on their cardiovascular status. This information helps tailor treatment plans effectively.
Collaboration with cardiologists experienced in EDS is beneficial for comprehensive care. Their expertise ensures that specific risks associated with the syndrome are addressed promptly and appropriately.
Surgical Considerations
Surgical considerations for individuals with Ehlers–Danlos Syndrome (EDS) require careful planning and execution. Due to tissue fragility, surgical procedures can pose significant risks. Surgeons need to be aware of the potential complications related to healing and recovery.
Prior to surgery, a thorough assessment is essential. This includes understanding the patient’s specific type of EDS and any associated conditions that could impact surgical outcomes. Collaboration among specialists can lead to better management strategies.
Post-operative care is equally crucial. Patients may experience delayed wound healing or increased scarring due to their condition. Continuous monitoring helps in identifying complications early on.
Minimally invasive techniques are often preferred when possible, as they reduce stress on fragile tissues. Ensuring adequate pain control post-surgery also plays a vital role in rehabilitation, allowing patients a smoother recovery process while managing their unique challenges effectively.
Living with Ehlers–Danlos Syndrome
Living with Ehlers–Danlos Syndrome presents daily challenges that can be overwhelming. Individuals may struggle with joint pain and fatigue, making even simple tasks feel monumental. The unpredictability of symptoms often complicates planning daily activities.
Adaptive strategies become essential for managing life effectively. Many find solace in using assistive devices or modifying their environment to reduce strain on their joints. Staying active within personal limits is vital; gentle exercises can help maintain mobility without exacerbating symptoms.
The psychological impact cannot be overlooked. Anxiety and depression are common as individuals navigate fluctuating health issues and societal misunderstandings about invisible disabilities. Support from friends, family, or support groups creates a network that fosters connection and understanding.
Mindfulness practices can also provide relief from stress while enhancing emotional well-being. Living authentically and seeking joy amid the struggles helps build resilience against the hurdles posed by this complex condition.
Daily Challenges
Living with Ehlers–Danlos Syndrome often means navigating a range of daily challenges. Individuals may experience joint pain or instability, making even simple tasks seem daunting. Everyday activities like climbing stairs or carrying groceries can lead to dislocations or sprains.
Fatigue is another common hurdle. Chronic exhaustion can affect concentration and motivation, leading to difficulties in work or school settings. This fatigue doesn’t just stem from physical exertion; it’s also related to ongoing pain management.
Social interactions may be strained as well. Friends and family might not fully understand the invisible nature of the condition, which can lead to feelings of isolation. Balancing social life with health needs requires careful planning and communication.
Adapting routines becomes essential for maintaining independence while managing symptoms effectively. Prioritizing rest and pacing oneself are strategies that many find beneficial amid these daily struggles.
Adaptive Strategies
Living with Ehlers–Danlos Syndrome requires embracing adaptive strategies to enhance daily life. One effective approach includes utilizing assistive devices such as braces or splints. These tools can provide joint support and reduce the risk of injuries.
Prioritizing rest is crucial. Scheduling breaks throughout the day helps manage fatigue, allowing individuals to recharge their energy levels. Incorporating gentle exercises, like swimming or yoga, can improve muscle strength without overstressing joints.
Creating a structured environment also aids in managing symptoms. Organizing tasks and using reminders can help maintain focus and productivity while minimizing strain on the body.
Engaging in open communication with family members fosters understanding. Sharing experiences encourages loved ones to offer support tailored to individual needs, enhancing overall well-being and resilience against challenges posed by this condition.
Psychological Impact
Living with Ehlers–Danlos Syndrome can take a significant toll on mental health. Chronic pain, fatigue, and unpredictable symptoms create daily stress. This constant strain often leads to anxiety and depression.
Individuals may feel isolated due to their condition. Friends and family might not fully understand the challenges they face. This lack of understanding can exacerbate feelings of loneliness.
