Baboon Syndrome, scientifically known as symmetrical drug-related intertriginous and flexural exanthema (SDRIFE), is a condition that often flies under the radar. Yet, it can have significant implications for those affected.
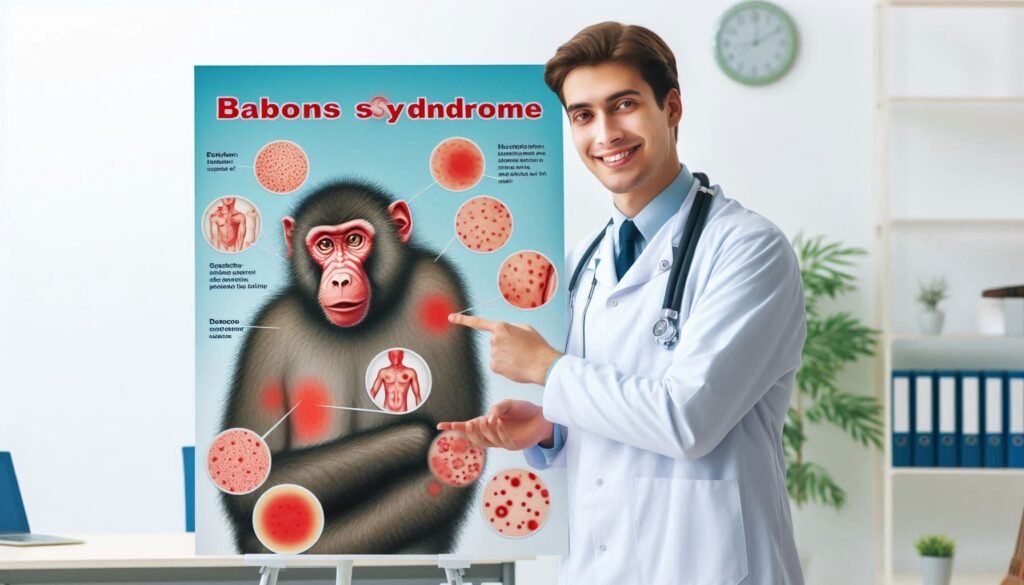
This unique skin reaction usually presents as an alarming red rash in areas where skin folds over one another, resembling the distinctive coloration of a baboon’s behind. Understanding this syndrome is essential not only for healthcare professionals but also for patients who may unknowingly trigger it through medication.
Recognizing Baboon Syndrome matters because it can significantly impact a person’s quality of life. The discomfort and potential for misdiagnosis can lead individuals down unnecessary treatment paths if not properly identified.
Increasing awareness among healthcare providers ensures prompt diagnosis and effective management strategies are implemented. Patients experiencing unusual rashes should consult their doctors regarding possible medication links to avoid further complications associated with SDRIFE.
As we explore Baboon Syndrome further, we’ll uncover its causes, symptoms, diagnosis methods, and potential treatments. Recognizing this condition can lead to quicker interventions and better management strategies for individuals dealing with its effects. Join us on this informative journey to demystify SDRIFE and shed light on why awareness matters.

Overview of Baboon Syndrome or Symmetrical Drug-Related Intertriginous and Flexural Exanthema (SDRIFE)
Baboon Syndrome, also known as symmetrical drug-related intertriginous and flexural exanthema (SDRIFE), is a rare dermatological condition. It primarily manifests as red, inflamed skin in the folds of the body, such as underarms, groin areas, and around the buttocks. This syndrome usually occurs after exposure to certain medications.
“How Does Variably Protean Syndrome Present?”
The name “Baboon Syndrome” stems from its resemblance to the bright pink or red rumps of baboons. The inflammatory response can be quite distressing for those affected. It’s important to identify this condition early on for appropriate management.
Baboon Syndrome often correlates with allergic reactions to drugs like penicillin or other antibiotics. Understanding its characteristics helps in recognizing it promptly among various dermatoses.
Other Names of Baboon Syndrome
Baboon Syndrome is known by several other names, which can sometimes lead to confusion. One common term used interchangeably is symmetrical drug-related intertriginous and flexural exanthema (SDRIFE). This name highlights the condition’s characteristic rash that appears symmetrically in skin folds.
“What Causes Valentine Syndrome? Heart Condition Guide”
Another less commonly recognized name for Baboon Syndrome is “red butt syndrome.” This informal label reflects the appearance of the affected areas, particularly in individuals with more pronounced symptoms.
Additionally, some medical literature references it as a type of drug-induced dermatitis. Regardless of the terminology used, understanding these alternative names can help healthcare professionals accurately diagnose and treat this unique dermatological condition effectively.
Histopathology of Baboon Syndrome (SDRIFE)
The histopathology of Baboon Syndrome reveals distinct features. Typically, it shows a dense infiltrate of lymphocytes in the dermis. This infiltration is often accompanied by spongiosis, which indicates edema within the epidermal layer.
“Why Does Vanishing White Matter Syndrome Progress?”
Additionally, eosinophils may be present, suggesting an allergic or hypersensitivity reaction to certain medications. The involvement of these immune cells highlights the inflammatory nature of this condition.