Coping with the uncertainty of flare-ups adds another layer of emotional burden. Many patients worry about their future mobility or potential complications. These concerns can lead to frustration and hopelessness.
Support groups offer a valuable space for connection and sharing experiences. Engaging in therapy also provides tools for managing emotions effectively. Addressing psychological needs is just as important as treating physical symptoms in Ehlers–Danlos Syndrome management.
Complications and Associated Conditions
Ehlers-Danlos Syndrome can lead to various complications and associated conditions that significantly impact an individual’s quality of life. One common issue is Chronic Fatigue Syndrome, where individuals experience persistent fatigue that doesn’t improve with rest. This condition often exacerbates the overall discomfort faced by those living with EDS.
Another frequent complication is Postural Orthostatic Tachycardia Syndrome (POTS). People with POTS may suffer from rapid heart rates and dizziness upon standing. These symptoms can complicate daily activities and require careful management.
Gastrointestinal issues are also prevalent among EDS patients. Many experience problems like irritable bowel syndrome or gastroparesis, leading to digestive challenges and nutritional deficiencies.
Awareness of these complications is crucial for effective management strategies tailored to each individual’s needs.
Chronic Fatigue Syndrome
Chronic Fatigue Syndrome (CFS) is a complex condition characterized by extreme fatigue that doesn’t improve with rest. This debilitating exhaustion can interfere significantly with daily activities and quality of life.
Individuals with CFS often experience additional symptoms, such as sleep disturbances, cognitive difficulties, and musculoskeletal pain. The fatigue may worsen after physical or mental exertion, leading to what is commonly referred to as post-exertional malaise.
The exact cause of CFS remains unclear. Some theories suggest it could stem from viral infections, immune system dysfunctions, or hormonal imbalances.
Diagnosis typically involves ruling out other conditions and identifying the characteristic symptoms over time. Treatment focuses on managing symptoms through lifestyle changes and supportive therapies rather than offering a one-size-fits-all solution.
Living with Chronic Fatigue Syndrome requires careful management of energy levels along with ongoing support from healthcare professionals who understand this unique challenge.
Postural Orthostatic Tachycardia Syndrome (POTS)
Postural Orthostatic Tachycardia Syndrome (POTS) is a condition that affects blood flow and heart rate. It primarily occurs when someone transitions from sitting or lying down to standing up.
Individuals with POTS experience an exaggerated increase in heart rate, often exceeding 30 beats per minute within ten minutes of standing. This can lead to symptoms such as dizziness, lightheadedness, fatigue, and even fainting.
POTS is commonly linked with Ehlers-Danlos Syndrome due to the connective tissue abnormalities that both conditions share. These issues can affect vascular stability and autonomic regulation.
Management of POTS typically includes lifestyle changes, increased fluid intake, and specific exercises aimed at improving circulation. In some cases, medications may be prescribed to help manage symptoms effectively while allowing individuals to maintain a more active lifestyle.
Gastrointestinal Issues
Ehlers–Danlos Syndrome (EDS) can lead to various complications and associated conditions that significantly impact the lives of those affected. One such complication is gastrointestinal issues, which are reported frequently among EDS patients. These problems may manifest as digestive disorders, including irritable bowel syndrome (IBS), gastroparesis, or food intolerances.
Individuals with EDS often experience symptoms like abdominal pain, bloating, and constipation. This discomfort can stem from a combination of connective tissue laxity affecting the gut’s structure and function along with autonomic dysfunction related to EDS. Managing these gastrointestinal challenges typically requires a tailored approach that considers both dietary adjustments and medical interventions.
Moreover, it’s essential for individuals living with Ehlers–Danlos Syndrome to maintain open communication with healthcare providers about their symptoms. A multidisciplinary team can provide comprehensive care addressing not only musculoskeletal concerns but also any overlapping gastrointestinal issues.
Living well with EDS involves recognizing its multifaceted nature and seeking support across different areas of health. By understanding these potential complications better, individuals can advocate for themselves more effectively while navigating their unique experiences with this complex condition.