Keratinocyte damage can also be observed in biopsy specimens. Such findings underscore how crucial it is for healthcare professionals to recognize these patterns while diagnosing and managing SDRIFE effectively. Understanding histopathological characteristics aids not only in confirming diagnosis but also in tailoring appropriate treatment plans.
Pathophysiology of Symmetrical Drug-related Intertriginous and Flexural Exanthema
Symmetrical Drug-related Intertriginous and Flexural Exanthema (SDRIFE) involves an immune-mediated response triggered by certain medications. The primary mechanism behind this condition is the activation of T-cells, which leads to inflammation in skin areas with folds or intertriginous zones.
“How Does VATER Syndrome Affect Multiple Systems?”
In SDRIFE, the drug acts as a hapten, binding to skin proteins and forming complexes that elicit a hypersensitivity reaction. This results in keratinocyte activation and subsequent production of pro-inflammatory cytokines.
The symmetrical distribution of lesions highlights its unique nature compared to other dermatoses. Skin fold involvement indicates a specific pathophysiological pattern associated with the underlying triggers, distinguishing it from other inflammatory conditions.
Etiology of SDRIFE (Baboon Syndrome)
The etiology of symmetrical drug-related intertriginous and flexural exanthema (SDRIFE), primarily revolves around an adverse drug reaction. This condition occurs when certain medications trigger a hypersensitivity response in the body.
“What Are The Signs of Waardenburg Syndrome?”
Common culprits include antibiotics like penicillin, anti-seizure drugs such as phenytoin, and non-steroidal anti-inflammatory drugs (NSAIDs). These substances can lead to characteristic skin eruptions in areas where skin folds occur.
Genetic predisposition may also play a role. Individuals with specific genetic markers could be more susceptible to developing SDRIFE after exposure to these triggering agents. Understanding these factors is crucial for diagnosis and preventive strategies.
Epidemiology and Baboon Syndrome
Baboon Syndrome, or SDRIFE, is relatively rare but increasingly recognized in clinical settings. It often occurs after exposure to certain medications, particularly those within the beta-lactam antibiotic class and some non-steroidal anti-inflammatory drugs (NSAIDs).
“Why Does Walker-Warburg Syndrome Affect Brain Development?”
Epidemiological studies suggest that this syndrome predominantly affects younger individuals. The incidence appears to be higher among males than females.
Geographically, cases have been documented worldwide, though variations exist based on local drug usage patterns and genetic predispositions. Understanding these epidemiological factors can aid healthcare professionals in identifying at-risk populations and improving patient outcomes through timely diagnosis and treatment strategies.
Causes and Clinical Features of Symmetrical Drug-related Intertriginous and Flexural Exanthema (SDRIFE)
Symmetrical drug-related intertriginous and flexural exanthema (SDRIFE), is primarily triggered by certain medications. Common culprits include antibiotics, non-steroidal anti-inflammatory drugs (NSAIDs), and anticonvulsants. These substances can provoke an immune response leading to the characteristic skin changes.
Clinically, SDRIFE presents as red, inflamed patches that typically appear in skin folds such as underarms, groin, and around the buttocks. The lesions often resemble a baboon’s posterior due to their color and location.
Patients may also experience pruritus or itching alongside the skin manifestations. While not life-threatening, these symptoms can lead to significant discomfort and affect quality of life if left untreated. Recognizing these features early is essential for effective management.
Signs and Symptoms of Baboon Syndrome
Baboon Syndrome primarily manifests through distinctive skin changes. These include bright red, inflamed patches located in the intertriginous areas—places where skin rubs against skin, such as the armpits and groin.
The affected areas may also exhibit scaling or crusting, leading to discomfort and itching. Importantly, these symptoms can develop rapidly after exposure to certain medications.
Accompanying systemic symptoms can sometimes occur, including fever or malaise. Patients might experience a sense of unease due to the sudden onset of these signs. Recognizing these indicators early is essential for effective management and treatment.
Diagnosis and Differential Diagnosis of SDRIFE (Baboon Syndrome)
Diagnosing Baboon Syndrome involves a comprehensive clinical evaluation. Dermatologists assess skin lesions’ characteristics and locations, focusing on symmetrical patterns in flexural areas like the groin and armpits.
A detailed patient history is crucial to identify recent drug exposures. Specific medications often trigger this condition, making it essential for healthcare providers to inquire about any new treatments or changes in medication regimens.
Differential diagnosis includes other dermatoses such as eczema, psoriasis, or contact dermatitis. A thorough examination helps distinguish these conditions based on lesion appearance and distribution. In some cases, a biopsy may be necessary to confirm the diagnosis of SDRIFE by ruling out other similar skin disorders.
Complications of SDRIFE
Complications of SDRIFE can significantly impact patients’ quality of life. While the condition is typically self-limiting, it may lead to secondary infections if skin integrity is compromised. The intense itching and discomfort often cause individuals to scratch affected areas, increasing this risk.
Additionally, emotional distress can arise from the visible lesions associated with Baboon Syndrome. This psychological toll might contribute to anxiety or depression in some patients, particularly those who experience recurrent episodes.
In rare cases, prolonged inflammation and irritation could result in post-inflammatory hyperpigmentation or scarring. These long-lasting effects serve as a reminder of the initial dermatological challenge faced by individuals suffering from symmetrical drug-related intertriginous and flexural exanthema.
Comparative Analysis with Other Similar Conditions
Baboon Syndrome shares similarities with several other dermatological conditions, making accurate diagnosis essential. Conditions such as drug-induced hypersensitivity syndrome and Stevens-Johnson syndrome can present with overlapping symptoms like rashes and inflammation. However, their underlying mechanisms differ significantly.
In contrast to Baboon Syndrome’s characteristic intertriginous involvement, eczema typically manifests in more generalized areas of the skin. Itching is a hallmark of eczema but is less prominent in SDRIFE cases.
Furthermore, while both psoriasis and Baboon Syndrome involve red patches on the skin, psoriasis usually presents with silvery scales. Understanding these distinctions aids healthcare professionals in providing appropriate treatment and managing patient expectations effectively.
Baboon Syndrome vs. Other Dermatoses: How to Differentiate
Baboon Syndrome can be easily confused with other dermatoses due to its distinct characteristics. It primarily manifests as symmetrical, red patches in intertriginous areas—those skin folds where friction occurs. This differentiates it from conditions like psoriasis or eczema that may have more varied presentations.
To distinguish Baboon Syndrome from allergic contact dermatitis, consider the patient’s medication history. SDRIFE typically arises after exposure to specific drugs rather than environmental irritants.
Clinicians often rely on histopathological examination for accurate diagnosis. The unique features observed in biopsy samples help rule out similar skin conditions and confirm the presence of Baboon Syndrome, guiding appropriate management strategies effectively.
Connection Between Stress and Baboon Syndrome
Stress has long been recognized as a significant factor in various skin conditions. Research indicates that psychological stress may play a role in triggering Baboon Syndrome.
When the body experiences stress, it releases certain hormones that can influence immune responses. This alteration may make individuals more susceptible to adverse reactions from medications, leading to symptoms associated with SDRIFE.
Moreover, those already dealing with chronic stress might find their skin condition exacerbated by the additional emotional strain. Understanding this connection is crucial for effective management and treatment of Baboon Syndrome while addressing underlying stress factors can promote overall well-being.
Outcome and Drug Triggers for SDRIFE
The outcome of SDRIFE largely depends on the identification and discontinuation of the triggering drug. Typically, symptoms resolve within days to weeks once exposure ceases. However, in some cases, residual pigmentation may persist long after the rash has healed.
Common drug triggers include antibiotics like penicillin and sulfonamides, as well as other medications such as non-steroidal anti-inflammatory drugs (NSAIDs). Recognition of these culprits is crucial for effective management.
Additionally, individual responses can vary significantly. What causes an outbreak in one person might not affect another similarly. Therefore, understanding personal medication history plays a vital role in preventing future occurrences of this dermatitis-like condition.
Importance of Recognizing and Addressing Baboon Syndrome
Recognizing Baboon Syndrome is crucial for effective patient care. This skin condition can occur in individuals with a history of certain drug exposures. Early identification helps prevent complications.
Addressing the syndrome promptly aids in alleviating distress and discomfort for affected individuals. Symptoms like itching and inflammation may significantly affect quality of life. By understanding its manifestations, healthcare providers can offer timely intervention.
Moreover, acknowledging Baboon Syndrome allows for better communication between patients and doctors regarding medication history. Increased awareness within the medical community ensures that this condition is not overlooked during diagnosis, leading to more accurate treatment plans tailored to individual needs.
Treatment Options for Baboon Syndrome
Treatment for Baboon Syndrome primarily focuses on identifying and removing the trigger drug. This is crucial, as continuing exposure can worsen symptoms or lead to complications. Once the offending medication is discontinued, patients often experience significant improvement in their condition.
Topical corticosteroids are commonly prescribed to reduce inflammation and alleviate discomfort associated with symmetrical drug-related intertriginous and flexural exanthema (SDRIFE). These medications help soothe affected areas while promoting healing of the skin.
In more severe cases, systemic treatments such as antihistamines may be recommended to control itching and allergic reactions. Supportive care, including proper skin hygiene and emollients, plays a vital role in managing symptoms effectively.
Key Summary and Conclusion
Baboon Syndrome, also known as symmetrical drug-related intertriginous and flexural exanthema (SDRIFE), highlights the importance of understanding drug reactions. This unique dermatological condition primarily manifests in areas like the groin and underarms, presenting with red, inflamed patches. Recognizing its clinical features is crucial for timely diagnosis.
The etiology often links to specific medications, emphasizing the need for awareness among healthcare providers and patients alike. The pathophysiology remains complex but involves immune-mediated mechanisms triggered by drugs.
Complications can arise if left untreated, including secondary infections or further skin irritation. Differentiating Baboon Syndrome from other dermatoses requires careful assessment of symptoms and history.
Recognizing Baboon Syndrome not only alerts medical professionals to potential adverse drug reactions but also guides treatment options effectively. Awareness leads to better outcomes for those affected by this unusual yet significant condition.


